LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Do weight loss injections cause constipation? This common concern affects many patients considering or currently using GLP-1 receptor agonists like semaglutide (Wegovy) and tirzepatide (Zepbound). Clinical trials show that constipation occurs in approximately 6-24% of patients taking these medications, making it a recognized side effect. Understanding why this happens—primarily through slowed gastrointestinal motility and delayed gastric emptying—helps patients and healthcare providers implement effective prevention and management strategies. This article examines the mechanisms behind constipation with weight loss injections, evidence-based management approaches, and when to seek medical attention.
Quick Answer: Yes, weight loss injections can cause constipation, affecting approximately 6-24% of patients taking GLP-1 receptor agonists like semaglutide and tirzepatide.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and tirzepatide (Zepbound), work through multiple mechanisms to promote weight reduction. These medications mimic naturally occurring hormones that regulate appetite and glucose metabolism.
GLP-1 receptor agonists bind to GLP-1 receptors in the brain, particularly in areas controlling appetite and satiety. This action reduces hunger signals and increases feelings of fullness after eating smaller portions. Additionally, these medications slow gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed emptying contributes to prolonged satiety and reduced caloric intake.
Beyond appetite regulation, GLP-1 medications enhance insulin secretion in response to meals while suppressing glucagon release, improving overall glycemic control. Tirzepatide offers dual action by also activating glucose-dependent insulinotropic polypeptide (GIP) receptors, potentially enhancing weight loss effects. The FDA has approved Wegovy (semaglutide 2.4 mg) and Zepbound (tirzepatide) for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, when used with a reduced-calorie diet and increased physical activity. Similar medications like Ozempic and Mounjaro are FDA-approved for type 2 diabetes, not weight management.
Clinical trials demonstrate significant weight reduction, with patients losing approximately 15% of body weight over 68 weeks with semaglutide (STEP 1 trial) and up to 21% with tirzepatide 15 mg over 72 weeks (SURMOUNT-1 trial). These medications are typically started at low doses and gradually increased to reduce side effects. However, the same mechanisms that slow gastric emptying and alter gastrointestinal motility can lead to digestive side effects, including constipation, which affects a notable proportion of users.
