LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does semaglutide cause pancreatitis? This question concerns many patients prescribed Ozempic, Wegovy, or Rybelsus for type 2 diabetes or weight management. Semaglutide is a GLP-1 receptor agonist that enhances insulin secretion and reduces appetite. While FDA prescribing information includes a warning about acute pancreatitis based on clinical reports, establishing a direct causal link remains complex. Current research shows a possible association rather than confirmed causation, as patients taking semaglutide often have underlying risk factors including obesity and metabolic syndrome. This article examines the evidence, symptoms to watch for, and practical guidance for patients and healthcare providers navigating pancreatic safety concerns.
Quick Answer: Current evidence suggests a possible association between semaglutide and pancreatitis rather than a confirmed causal relationship, with clinical trials showing relatively low incidence rates.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for managing type 2 diabetes mellitus and chronic weight management. Marketed under brand names including Ozempic, Wegovy, and Rybelsus, this medication works by mimicking the action of naturally occurring GLP-1 hormone. It enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways.
The pancreas plays a dual role in metabolism: its endocrine cells produce hormones like insulin and glucagon, while exocrine cells secrete digestive enzymes. Because semaglutide influences pancreatic beta cells to release insulin in a glucose-dependent manner, questions naturally arise about its broader effects on pancreatic tissue. Pancreatitis—inflammation of the pancreas—can be acute (sudden onset) or chronic (persistent inflammation), and both forms carry significant morbidity.
Since GLP-1 receptor agonists became widely prescribed, regulatory agencies and researchers have monitored potential pancreatic safety signals. The FDA prescribing information for semaglutide products includes a warning about acute pancreatitis based on postmarketing reports and clinical trial data. However, establishing a definitive causal relationship remains complex, as patients prescribed semaglutide often have underlying risk factors for pancreatitis, including obesity, hypertriglyceridemia, and metabolic syndrome.
Understanding the relationship between semaglutide and pancreatic health requires examining both the pharmacological mechanisms and the clinical evidence, while recognizing that correlation does not automatically establish causation. This article reviews current research, clinical guidance, and practical considerations for patients and healthcare providers.
The question of whether semaglutide directly causes pancreatitis remains an area of ongoing investigation, with current evidence suggesting a possible association rather than a confirmed causal relationship. Clinical trials of semaglutide have reported cases of acute pancreatitis, though the incidence rates remain relatively low. In the SUSTAIN clinical trial program, cases of pancreatitis were reported, but at rates that did not reach statistical significance in most individual studies when compared to control groups.
Observational studies provide additional context but face methodological challenges: patients prescribed GLP-1 receptor agonists typically have more advanced metabolic disease, higher body mass index, and greater baseline pancreatitis risk than comparison groups. This confounding makes it difficult to determine whether any observed risk is due to the medication or underlying patient characteristics.
Importantly, meta-analyses of randomized controlled trials have generally not shown a statistically significant increased risk of pancreatitis with GLP-1 receptor agonists as a class. Observational studies show mixed results, with some suggesting a modest association and others finding no significant relationship after adjusting for confounding factors.
Mechanistically, there is no established biological pathway by which semaglutide would directly damage pancreatic tissue. Some researchers have hypothesized that GLP-1 receptor stimulation might promote pancreatic duct cell proliferation or increase pancreatic enzyme secretion, but animal studies have not consistently demonstrated these effects at therapeutic doses. The FDA and European Medicines Agency have reviewed available data and concluded that while pancreatitis should be considered a potential risk, the evidence does not support withdrawing these medications from the market.
Current clinical guidance from the American Diabetes Association acknowledges this uncertainty, recommending that healthcare providers remain vigilant for pancreatitis symptoms but not avoid GLP-1 receptor agonists solely based on theoretical pancreatic concerns. The benefit-risk profile generally favors use in appropriate patients, particularly given the cardiovascular and metabolic benefits demonstrated in outcome trials.
