LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

GLP-1 patches are marketed as needle-free alternatives to FDA-approved injectable medications like semaglutide and liraglutide, claiming to deliver weight loss and blood sugar control through the skin. However, no GLP-1 patch has received FDA approval, and scientific evidence supporting their effectiveness remains absent. Most commercially available patches contain herbal extracts or vitamins rather than pharmaceutical-grade GLP-1 receptor agonists. The large molecular size of GLP-1 peptides makes transdermal delivery highly implausible without advanced technology not present in consumer products. Understanding the distinction between proven GLP-1 medications and unregulated patch products is essential for safe, effective treatment.
Quick Answer: No, commercially available GLP-1 patches have not been proven effective and lack FDA approval for weight loss or diabetes management.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
GLP-1 patches are marketed as transdermal delivery systems that purportedly deliver glucagon-like peptide-1 (GLP-1) receptor agonists through the skin for weight loss and glycemic control. These products claim to offer a needle-free alternative to FDA-approved injectable GLP-1 medications like semaglutide and liraglutide. Manufacturers typically advertise these patches as convenient, pain-free options that continuously release medication over 24 hours.
The theoretical mechanism involves transdermal absorption of GLP-1 analogs or related compounds through the skin's stratum corneum into systemic circulation. Proponents claim these patches can suppress appetite, slow gastric emptying, and improve insulin secretion—effects associated with legitimate GLP-1 receptor agonists. However, there is no official link between these marketed patches and FDA-approved GLP-1 therapies.
As of 2024, most commercially available "GLP-1 patches" do not actually contain pharmaceutical-grade GLP-1 receptor agonists. Instead, they often include herbal extracts, vitamins, or other compounds claimed to "support" GLP-1 production or function. The scientific plausibility of delivering active GLP-1 peptides transdermally remains highly questionable, as these are large protein molecules (molecular weight >3,000 Da) that typically cannot penetrate intact skin in therapeutically meaningful amounts—well above the recognized 500 Da threshold for effective passive skin penetration.
Importantly, any patch claiming to contain actual semaglutide, liraglutide, or other GLP-1 receptor agonists would be an unapproved, potentially illegal drug product in the US. The FDA has not approved any transdermal patch delivery system for GLP-1 medications. Consumers should understand that marketing claims for these products often lack rigorous clinical validation. The distinction between evidence-based pharmaceutical GLP-1 medications and unregulated patch products is critical for patient safety and treatment efficacy.
The FDA has approved several GLP-1 receptor agonists for type 2 diabetes management and, in some cases, chronic weight management. These include semaglutide (Ozempic®, Wegovy®, Rybelsus®), liraglutide (Victoza®, Saxenda®), dulaglutide (Trulicity®), and tirzepatide (Mounjaro®, Zepbound®)—though tirzepatide is technically a dual GIP/GLP-1 receptor agonist. While exenatide (Byetta®, Bydureon®) was previously approved, these products have been discontinued in the US market.
Currently approved delivery methods include:
Subcutaneous injection: The most common route, using pre-filled pens for once-weekly (semaglutide, dulaglutide) or once-daily (liraglutide) administration
Oral tablets: Semaglutide (Rybelsus®) is the only FDA-approved oral GLP-1 medication, utilizing absorption-enhancing technology
No transdermal patch formulation has received FDA approval for GLP-1 delivery. The FDA approval process requires extensive Phase I-III clinical trials demonstrating safety, efficacy, pharmacokinetics, and quality manufacturing standards. Approved GLP-1 medications undergo rigorous bioavailability testing to ensure therapeutic drug levels reach systemic circulation.
These medications work by activating GLP-1 receptors in pancreatic beta cells, the brain, and gastrointestinal tract. This activation enhances glucose-dependent insulin secretion, suppresses inappropriate glucagon release, delays gastric emptying, and reduces appetite through central nervous system pathways. Common adverse effects include nausea, vomiting, diarrhea, and constipation. More serious risks include pancreatitis, gallbladder disease, acute kidney injury (particularly with dehydration), hypoglycemia (when combined with insulin or sulfonylureas), and thyroid C-cell tumors in animal studies. Semaglutide may worsen diabetic retinopathy in some patients with pre-existing disease.
Notably, Wegovy® (semaglutide 2.4 mg) now has an additional indication for cardiovascular risk reduction in adults with established cardiovascular disease and either overweight or obesity.
Patients should only use GLP-1 medications prescribed by licensed healthcare providers and obtained through legitimate pharmacies, ensuring product authenticity and appropriate medical supervision.
