LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
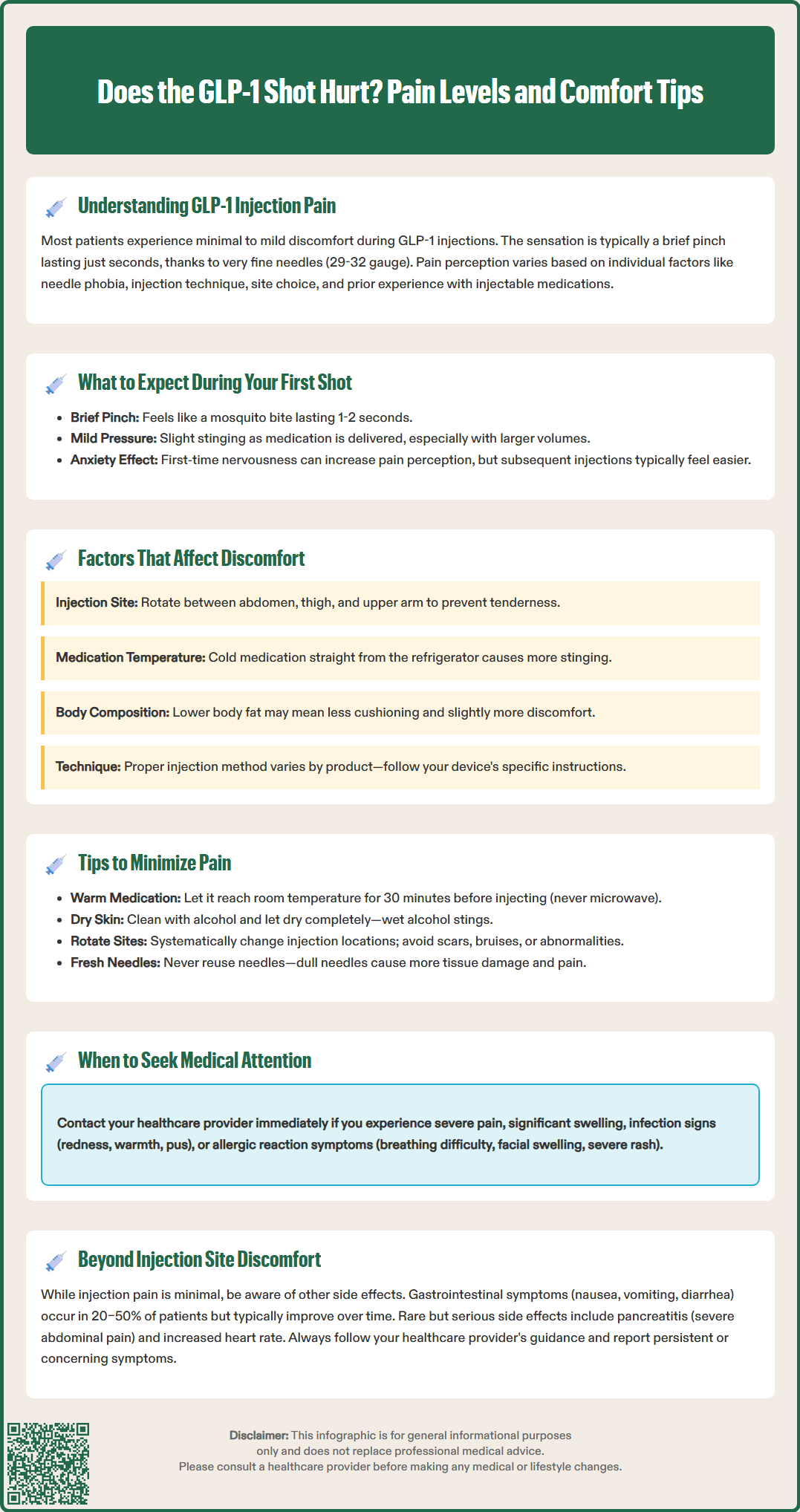
Does the GLP-1 shot hurt? Most patients report minimal to mild discomfort with GLP-1 injections used for type 2 diabetes and weight management. These medications—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—use very fine needles (29–32 gauge) designed to reduce pain during subcutaneous administration. While pain perception varies individually, the typical sensation is a brief pinch lasting only seconds. Proper injection technique, site rotation, and allowing medication to reach room temperature can further minimize discomfort. Understanding what to expect and how to optimize your injection technique helps ensure a more comfortable experience with these FDA-approved medications.