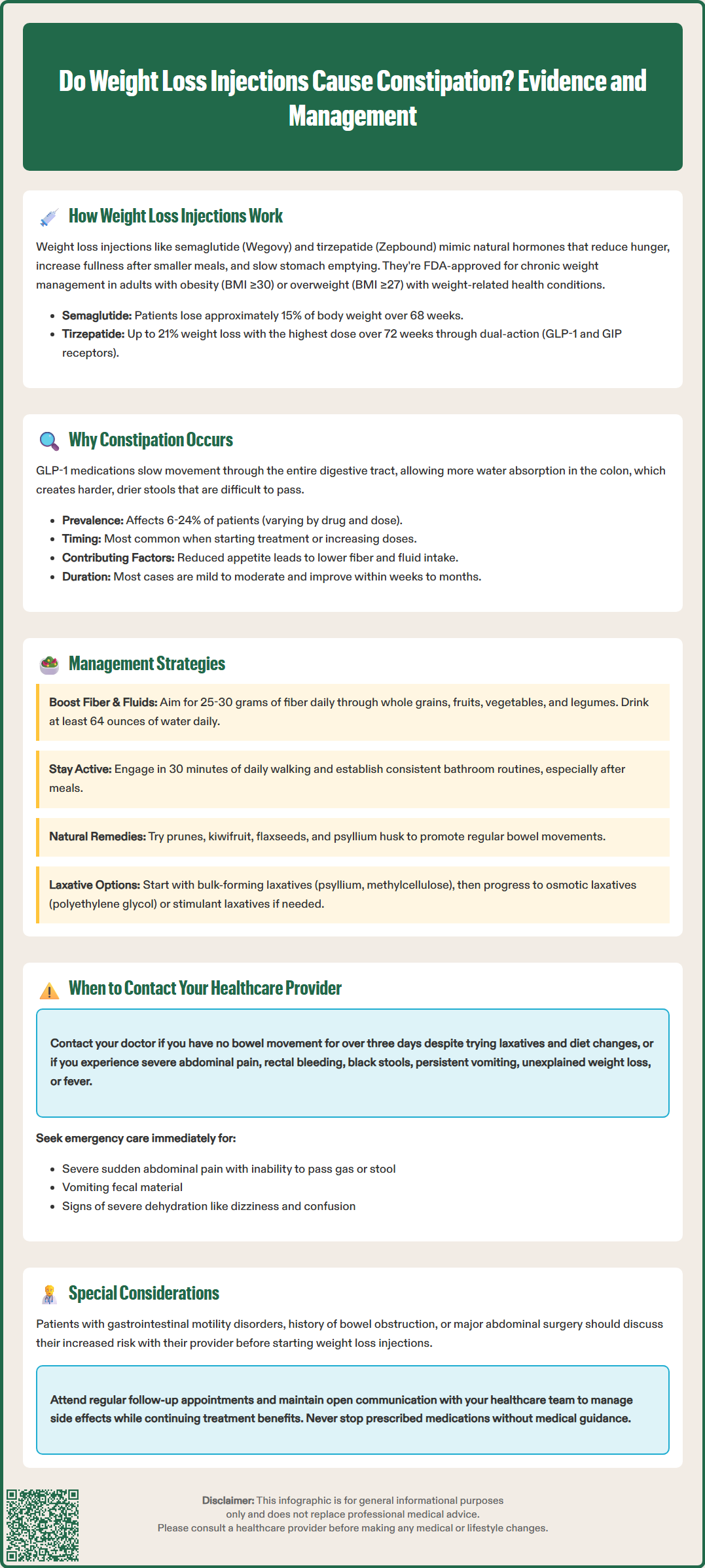
Constipation—defined as having fewer than three bowel movements per week, hard or dry stools, or difficulty or pain with passage of stool—is a recognized adverse effect of GLP-1 receptor agonists, though it occurs less frequently than nausea or diarrhea. Understanding the physiological basis helps patients and clinicians anticipate and manage this side effect effectively.
The primary mechanism involves delayed gastric emptying and reduced gastrointestinal motility throughout the digestive tract. GLP-1 receptors are present not only in the stomach but also in the intestines. When activated, these receptors slow the movement of contents through the entire gastrointestinal system. This prolonged transit time allows more water absorption from stool in the colon, resulting in harder, drier stools that are difficult to pass.
Clinical trial data from the STEP trials for semaglutide reported constipation in approximately 11-24% of participants, depending on the dose, compared to 11% in placebo groups. With tirzepatide, constipation rates ranged from 6-11% across different dosing groups in the SURMOUNT trials. These rates establish a clear association between GLP-1 medications and constipation risk. Constipation is typically more common during dose initiation and escalation periods.
Additional contributing factors include reduced food and fluid intake. As appetite decreases, patients naturally consume less, including dietary fiber and fluids—both essential for normal bowel function. The combination of pharmacological effects on gut motility and behavioral changes in eating patterns creates a multifactorial risk for constipation.
Most cases of constipation are mild to moderate and tend to improve as the body adjusts to the medication, typically within the first few weeks to months of treatment. However, persistent or severe constipation requires clinical attention, as rare cases of ileus (intestinal obstruction) have been reported with these medications.
Effective management of constipation during GLP-1 therapy involves both preventive strategies and therapeutic interventions. Proactive measures can significantly reduce the incidence and severity of this side effect.
Dietary modifications form the foundation of constipation management:
Increase fiber intake: Aim for 25-30 grams daily through whole grains, fruits, vegetables, and legumes. Focus on soluble fiber (like psyllium) and introduce fiber gradually to avoid bloating.
