LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
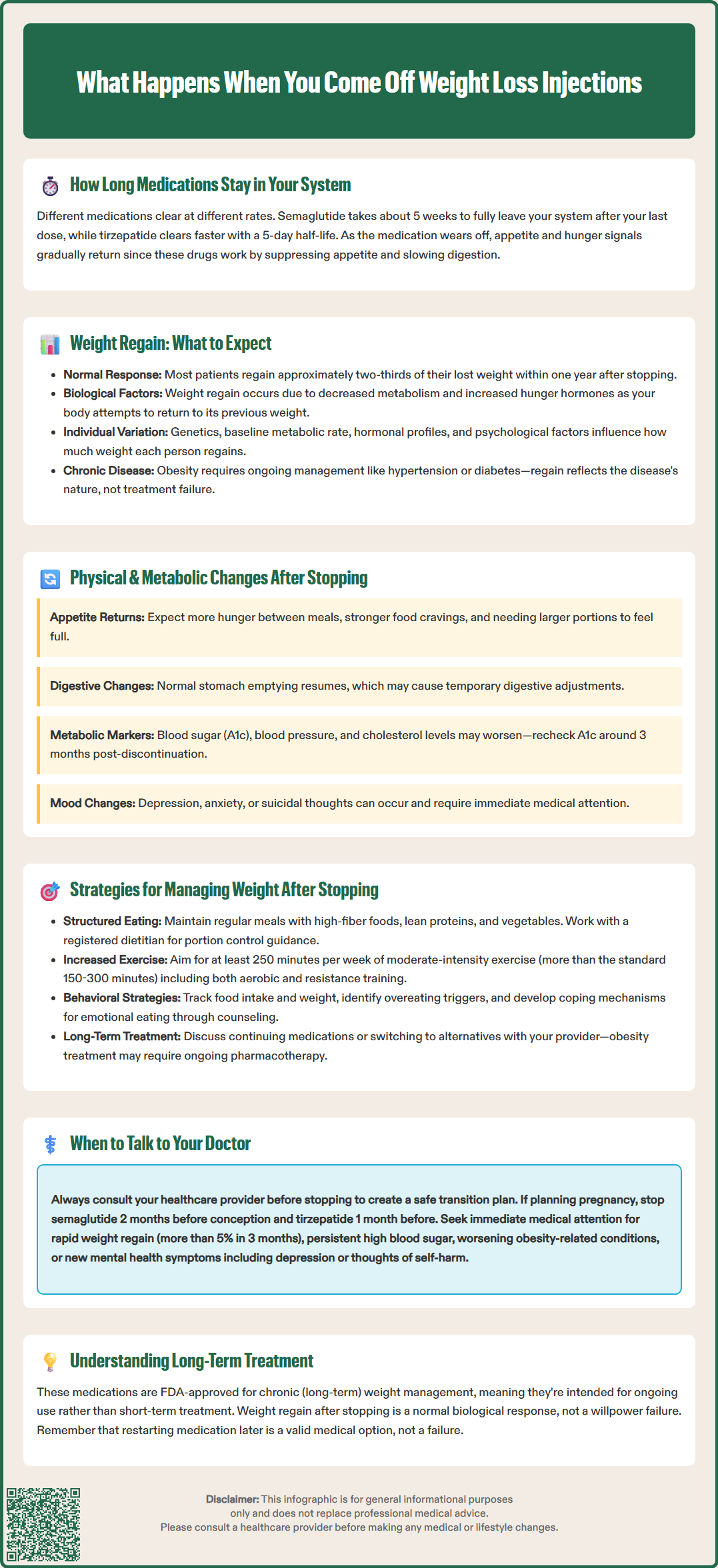
When you stop taking weight loss injections like semaglutide (Wegovy) or tirzepatide (Zepbound), your body undergoes significant physiological changes as the medication's effects gradually diminish. Most patients experience returning appetite, metabolic shifts, and weight regain—typically two-thirds of lost weight within one year. Understanding what happens when you come off weight loss injections helps you prepare for these changes and develop strategies to maintain your progress. This article examines the biological mechanisms behind discontinuation effects, expected timelines, and evidence-based approaches to managing your weight after stopping treatment.
Quick Answer: When you stop weight loss injections, most patients regain approximately two-thirds of their lost weight within one year as appetite returns and metabolic adaptations reverse.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
When you discontinue weight loss medications such as semaglutide (Wegovy) or tirzepatide (Zepbound), your body gradually transitions away from the pharmacological effects of these drugs. Semaglutide is a GLP-1 receptor agonist that mimics the naturally occurring hormone glucagon-like peptide-1, while tirzepatide is a dual GIP/GLP-1 receptor agonist that acts on two incretin hormone pathways. Both medications regulate appetite, slow gastric emptying, and influence insulin secretion.