Quick Answer: GLP-1 injections typically cause minimal to mild discomfort, with most patients experiencing only a brief pinching sensation lasting seconds due to the very fine needles used.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are injectable medications approved by the FDA for type 2 diabetes management and, in some formulations, chronic weight management. Common agents include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro, Zepbound)—with tirzepatide being a dual GIP/GLP-1 receptor agonist rather than a GLP-1-only medication. These medications work by mimicking incretin hormones, enhancing glucose-dependent insulin secretion, suppressing glucagon release, slowing gastric emptying, and promoting satiety through central nervous system pathways.
Most patients report minimal to mild discomfort with GLP-1 injections. The needles used are typically very fine (29–32 gauge) and short (4–8 mm), designed specifically to reduce pain during subcutaneous administration. Many patients find that injection-related pain is generally mild, with the brief, pinching sensation most patients describe lasting only seconds. Some devices feature completely concealed needles in autoinjector formats.
Pain perception is highly individual and influenced by multiple factors including needle phobia, injection technique, anatomical site selection, and previous experience with injectable medications. While some patients report virtually no sensation, others may experience mild stinging or burning, particularly during initial injections. It is important to note that significant or persistent pain at injection sites is uncommon and may indicate improper technique or, rarely, local adverse reactions requiring clinical evaluation. The American Diabetes Association emphasizes that proper injection education can improve patient comfort and medication adherence.
Before your first GLP-1 injection, your healthcare provider or diabetes educator should provide comprehensive training on proper administration technique. GLP-1 medications come in different delivery systems: some are prefilled, single-use autoinjectors with hidden needles (like Wegovy and Trulicity), while others are multi-dose pens requiring needle attachment and priming (like Ozempic and Victoza). Always follow the specific Instructions for Use (IFU) provided with your medication.
During the actual injection, you will typically experience a brief sensation as the needle penetrates the skin—often described as a small pinch or mosquito bite. This initial sensation usually lasts 1–2 seconds. As the medication is delivered, some patients report a mild pressure sensation or slight stinging. The stinging may be more noticeable with larger volume injections or if the medication is cold from refrigerator storage. After needle withdrawal, there may be minimal residual tenderness at the injection site, though this typically resolves within minutes.
It is normal to feel anxious before your first injection, and this anxiety can amplify pain perception. Many patients report that subsequent injections are less uncomfortable as they become familiar with the process and develop confidence in their technique. Mild bleeding (a small drop) or bruising at the injection site occurs occasionally and is generally not concerning. If you experience severe pain, significant swelling, signs of infection (increasing redness, warmth, purulent drainage), or signs of allergic reaction (trouble breathing, facial/throat swelling, severe rash), contact your healthcare provider promptly for assessment.
Several modifiable and non-modifiable factors influence the level of discomfort experienced during GLP-1 injections. Injection site selection plays a crucial role—the abdomen (at least 2 inches from the navel), thigh, and upper arm are FDA-approved sites for most GLP-1 medications, with comfort levels varying between individuals. Rotating injection sites with each dose, as recommended by the American Association of Clinical Endocrinology (AACE) and the American Diabetes Association, helps prevent lipohypertrophy (fatty lumps) and reduces localized tenderness from repeated injections in the same area.
