LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does semaglutide help with insulin resistance? This question is increasingly relevant as millions of Americans struggle with metabolic dysfunction. Insulin resistance—when cells become less responsive to insulin—affects approximately 38% of US adults with prediabetes and represents a critical pathway to type 2 diabetes and cardiovascular disease. Semaglutide, a GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management, has demonstrated significant metabolic benefits. While not specifically approved for treating insulin resistance alone, clinical evidence suggests semaglutide improves insulin sensitivity markers primarily through substantial weight loss and enhanced glycemic control, offering potential benefits for appropriately selected patients.
Quick Answer: Semaglutide improves insulin sensitivity primarily through significant weight loss and enhanced glycemic control rather than direct insulin-sensitizing effects.
Insulin resistance occurs when cells in muscle, fat, and liver tissue become less responsive to insulin, the hormone responsible for facilitating glucose uptake from the bloodstream. As a result, the pancreas compensates by producing more insulin to maintain normal blood glucose levels, leading to hyperinsulinemia. Over time, this compensatory mechanism can fail, resulting in prediabetes and eventually type 2 diabetes mellitus.
Insulin resistance is common in the United States, with prediabetes affecting approximately 38% of US adults according to CDC estimates. This metabolic dysfunction represents a critical component of metabolic syndrome, which includes central obesity, dyslipidemia, hypertension, and elevated fasting glucose. The constellation of these risk factors significantly increases cardiovascular disease risk, making insulin resistance a major public health concern.
Insulin resistance develops through multiple pathways, including chronic inflammation, excess visceral adiposity, physical inactivity, and genetic predisposition. Adipose tissue in insulin-resistant states releases increased free fatty acids and inflammatory cytokines such as tumor necrosis factor-alpha and interleukin-6, which interfere with insulin signaling pathways at the cellular level. This creates a vicious cycle where metabolic dysfunction perpetuates further insulin resistance.
The clinical consequences extend beyond glucose metabolism. Insulin resistance is associated with metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as NAFLD), polycystic ovary syndrome (PCOS), obstructive sleep apnea, and certain metabolic-related conditions. The US Preventive Services Task Force recommends screening adults aged 35-70 years with overweight or obesity for prediabetes and diabetes. Early identification and intervention are essential to prevent progression to overt diabetes and reduce cardiovascular morbidity and mortality. Lifestyle modifications including weight loss, dietary changes, and increased physical activity remain first-line interventions, though pharmacological options may be considered for specific high-risk individuals.
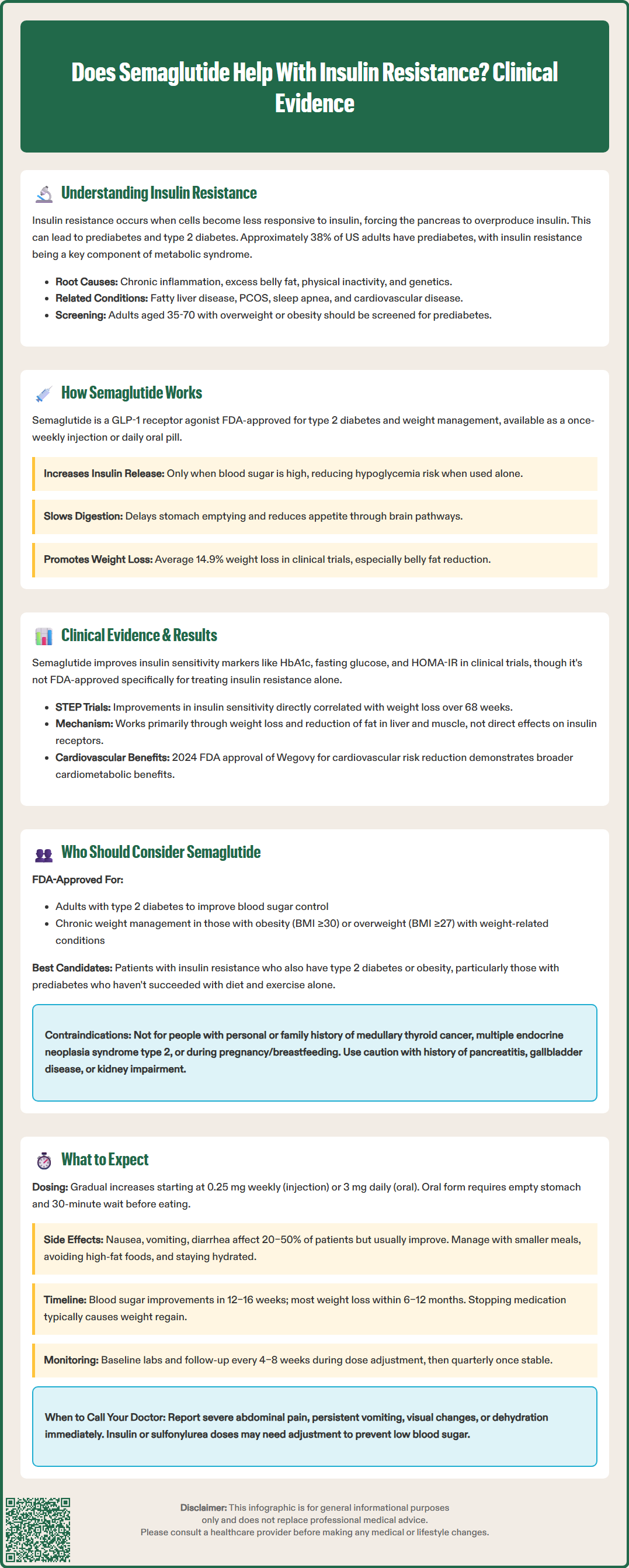
Semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) approved by the FDA for the treatment of type 2 diabetes (under the brand names Ozempic and Rybelsus) and chronic weight management (as Wegovy). The medication is a synthetic analog of human GLP-1, modified with an albumin side chain that extends its half-life to approximately one week, allowing for once-weekly subcutaneous administration or daily oral dosing.