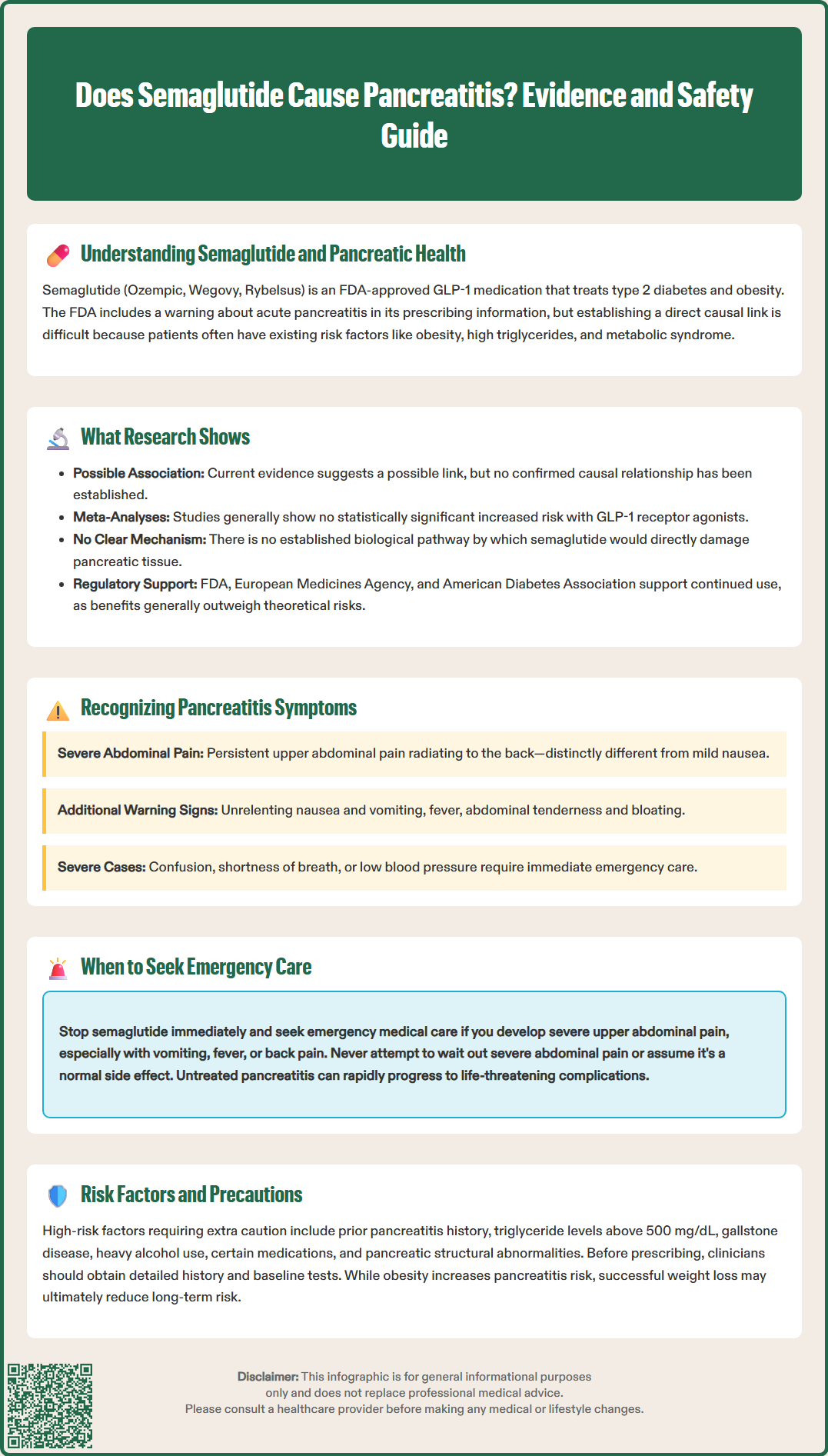
Patients taking semaglutide should be educated about pancreatitis warning signs, as early recognition and prompt medical evaluation are essential for optimal outcomes. The hallmark symptom of acute pancreatitis is severe, persistent abdominal pain, typically located in the upper abdomen (epigastric region) and often radiating to the back. This pain characteristically develops suddenly, remains constant rather than cramping, and worsens after eating. Unlike common gastrointestinal side effects of semaglutide—such as nausea, which typically improves over time—pancreatitis pain is severe and unrelenting.
Accompanying symptoms may include:
Nausea and vomiting that is persistent and does not respond to usual remedies
Possible fever and elevated heart rate
Abdominal tenderness when the area is touched
Abdominal distension or bloating
In severe cases, signs of systemic illness including confusion, shortness of breath, or low blood pressure
Diagnosis of acute pancreatitis typically requires at least two of three criteria: characteristic abdominal pain, elevated pancreatic enzymes (lipase or amylase) greater than three times the upper limit of normal, and imaging findings consistent with pancreatic inflammation.
It is important to distinguish pancreatitis from the common gastrointestinal side effects that affect many semaglutide users, particularly during dose escalation. Typical GLP-1-related nausea is usually mild to moderate, improves with dietary modifications, and is not accompanied by severe abdominal pain. Pancreatitis pain is qualitatively different—patients often describe it as the worst abdominal pain they have experienced.
The FDA Medication Guide for semaglutide products explicitly instructs patients to discontinue the medication and seek immediate medical attention if pancreatitis is suspected. Healthcare providers should emphasize this guidance during prescribing discussions. Patients should not attempt to "wait out" severe abdominal pain or assume it represents a normal medication side effect. When in doubt, evaluation in an emergency department is appropriate, as acute pancreatitis can rapidly progress to serious complications including pancreatic necrosis, systemic inflammatory response, and multi-organ failure.
