LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does GLP-1 make you pee a lot? This common question arises among patients starting glucagon-like peptide-1 (GLP-1) receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound). While frequent urination is not listed as a direct side effect in FDA prescribing information, some patients report changes in urinary patterns. Understanding the relationship between these medications and urination involves examining both their mechanism of action and indirect factors like weight loss, improved blood sugar control, and hydration changes. This article explores the evidence behind urinary symptoms on GLP-1 therapy and when to seek medical evaluation.
Quick Answer: GLP-1 receptor agonists do not directly cause frequent urination as a pharmacological effect, though some patients may experience urinary changes due to indirect factors like weight loss, improved glycemic control, or hydration changes.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications originally developed for type 2 diabetes management, with some now approved for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) works similarly but is technically a dual GIP/GLP-1 receptor agonist rather than a pure GLP-1 medication.
These incretin-based therapies work by mimicking naturally occurring hormones released by the intestines after eating. They bind to receptors found in multiple organs, including the pancreas, brain, stomach, and cardiovascular system. In the pancreas, these drugs stimulate insulin secretion in a glucose-dependent manner, meaning they promote insulin release only when blood sugar levels are elevated. This mechanism significantly reduces the risk of hypoglycemia when used alone, though this risk increases when combined with insulin or sulfonylureas.
Additionally, these medications slow gastric emptying, which prolongs the feeling of fullness after meals and reduces appetite through central nervous system pathways. They also suppress glucagon secretion, a hormone that raises blood sugar levels. The combined effects lead to improved glycemic control in people with type 2 diabetes and substantial weight loss in appropriate patients.
The FDA has approved specific formulations for different indications: semaglutide 2.4 mg (Wegovy), liraglutide 3 mg (Saxenda), and tirzepatide (Zepbound) are approved for chronic weight management, while all are approved for diabetes at different doses. Some of these medications (liraglutide, semaglutide, and dulaglutide) have demonstrated cardiovascular benefits in clinical trials, with Wegovy specifically approved for reducing cardiovascular risk in adults with established cardiovascular disease and either obesity or overweight. Understanding these fundamental mechanisms provides context for evaluating their potential effects on urinary function and fluid balance.
Frequent urination is not listed as a common adverse effect in the FDA-approved prescribing information for GLP-1 receptor agonists or tirzepatide. The most frequently reported side effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, constipation, and abdominal pain. These occur in a significant proportion of patients, particularly during dose escalation. However, there is no official direct link between these medications and increased urinary frequency as a pharmacological effect of the drug class.
It is important to note that severe gastrointestinal side effects can lead to dehydration, which may affect kidney function. FDA prescribing information for these medications includes warnings about the risk of acute kidney injury in patients who experience severe adverse gastrointestinal reactions.
That said, some patients report subjective increases in urination after starting therapy. These reports appear anecdotal rather than supported by robust clinical evidence. When urinary changes do occur, they are more likely related to indirect factors associated with the medication's primary effects rather than a direct pharmacological action on the urinary system.
If you are experiencing increased urination while taking a GLP-1 medication, several factors unrelated to the drug's direct mechanism may be responsible, which warrants further evaluation to identify the underlying cause.