The primary mechanism of action involves binding to GLP-1 receptors located throughout the body, particularly in pancreatic beta cells, the gastrointestinal tract, and the central nervous system. In pancreatic beta cells, semaglutide enhances glucose-dependent insulin secretion, meaning insulin release occurs primarily when blood glucose levels are elevated. This glucose-dependent mechanism significantly reduces the risk of hypoglycemia when used as monotherapy, though the risk increases when combined with insulin or sulfonylureas. Simultaneously, semaglutide suppresses inappropriate glucagon secretion from pancreatic alpha cells, further improving glycemic control.
Beyond pancreatic effects, semaglutide slows gastric emptying, which moderates postprandial glucose excursions and promotes satiety. Central nervous system effects include reduced appetite and food intake through actions on hypothalamic appetite centers and reward pathways. These mechanisms contribute to the substantial weight loss observed in clinical trials, with patients in the STEP 1 trial losing an average of 14.9% of body weight (compared to 2.4% with placebo) on the 2.4 mg weekly dose used for obesity management.
The medication's effects on insulin resistance are multifactorial and indirect. By promoting weight loss, particularly visceral adipose tissue reduction, semaglutide decreases the inflammatory burden and free fatty acid release that drive insulin resistance. Additionally, improved glycemic control reduces glucotoxicity, a phenomenon where chronic hyperglycemia itself impairs insulin signaling. The combination of these effects creates a favorable metabolic environment that can enhance insulin sensitivity over time.
Multiple clinical trials have demonstrated semaglutide's beneficial effects on markers of insulin sensitivity, though it is important to note that the medication is not specifically FDA-approved for treating insulin resistance as a standalone indication. The SUSTAIN clinical trial program, which evaluated semaglutide in over 8,000 patients with type 2 diabetes, consistently showed improvements in HbA1c, fasting plasma glucose, and body weight—all indirect indicators of improved insulin sensitivity.
The homeostatic model assessment of insulin resistance (HOMA-IR), a validated surrogate marker calculated from fasting glucose and insulin levels, has shown improvement in patients treated with semaglutide. In the STEP trials evaluating semaglutide for weight management in individuals without diabetes, participants demonstrated reductions in HOMA-IR alongside substantial weight loss. For example, in the STEP 1 trial, participants receiving semaglutide 2.4 mg weekly showed improvements in insulin sensitivity markers that correlated with the degree of weight loss achieved after 68 weeks of treatment.
Limited studies using hyperinsulinemic-euglycemic clamp techniques—the gold standard for measuring insulin sensitivity—suggest that GLP-1 receptor agonists may improve peripheral insulin sensitivity, primarily through weight loss rather than direct cellular effects. These improvements appear to occur primarily through weight loss and reduction in ectopic fat deposition in liver and muscle tissue, rather than through direct insulin-sensitizing effects on cellular receptors.
It is crucial to understand that semaglutide's effects on insulin resistance are largely mediated through weight reduction and improved glycemic control rather than direct insulin-sensitizing action like metformin or thiazolidinediones. The American Diabetes Association's Standards of Care acknowledge GLP-1 receptor agonists as effective glucose-lowering agents with cardiovascular and renal benefits, but they do not specifically recommend them solely for insulin resistance in the absence of diabetes or obesity indications. Notably, the 2024 FDA approval of Wegovy for cardiovascular risk reduction in adults with established cardiovascular disease and obesity/overweight (based on the SELECT trial) provides additional evidence of cardiometabolic benefits beyond glycemic control.
Semaglutide is FDA-approved for specific indications, and prescribing decisions should align with these approved uses rather than treating insulin resistance as an isolated condition. The medication is indicated for adults with type 2 diabetes to improve glycemic control as an adjunct to diet and exercise, and for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. In 2024, the FDA also approved Wegovy to reduce the risk of cardiovascular death, heart attack, and stroke in adults with established cardiovascular disease and either obesity or overweight.