The timeline for these changes depends on each medication's specific half-life. Semaglutide has a half-life of approximately one week, taking about 5 weeks to be substantially eliminated from your system. Tirzepatide has a shorter half-life of about 5 days. During this washout period, you may notice a gradual return of appetite and changes in satiety signals that were previously suppressed.
Many patients experience a resurgence of hunger cues and food-related thoughts that had been diminished during treatment. The physiological mechanisms that contributed to weight regulation before starting medication—including hormonal signals, proposed metabolic set points, and appetite regulation—typically reassert themselves. This is not a failure of willpower but rather a predictable biological response to the removal of pharmacological intervention.
It's important to note that Wegovy (semaglutide 2.4 mg) and Zepbound (tirzepatide) are FDA-approved for chronic weight management, while Ozempic (semaglutide) and Mounjaro (tirzepatide) are approved for type 2 diabetes management, though sometimes used off-label for weight loss.
If you're planning pregnancy, FDA guidance recommends discontinuing semaglutide approximately 2 months before a planned pregnancy and tirzepatide about 1 month before conception due to potential fetal risks.
Research evidence indicates that most patients regain a significant portion of their lost weight after discontinuing incretin-based weight loss medications. The STEP 1 extension study found that participants who stopped semaglutide regained approximately two-thirds of their previously lost weight within one year. The STEP 4 trial, which specifically examined continuation versus withdrawal of semaglutide, confirmed substantial weight regain in the discontinuation group. Similar patterns have been observed with liraglutide in the SCALE trials and tirzepatide in the SURMOUNT-4 study, suggesting this is a consistent finding across multiple incretin-based anti-obesity agents.
Several factors influence the degree of weight regain after discontinuation:
Biological factors: Your body's metabolic adaptation during weight loss includes decreased energy expenditure and increased hunger hormones (such as ghrelin), which persist after stopping medication. These adaptations represent your body's attempt to return to its previous weight.
Duration of treatment: Longer treatment periods may allow for better establishment of behavioral changes, though this doesn't prevent biological drivers of weight regain.
Lifestyle modifications: Patients who successfully implement and maintain dietary changes, physical activity routines, and behavioral strategies during treatment tend to experience less dramatic weight regain, though some regain typically still occurs.
Individual variability: Genetic factors, baseline metabolic rate, hormonal profiles, and psychological factors all contribute to individual differences in post-discontinuation weight trajectories.
It's important to recognize that this weight regain pattern reflects the chronic nature of obesity as a disease rather than treatment failure. The American Medical Association, American Diabetes Association, and other medical organizations recognize obesity as a chronic condition requiring ongoing management, similar to hypertension or diabetes. Discontinuing effective pharmacotherapy predictably results in disease recurrence, just as stopping blood pressure medications typically leads to elevated blood pressure returning.
Beyond weight regain, stopping GLP-1 and GIP/GLP-1 medications triggers several physiological changes that patients should anticipate. Understanding these changes helps distinguish normal responses from concerning symptoms requiring medical attention.
Appetite and satiety changes: The most immediate and noticeable change is typically increased appetite. Patients often report feeling hungrier between meals, experiencing more frequent food cravings, and requiring larger portions to feel satisfied. These changes usually begin as medication levels decline, with timing varying based on the drug's half-life. The sensation of early fullness that many patients appreciated during treatment diminishes, and pre-treatment eating patterns may reassert themselves.
Gastrointestinal function: During treatment, these medications slow gastric emptying, which contributes to prolonged satiety. After discontinuation, normal gastric motility returns, which may initially feel like food moves through your system more quickly. Some patients report temporary digestive changes during this transition period, though these typically resolve as the body readjusts.
Metabolic parameters: For patients who also had improvements in blood glucose control, hemoglobin A1c levels may rise after stopping treatment. Blood pressure and lipid profiles that improved during weight loss may also deteriorate as weight returns. Regular monitoring is recommended, with A1c rechecked approximately 3 months after discontinuation for patients with diabetes.
Mental health considerations: Some patients report changes in mood after discontinuation. The FDA prescribing information for Wegovy includes a warning about suicidal thoughts and behaviors, though a causal relationship has not been established. Any new or worsening depression, anxiety, or thoughts of self-harm warrant immediate discussion with your healthcare provider. Monitor for mood changes and seek prompt evaluation if concerning symptoms develop.