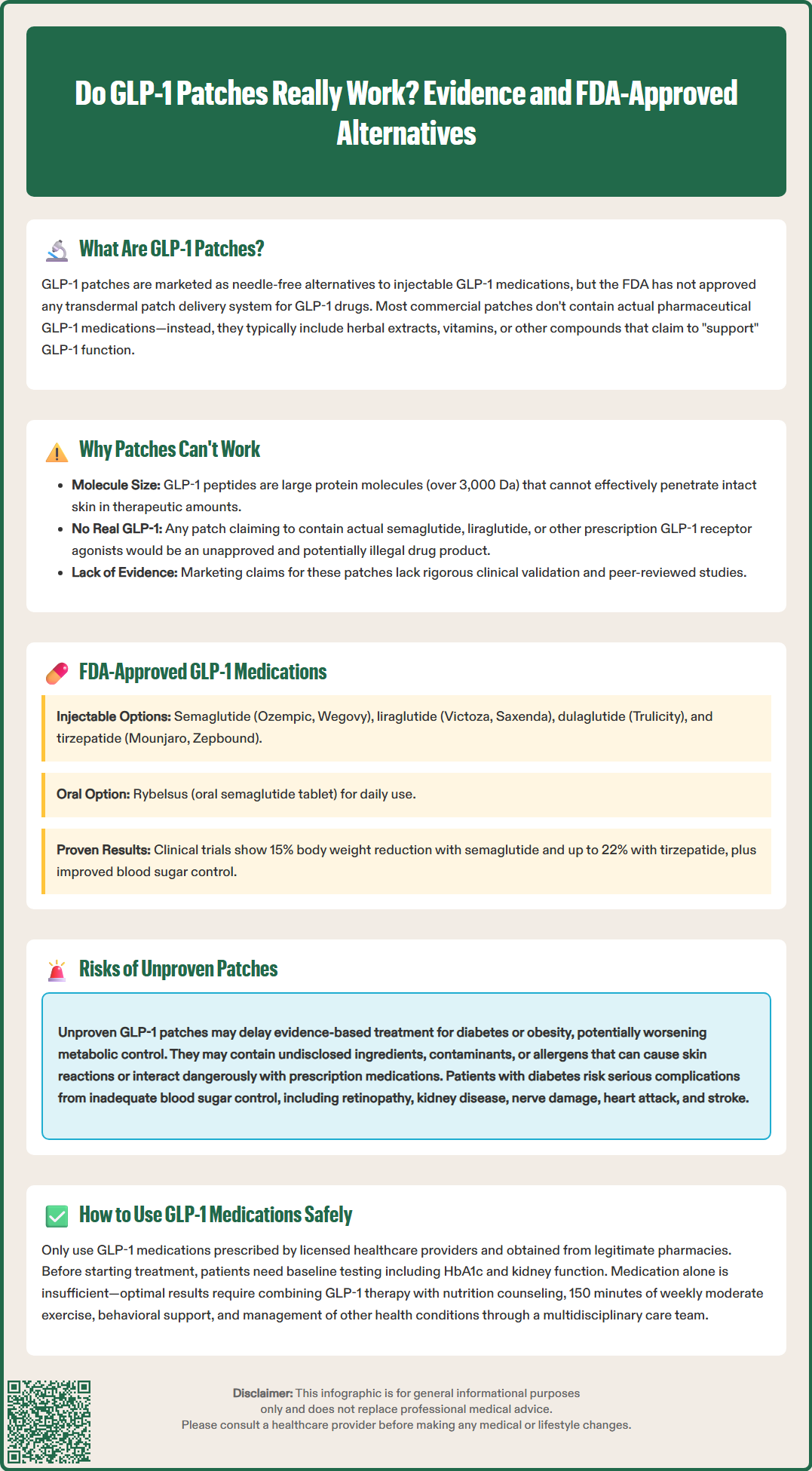
As of 2024, there is no peer-reviewed clinical evidence demonstrating that commercially available GLP-1 patches deliver therapeutic outcomes comparable to FDA-approved GLP-1 medications. A comprehensive literature search of PubMed, Cochrane Library, and ClinicalTrials.gov reveals no published randomized controlled trials evaluating over-the-counter GLP-1 patches for weight loss or diabetes management.
The fundamental challenge lies in transdermal delivery of large peptide molecules. GLP-1 receptor agonists are hydrophilic proteins with molecular weights exceeding 3,000 Daltons—far above the typical 500 Da threshold for effective passive skin penetration. The skin's stratum corneum serves as an effective barrier against such molecules. While pharmaceutical research explores advanced transdermal delivery systems using microneedles, iontophoresis, or chemical enhancers, these technologies remain experimental for GLP-1 delivery and are not present in consumer patch products.
Products marketed as "GLP-1 patches" typically contain botanical extracts, amino acids, or vitamins rather than actual GLP-1 receptor agonists. Manufacturers may claim these ingredients "stimulate natural GLP-1 production," but such assertions lack clinical validation. No evidence shows these products produce clinically meaningful metabolic effects or significant changes in endogenous GLP-1 levels.
Some research investigates transdermal delivery of small-molecule GLP-1 receptor agonists or modified peptides, but these remain in early development stages. No data support the efficacy of currently marketed patches. The absence of pharmacokinetic studies, dose-response relationships, or comparative effectiveness data represents a significant evidence gap.
Patients seeking GLP-1 therapy should rely on FDA-approved medications with established efficacy profiles, including landmark trials like STEP (semaglutide) demonstrating approximately 15% body weight reduction and SCALE (liraglutide) showing 5-8% weight reduction, along with improved glycemic control in patients with diabetes.