Patients with documented insulin resistance who also meet criteria for type 2 diabetes or obesity represent the most appropriate candidates. This includes individuals with prediabetes (HbA1c 5.7–6.4%, fasting glucose 100–125 mg/dL, or 2-hour glucose 140–199 mg/dL on oral glucose tolerance testing) who have elevated BMI and have not achieved adequate results with lifestyle interventions. The American Diabetes Association guidelines recommend lifestyle interventions as first-line therapy for prediabetes, with consideration of metformin (not GLP-1 RAs) in specific high-risk individuals, such as those with BMI ≥35 kg/m², age <60 years, or prior gestational diabetes.
Certain populations may derive particular benefit from semaglutide's metabolic effects. Patients with metabolic dysfunction-associated steatotic liver disease (MASLD, formerly NAFLD) and insulin resistance may experience improvements in hepatic steatosis and liver enzyme elevations, though this represents an off-label use with evolving evidence. Women with polycystic ovary syndrome, a condition characterized by insulin resistance, may see improvements in metabolic parameters, though semaglutide is not specifically approved for PCOS treatment. Individuals with established cardiovascular disease and type 2 diabetes represent another priority group, given semaglutide's demonstrated cardiovascular benefits.
Contraindications and precautions must be carefully considered. Semaglutide is contraindicated in patients with personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2, and during pregnancy or breastfeeding. Caution is warranted in patients with history of pancreatitis, gallbladder disease, severe gastrointestinal disease including gastroparesis, diabetic retinopathy, or renal impairment. Semaglutide is not indicated for type 1 diabetes. Prescribing decisions should involve shared decision-making, considering individual patient factors, preferences, cost considerations, and realistic expectations about outcomes.
Semaglutide therapy requires gradual dose escalation to minimize gastrointestinal adverse effects, which represent the most common tolerability issue. For the subcutaneous formulation (Ozempic for diabetes, Wegovy for weight management), treatment typically begins at 0.25 mg once weekly for four weeks, then increases to 0.5 mg weekly. Further dose escalations occur monthly as tolerated, with maximum doses of 2.0 mg weekly for diabetes and 2.4 mg weekly for weight management. The oral formulation (Rybelsus) starts at 3 mg daily, increasing to 7 mg and potentially 14 mg at monthly intervals. Rybelsus must be taken on an empty stomach with no more than 4 ounces of plain water, at least 30 minutes before the first food, beverage, or other oral medications of the day.
Gastrointestinal side effects including nausea, vomiting, diarrhea, constipation, and abdominal discomfort affect 20–50% of patients, particularly during dose escalation periods. These symptoms are generally mild to moderate and diminish over time as physiological adaptation occurs. Practical strategies to minimize these effects include eating smaller, more frequent meals, avoiding high-fat foods, staying well-hydrated, and taking the medication consistently on the same day and time each week. If symptoms become intolerable, dose reduction or temporarily pausing escalation may be necessary.
Metabolic improvements typically emerge gradually over several months. Patients with type 2 diabetes generally observe meaningful HbA1c reductions within 12–16 weeks, with maximal effects by 6 months. Weight loss follows a similar trajectory, with most reduction occurring in the first 6–12 months of therapy. Improvements in insulin resistance markers, while not routinely monitored in clinical practice, parallel these changes. Patients should understand that semaglutide is not a short-term intervention; sustained benefits require ongoing treatment, and discontinuation typically results in weight regain and metabolic deterioration.
Regular monitoring is essential for safety and efficacy assessment. Baseline evaluation should include HbA1c (if diabetic), comprehensive metabolic panel, lipid profile, and assessment for contraindications. Follow-up visits at 4–8 week intervals during dose escalation allow for adverse effect monitoring and dose adjustment. Once stable on a maintenance dose, quarterly visits are typically appropriate. Patients should be counseled to report severe abdominal pain (potential pancreatitis), right upper quadrant pain (possible gallbladder disease), visual changes (especially with diabetic retinopathy), persistent nausea or vomiting, or signs of dehydration which may increase risk of acute kidney injury. When combined with insulin or sulfonylureas, dose adjustments of these medications may be needed to prevent hypoglycemia. Women of childbearing potential should use effective contraception during treatment. Lifestyle modifications including dietary counseling and physical activity recommendations should continue as foundational therapy.
Semaglutide is not FDA-approved for treating insulin resistance as a standalone condition. It is approved for type 2 diabetes and chronic weight management in adults with obesity or overweight with weight-related comorbidities, conditions often associated with insulin resistance.
Metabolic improvements typically emerge gradually over several months, with meaningful changes in glycemic control and insulin sensitivity markers generally observed within 12–16 weeks and maximal effects by 6 months of treatment.
Semaglutide and metformin work through different mechanisms—metformin directly improves insulin sensitivity while semaglutide primarily works through weight loss and enhanced insulin secretion. The American Diabetes Association recommends metformin as the preferred pharmacological option for prediabetes in high-risk individuals.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.