While some weight regain is common after discontinuing weight loss medications, proactive strategies can help minimize the extent of regain and support long-term weight management. A comprehensive approach addresses multiple aspects of weight regulation.
Nutritional strategies: Focus on maintaining a structured eating pattern with regular meals and planned snacks to manage returning hunger signals. Emphasize high-fiber foods, lean proteins, and vegetables that promote satiety. Consider working with a registered dietitian to develop a sustainable eating plan that accounts for your increased appetite while maintaining a modest caloric deficit or maintenance level. Portion control becomes particularly important as natural satiety signals change.
Physical activity: Regular exercise plays a crucial role in weight maintenance after medication discontinuation. The American College of Sports Medicine and U.S. Department of Health and Human Services recommend at least 250 minutes per week of moderate-intensity activity for weight loss maintenance (beyond the 150-300 minutes weekly recommended for general health). Both aerobic exercise and resistance training help preserve lean muscle mass, support metabolic rate, and contribute to energy balance. Find activities you enjoy to enhance long-term adherence.
Behavioral approaches: Cognitive-behavioral strategies can help manage the psychological aspects of weight maintenance. These include self-monitoring (tracking food intake, weight, and activity), identifying and managing triggers for overeating, developing coping strategies for emotional eating, and building a supportive environment. Many patients benefit from ongoing behavioral counseling or participation in structured weight management programs.
Medical options: Discuss with your healthcare provider whether continuing or transitioning to alternative weight management medications is appropriate for your situation. FDA-approved medications for chronic weight management include orlistat, phentermine/topiramate ER, naltrexone/bupropion ER, liraglutide 3 mg, semaglutide 2.4 mg, and tirzepatide. For some patients, obesity pharmacotherapy may be a long-term treatment rather than a time-limited intervention. Bariatric surgery may be considered for those with BMI ≥40 kg/m² or ≥35 kg/m² with obesity-related complications (with recent guidelines supporting consideration at lower BMI thresholds with metabolic disease). Consider referral to an obesity medicine specialist certified by the American Board of Obesity Medicine.
The decision to discontinue weight loss injections should ideally be made collaboratively with your healthcare provider rather than independently. Several scenarios warrant medical consultation before, during, or after stopping treatment.
Before stopping: Schedule a discussion with your doctor if you're considering discontinuation for any reason—whether due to side effects, cost concerns, achievement of weight goals, or other factors. Your provider can help assess whether stopping is appropriate, discuss alternative options, and develop a transition plan. For patients with diabetes, stopping may require adjustments to other glucose-lowering medications to maintain glycemic control.
Planned discontinuation: If you and your provider decide to stop treatment, discuss strategies for monitoring and managing potential weight regain. Establish a follow-up schedule to track weight, metabolic parameters, and overall health. Some providers recommend a gradual dose reduction rather than abrupt cessation, though evidence supporting this approach is limited.
Pregnancy planning: If you're planning pregnancy, discuss discontinuation timing with your provider. FDA guidance recommends stopping semaglutide approximately 2 months before planned conception and tirzepatide about 1 month before conception. Effective contraception should be used during dose adjustments and the washout period.
Concerning symptoms after stopping: Contact your healthcare provider if you experience:
Significant weight regain (more than 5% of body weight within 3 months or 2-3 pounds per week for several consecutive weeks)
For patients with diabetes: persistent fasting glucose >180 mg/dL, random glucose >250 mg/dL, or symptoms of hyperglycemia
Worsening of obesity-related comorbidities (sleep apnea, joint pain, hypertension)
New or worsening depression, anxiety, or thoughts of self-harm
Difficulty managing appetite or eating behaviors
Long-term follow-up: Maintain regular contact with your healthcare team after discontinuation. Obesity is a chronic disease, and ongoing medical supervision supports better long-term outcomes. Your provider can help determine if and when resuming medication might be appropriate, or whether alternative interventions should be considered. Remember that restarting treatment after a period off medication is a reasonable medical decision, not a personal failure.
Semaglutide has a half-life of approximately one week and takes about 5 weeks to be substantially eliminated from your system. Tirzepatide has a shorter half-life of about 5 days, clearing more quickly from the body.
Clinical trials show that most patients regain approximately two-thirds of their lost weight within one year after stopping treatment. The amount of regain varies individually and can be influenced by lifestyle modifications, though some regain typically occurs due to biological factors.
Yes, restarting weight loss medications after discontinuation is a reasonable medical decision that should be discussed with your healthcare provider. Obesity is recognized as a chronic condition that may require ongoing or intermittent pharmacological management.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.