Using unproven GLP-1 patches carries several significant risks beyond simple ineffectiveness. These products are not FDA-approved drugs; if marketed as dietary supplements or cosmetics, they are regulated under different frameworks (Dietary Supplement Health and Education Act or cosmetics regulations) that do not require pre-market approval for safety and efficacy. This regulatory distinction creates substantial patient safety concerns.
Key risks include:
Delayed appropriate treatment: Patients with type 2 diabetes or obesity may postpone evidence-based interventions while using ineffective patches, potentially worsening metabolic control and increasing cardiovascular risk
Undisclosed ingredients: While supplement manufacturers must follow current Good Manufacturing Practices, quality control varies widely; products may contain contaminants, adulterants, or unlisted substances
Allergic reactions: Adhesive components and botanical extracts can cause contact dermatitis, skin irritation, or systemic allergic responses
Drug interactions: Herbal ingredients may interact with prescription medications, including anticoagulants, antihypertensives, or diabetes medications
False reassurance: Belief in patch efficacy may lead patients to neglect dietary modifications, physical activity, or medication adherence
The financial burden represents another limitation. These patches often cost $30-100 monthly without insurance coverage or proven benefit, diverting resources from effective interventions.
Red flags requiring medical attention include:
Severe or persistent hyperglycemia (blood glucose >300 mg/dL)
Symptoms of diabetic ketoacidosis or hyperosmolar hyperglycemic state
Severe abdominal pain (possible pancreatitis)
Right upper quadrant pain (possible gallbladder disease)
Signs of allergic reaction or severe skin reactions
Patients with diabetes should understand that inadequate glycemic control increases risks of microvascular complications (retinopathy, nephropathy, neuropathy) and macrovascular events (myocardial infarction, stroke). Similarly, obesity management requires evidence-based approaches; ineffective interventions delay meaningful health improvements.
Healthcare providers should counsel patients about these risks and redirect them toward proven therapies. The American Diabetes Association and American College of Physicians recommend individualized therapy; GLP-1 receptor agonists may be appropriate second-line agents after metformin or even first-line in patients with established cardiovascular disease, chronic kidney disease, or when weight management is a priority.
Adverse events from supplement products should be reported to the FDA through the MedWatch program.
Patients seeking GLP-1-based therapy have several evidence-based options available through prescription from licensed healthcare providers. The choice depends on individual clinical circumstances, including diabetes status, weight management goals, cardiovascular risk, renal function, and patient preferences regarding administration route and frequency.
FDA-approved injectable GLP-1 medications include:
Semaglutide (Ozempic® 0.5-2 mg weekly for diabetes; Wegovy® 2.4 mg weekly for weight management): Demonstrated 15-17% weight loss in STEP trials and significant cardiovascular benefits in SUSTAIN and SELECT trials
Liraglutide (Victoza® 1.8 mg daily for diabetes; Saxenda® 3 mg daily for weight management): Proven efficacy with 5-8% weight reduction and cardiovascular outcome benefits in the LEADER trial
Dulaglutide (Trulicity® 0.75-4.5 mg weekly): Convenient once-weekly dosing with demonstrated cardiovascular benefit in the REWIND trial
Tirzepatide (Mounjaro® for diabetes; Zepbound® for weight management): Dual GIP/GLP-1 agonist showing superior weight loss (up to 22%) in SURMOUNT trials
Oral option:
These medications require proper patient selection and monitoring. Contraindications include personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Common adverse effects—nausea, vomiting, diarrhea—typically diminish with gradual dose titration.
Patients should undergo baseline assessment including HbA1c and renal function. Monitoring includes periodic HbA1c measurement, weight tracking, assessment for adverse effects, and evaluation of diabetic retinopathy status (particularly with semaglutide). These medications should be avoided during pregnancy and breastfeeding. Patients taking insulin or sulfonylureas should be monitored for hypoglycemia risk.
Referral to endocrinology is appropriate for complex cases, inadequate response, or significant adverse effects.
Comprehensive obesity and diabetes management extends beyond pharmacotherapy, incorporating medical nutrition therapy, physical activity (150 minutes weekly of moderate-intensity exercise), behavioral counseling, and treatment of comorbidities. Multidisciplinary care involving physicians, dietitians, diabetes educators, and mental health professionals optimizes outcomes and addresses the complex pathophysiology of metabolic disease.
No, the FDA has not approved any transdermal patch for GLP-1 delivery. All FDA-approved GLP-1 medications are administered via subcutaneous injection or oral tablets, requiring prescription from licensed healthcare providers.
GLP-1 receptor agonists are large protein molecules exceeding 3,000 Daltons in molecular weight, far above the 500 Dalton threshold for effective passive skin penetration. The skin's barrier prevents these molecules from reaching therapeutic levels in the bloodstream without advanced delivery technology not present in consumer patches.
FDA-approved options include injectable semaglutide (Wegovy®), liraglutide (Saxenda®), tirzepatide (Zepbound®), and oral semaglutide (Rybelsus®). These medications have demonstrated significant weight loss (5-22%) and metabolic benefits in rigorous clinical trials when prescribed and monitored by healthcare providers.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.