Certain patient populations face elevated pancreatitis risk and require careful consideration before initiating semaglutide therapy. According to FDA prescribing information, semaglutide has not been studied in patients with a history of pancreatitis, and healthcare providers should consider alternative therapies in these individuals. This is not a formal contraindication, but rather a precautionary recommendation based on limited safety data in this population. For patients with chronic pancreatitis, individualized decision-making is appropriate, weighing potential risks against benefits in consultation with specialists.
Key risk factors for pancreatitis that warrant heightened vigilance include:
Hypertriglyceridemia: Triglyceride levels above 500 mg/dL increase pancreatitis risk, with markedly elevated risk when levels exceed 1,000 mg/dL. Semaglutide may modestly reduce triglycerides, but severe hypertriglyceridemia should be addressed before initiation.
Gallstone disease: Cholelithiasis is a leading cause of acute pancreatitis. Rapid weight loss associated with semaglutide may paradoxically increase gallstone formation risk, as noted in FDA prescribing information.
Alcohol use disorder: Heavy alcohol consumption is a major pancreatitis risk factor and may compound any medication-related risk.
Certain medications: Concurrent use of other drugs associated with pancreatitis (such as certain immunosuppressants or HIV medications) requires careful consideration.
Anatomical abnormalities: Pancreatic duct abnormalities or pancreas divisum may increase susceptibility.
Obesity itself is an independent risk factor for pancreatitis, creating a complex clinical scenario where the condition being treated contributes to the potential adverse effect. However, successful weight reduction may ultimately decrease long-term pancreatitis risk. The American Association of Clinical Endocrinologists recommends individualized decision-making, considering the patient's complete metabolic profile, pancreatitis history, and availability of alternative therapies.
Before prescribing semaglutide, clinicians should obtain a thorough medical history specifically addressing prior pancreatitis episodes, gallbladder disease, alcohol use, and family history of pancreatic disorders. Baseline laboratory evaluation including lipid panel and liver function tests represents good clinical practice. There is no evidence supporting routine pancreatic enzyme monitoring in asymptomatic patients.
If you develop symptoms suggestive of pancreatitis while taking semaglutide, immediate action is essential. Stop taking semaglutide immediately and do not resume without explicit guidance from your healthcare provider. Seek emergency medical evaluation the same day if you experience severe, persistent upper abdominal pain, especially if accompanied by vomiting, fever, or pain radiating to your back. Do not wait for a scheduled appointment or attempt to manage severe symptoms at home.
In the emergency department or urgent care setting, diagnostic evaluation typically includes:
Serum lipase (preferred) and possibly amylase: Pancreatic enzyme levels elevated to three times the upper limit of normal support pancreatitis diagnosis
Complete blood count and metabolic panel: To assess for systemic complications
Abdominal imaging: Right upper quadrant ultrasound is typically performed first to evaluate for gallstones; CT scan or MRI may be ordered if diagnosis remains unclear or to assess for complications
Triglyceride level: To identify hypertriglyceridemia as a contributing factor
If pancreatitis is confirmed, treatment focuses on supportive care including intravenous fluids, pain management, and monitoring for complications. Current guidelines favor early oral or enteral feeding as tolerated, rather than prolonged fasting. Most cases of acute pancreatitis resolve with appropriate management, though severe cases may require intensive care unit admission. As stated in FDA prescribing information, semaglutide should not be restarted after a confirmed pancreatitis episode, and alternative diabetes or weight management strategies should be pursued.
For patients who experience milder abdominal symptoms that do not clearly indicate pancreatitis, contact your prescribing physician within 24 hours for guidance. They may recommend temporarily holding semaglutide, adjusting the dose, or scheduling an in-person evaluation. Keep a symptom diary noting pain location, severity (on a 0-10 scale), timing relative to meals and medication doses, and associated symptoms.
After any pancreatitis episode, regardless of suspected cause, follow-up care should include identifying and addressing modifiable risk factors such as hypertriglyceridemia, gallstones, and alcohol use. Your healthcare team will work with you to develop an alternative treatment plan that effectively manages your diabetes or weight while minimizing pancreatic risk. Open communication about symptoms and concerns is essential for safe medication management.
The hallmark symptom is severe, persistent upper abdominal pain that often radiates to the back, accompanied by nausea, vomiting, and abdominal tenderness. This pain is qualitatively different from common GLP-1 side effects and requires immediate medical evaluation.
FDA prescribing information recommends healthcare providers consider alternative therapies for patients with prior pancreatitis, as semaglutide has not been adequately studied in this population. Individualized decision-making with your physician is essential.
No, FDA prescribing information states that semaglutide should not be restarted after a confirmed pancreatitis episode. Your healthcare provider should work with you to develop alternative diabetes or weight management strategies.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.