Maintain adequate hydration: Consume at least 64 ounces (8 cups) of water daily, adjusting for activity level and climate. Note: Patients with heart failure or kidney disease should follow their provider's fluid intake recommendations.
Include natural laxative foods: Prunes, kiwifruit, flaxseeds, and psyllium husk can promote regular bowel movements.
Avoid excessive processed foods: These often lack fiber and can worsen constipation.
Lifestyle interventions complement dietary changes:
Regular physical activity: Even moderate exercise like walking 30 minutes daily stimulates intestinal motility.
Establish routine: Attempt bowel movements at consistent times, particularly after meals when the gastrocolic reflex is strongest.
Respond to urges promptly: Delaying defecation can worsen constipation.
Pharmacological options may be necessary when lifestyle measures prove insufficient:
Bulk-forming laxatives (psyllium, methylcellulose): First-line agents that increase stool mass.
Osmotic laxatives (polyethylene glycol, lactulose): Draw water into the colon to soften stools.
Stool softeners (docusate): May help but have limited evidence for efficacy.
Stimulant laxatives (bisacodyl, senna): Can be used intermittently or for maintenance under healthcare guidance.
Rectal therapies (glycerin suppositories, saline enemas): Useful as rescue options for immediate relief.
Consult your healthcare provider before starting any laxative regimen, especially if taking other medications. Review all medications with your provider, as some (like opioids, iron supplements, or certain antidepressants) can worsen constipation. Some patients may benefit from slower dose escalation or temporary dose reduction of their GLP-1 medication if constipation becomes problematic, though this should only occur under medical supervision.
While mild constipation is manageable with self-care measures, certain symptoms warrant prompt medical evaluation. Recognizing warning signs ensures timely intervention and prevents serious complications.
Contact your healthcare provider if you experience:
Severe abdominal pain or distention: May indicate bowel obstruction or other serious conditions.
No bowel movement for more than three days despite using laxatives and dietary modifications.
Rectal bleeding or black, tarry stools: Could signal gastrointestinal bleeding requiring urgent assessment.
Persistent nausea and vomiting: Especially if unable to keep down fluids, raising dehydration concerns.
Unintentional weight loss beyond expected: May suggest inadequate nutrition or underlying pathology.
Fever accompanying constipation: Could indicate infection or inflammatory process.
Seek emergency care immediately (call 911 or go to the nearest emergency department) for:
Severe, sudden abdominal pain with inability to pass gas or stool (possible obstruction)
Vomiting fecal-material or persistent bilious vomiting
Signs of severe dehydration (dizziness, decreased urination, confusion)
Your provider may need to perform a physical examination, review your medication regimen, and potentially order investigations such as abdominal imaging if complications are suspected. Consider holding your next dose and contacting your prescriber if you experience severe or persistent gastrointestinal symptoms.
Patients with severe gastrointestinal motility disorders (such as gastroparesis), history of bowel obstruction, or significant abdominal surgical history should discuss their potential increased risk with their provider before starting weight loss injections. These individuals may require closer monitoring and more aggressive preventive strategies.
Regular follow-up appointments allow for ongoing assessment of side effects and treatment efficacy. Open communication with your healthcare team ensures that constipation and other adverse effects are managed appropriately while maintaining the benefits of weight loss therapy. Never discontinue prescribed medications without medical guidance, as abrupt cessation may affect metabolic control and weight management progress.
Clinical trials show constipation occurs in approximately 11-24% of patients taking semaglutide and 6-11% taking tirzepatide, compared to 11% in placebo groups. Most cases are mild to moderate and improve as the body adjusts to the medication.
GLP-1 receptor agonists slow gastrointestinal motility throughout the digestive tract, prolonging transit time and allowing more water absorption from stool in the colon. This results in harder, drier stools that are difficult to pass.
Contact your healthcare provider if you experience severe abdominal pain, no bowel movement for more than three days despite using laxatives, rectal bleeding, persistent vomiting, or fever. Seek emergency care for severe sudden abdominal pain with inability to pass gas or stool.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.