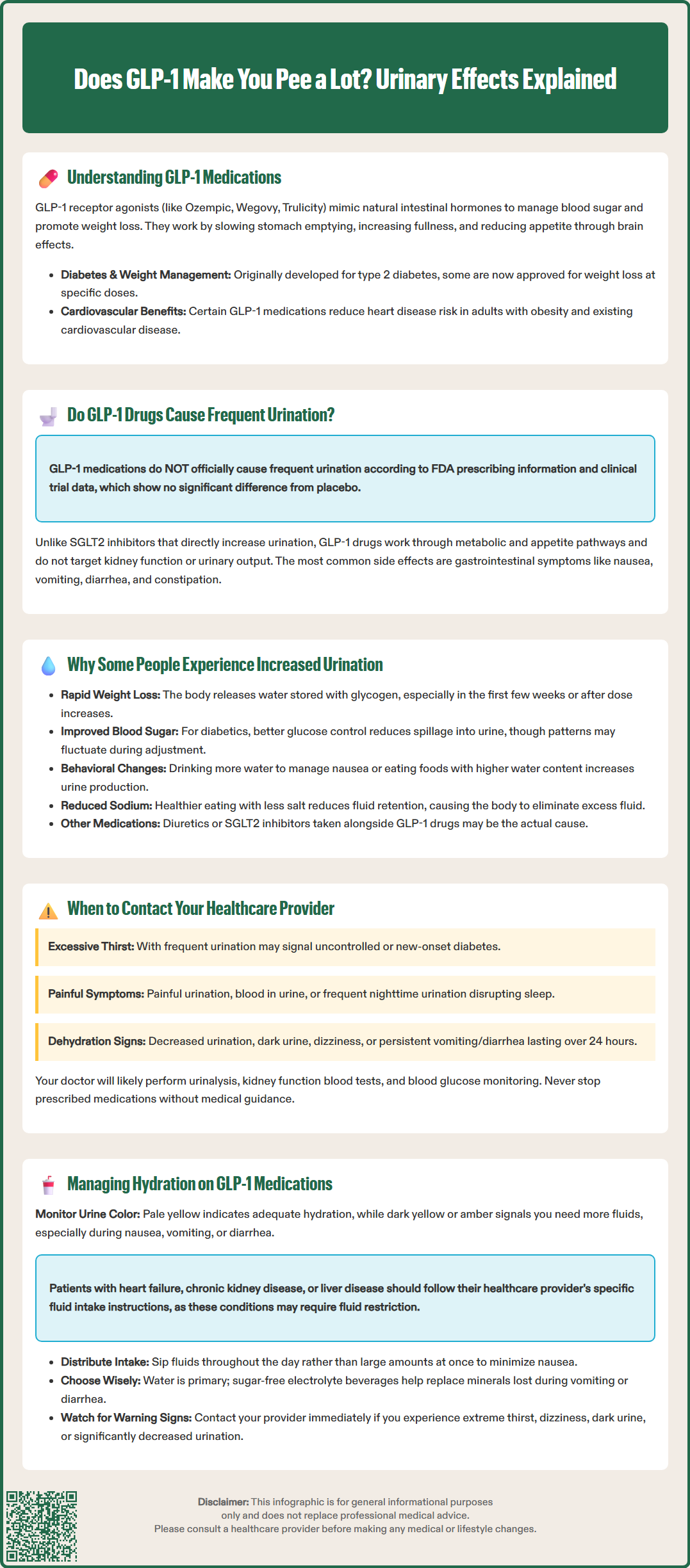
While GLP-1 medications do not directly cause frequent urination, several indirect mechanisms may explain why some individuals notice changes in their urinary patterns after starting treatment. Understanding these factors can help differentiate between expected physiological changes and symptoms requiring medical attention.
Weight Loss and Fluid Shifts: GLP-1 medications typically produce significant weight loss, particularly in the initial months of treatment. Rapid weight reduction may involve mobilization of glycogen stores and associated water weight. As the body metabolizes stored glycogen, bound water is released and excreted through the kidneys, potentially increasing urine output temporarily. This phenomenon might be noticeable in the first few weeks of treatment or after dose increases, though this mechanism has not been specifically studied in GLP-1 clinical trials.
Improved Glycemic Control: For patients with type 2 diabetes, GLP-1 therapy often substantially improves blood glucose levels. When blood sugar was previously elevated, excess glucose spills into the urine (glucosuria), causing osmotic diuresis and increased urination. As glycemic control improves and glucose levels normalize, this effect should actually decrease. However, the transition period may involve fluctuating urinary patterns as metabolic balance is restored.
Dietary and Hydration Changes: Many patients modify their eating and drinking habits when starting GLP-1 therapy. Some increase water intake in response to nausea or to support weight loss efforts. Others consume more low-calorie beverages or foods with higher water content. These behavioral changes can naturally increase urine production. Additionally, reduced sodium intake associated with healthier eating patterns may decrease fluid retention, leading to increased urination as excess fluid is eliminated.
Concurrent Medications: Patients taking GLP-1 drugs often use other medications that affect fluid balance, including diuretics for hypertension or SGLT2 inhibitors for diabetes. The combination of medications may have additive effects on urinary frequency that are incorrectly attributed solely to the GLP-1 agent.
While mild increases in urination may be benign and self-limiting, certain urinary symptoms warrant prompt medical evaluation. Recognizing warning signs helps ensure timely diagnosis and management of potentially serious conditions.
Contact your healthcare provider if you experience:
Excessive thirst with frequent urination: This combination may indicate inadequately controlled diabetes or, rarely, new-onset diabetes. Persistent hyperglycemia requires assessment and possible medication adjustment.
Painful urination or urgency: Dysuria, urgency, or suprapubic discomfort suggests urinary tract infection, which requires antibiotic treatment. Women and individuals with diabetes have increased UTI risk.
Blood in urine: Hematuria always requires investigation to exclude infection, kidney stones, or more serious urological conditions.
Nocturia disrupting sleep: Waking multiple times nightly to urinate may indicate uncontrolled diabetes, heart failure, sleep apnea, or prostate issues in men. This symptom significantly impacts quality of life and deserves evaluation.
Decreased urination or dark urine: Oliguria or concentrated urine may signal dehydration, particularly if accompanied by persistent nausea, vomiting, or diarrhea—common side effects of GLP-1 medications. Severe dehydration can lead to acute kidney injury, which is specifically mentioned in FDA warnings for these medications.
Dizziness or lightheadedness: Orthostatic symptoms combined with urinary changes may indicate volume depletion requiring fluid management adjustment.
Persistent vomiting or diarrhea: Seek urgent care if unable to maintain hydration or if severe gastrointestinal symptoms persist for more than 24 hours.
Your provider will likely perform a urinalysis, assess kidney function through blood tests (creatinine, estimated glomerular filtration rate), and evaluate blood glucose control with hemoglobin A1c or glucose monitoring. For people with diabetes, the American Diabetes Association recommends checking both eGFR and urine albumin-to-creatinine ratio at least annually, or more frequently with existing kidney disease. Your provider may adjust your medication dose, modify concurrent medications, or investigate alternative diagnoses. Never discontinue prescribed medications without medical guidance, as abrupt cessation may worsen glycemic control or cause weight regain.
Maintaining appropriate hydration is essential for patients taking GLP-1 medications, particularly given the common gastrointestinal side effects that can affect fluid balance. Implementing practical strategies helps optimize treatment outcomes while minimizing complications.
Hydration Guidelines: Aim for adequate daily fluid intake based on your individual needs, which vary depending on body size, activity level, climate, and health conditions. Rather than following a fixed rule, monitor urine color as a practical hydration indicator—pale yellow suggests adequate hydration, while dark yellow or amber indicates insufficient fluid intake. During periods of nausea, vomiting, or diarrhea, consciously increase fluid consumption to compensate for losses, unless you have been advised to restrict fluids.
Important Note: If you have heart failure, chronic kidney disease, or liver disease, follow your healthcare provider's specific guidance on fluid intake, as these conditions may require fluid restriction rather than increased consumption.
Timing Strategies: Distribute fluid intake throughout the day rather than consuming large volumes at once, which may exacerbate nausea or gastric discomfort. If nocturia is problematic, reduce fluid intake 2-3 hours before bedtime while ensuring adequate daytime hydration. Sip fluids slowly, particularly if experiencing nausea, as small frequent amounts are often better tolerated than large volumes.
Beverage Selection: Water remains the optimal choice for hydration. While caffeinated beverages have mild diuretic properties, moderate consumption contributes to overall hydration. Avoid excessive alcohol consumption, which impairs hydration status and may affect blood sugar control. Sugar-free electrolyte beverages can be beneficial during episodes of vomiting or diarrhea to replace lost minerals.
Monitoring and Adjustment: Track your weight regularly, as unexpected rapid weight changes may indicate fluid shifts. Report persistent gastrointestinal symptoms to your healthcare provider, as antiemetic medications or dose adjustments may improve tolerability. Contact your provider promptly if you develop signs of dehydration such as extreme thirst, dizziness, dark urine, or significantly decreased urination.
By understanding the relationship between GLP-1 medications and urinary patterns, patients can distinguish normal physiological responses from symptoms requiring medical attention, ensuring safe and effective treatment.
No, frequent urination is not listed as a common side effect in FDA prescribing information for GLP-1 receptor agonists. The most common side effects are gastrointestinal symptoms like nausea, vomiting, and diarrhea.
Increased urination may occur indirectly due to weight loss with fluid shifts, improved blood sugar control reducing glucose-related urination, increased water intake, or dietary changes. These are not direct pharmacological effects of the medication.
Contact your healthcare provider if you experience excessive thirst with frequent urination, painful urination, blood in urine, decreased urination with dark urine, dizziness, or persistent vomiting or diarrhea that may cause dehydration.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.