Medication temperature significantly affects comfort. Cold medication injected directly from the refrigerator often causes more stinging and discomfort than medication allowed to reach room temperature. Most GLP-1 product labels recommend removing the pen from refrigeration before injection, with specific timing varying by product (typically around 30 minutes). Injection technique is equally important—the proper technique varies by device and needle length, so always follow your specific product's Instructions for Use. Some devices require pinching a fold of skin while others do not; injection angles may vary based on needle length and body composition.
Individual factors including body composition, skin sensitivity, and psychological state also matter. Patients with lower body fat may experience more discomfort as there is less cushioning tissue. Anxiety and needle phobia can heighten pain perception through central sensitization mechanisms. Previous negative experiences with injections may create anticipatory anxiety that amplifies discomfort. Additionally, some patients report that certain injection sites may feel more sensitive at different times.
Evidence-based strategies can substantially reduce injection-related discomfort. Allow medication to warm: Remove your GLP-1 pen from the refrigerator and allow it to reach room temperature according to your product's Instructions for Use (typically around 30 minutes). Never microwave or heat the medication artificially, as this can denature the protein and reduce efficacy. Clean and prepare the site: Use an alcohol swab to clean the injection area and allow it to dry completely before injecting—wet alcohol on the skin can cause stinging as the needle penetrates.
Follow device-specific instructions: Each GLP-1 product has its own FDA-approved Instructions for Use that specify whether to pinch the skin, the proper injection angle, and how long to hold the device in place after injection. Always follow these specific guidelines rather than general advice. Do not inject through clothing, and avoid rubbing the injection site vigorously afterward, which can increase irritation.
Rotate injection sites systematically: Develop a rotation schedule using different areas of the approved injection sites. Avoid injecting into areas with scars, bruises, or skin abnormalities. Consider relaxation techniques: Some patients find that controlled breathing or distraction methods help reduce anxiety during injections. While some suggest applying a cold pack near (not on) the injection site before injection, evidence for this approach is limited.
Use proper needle disposal: Never reuse needles, as they become dull and cause more tissue trauma with subsequent use. Follow FDA guidelines for safe sharps disposal. Never share pens or needles with others, even if you change the needle. If you consistently experience significant pain despite proper technique, discuss alternative injection sites or formulations with your healthcare provider. Some patients may benefit from consultation with a diabetes educator for technique refinement.
While injection site discomfort is typically minimal and transient, GLP-1 receptor agonists are associated with several systemic side effects that patients should understand. Gastrointestinal effects are the most common adverse reactions, occurring in 20–50% of patients depending on the specific agent and dose. These include nausea, vomiting, diarrhea, constipation, and abdominal pain. The mechanism relates to delayed gastric emptying and direct effects on the gastrointestinal tract. Nausea is typically most pronounced during dose escalation and often improves with continued use as physiological tolerance develops. FDA labeling and the American Diabetes Association recommend gradual dose titration to minimize gastrointestinal symptoms.
Hypoglycemia risk is generally low with GLP-1 agonists when used as monotherapy, as their glucose-lowering effect is glucose-dependent. However, when combined with insulin or sulfonylureas, the risk increases substantially. Patients should be educated on hypoglycemia recognition (tremor, palpitations, sweating, confusion) and management with 15 grams of fast-acting carbohydrate. Dose adjustment of concomitant medications may be necessary.
Serious but rare adverse effects require clinical vigilance. Acute pancreatitis has been reported with GLP-1 agonists, and FDA labeling recommends discontinuing the medication if pancreatitis is suspected. Patients should seek immediate medical attention for severe, persistent abdominal pain radiating to the back, especially if accompanied by nausea and vomiting. There is a theoretical risk of medullary thyroid carcinoma based on rodent studies, leading to a boxed warning and contraindication in patients with personal or family history of medullary thyroid cancer or Multiple Endocrine Neoplasia syndrome type 2.
Other notable effects include injection site reactions beyond pain (erythema, pruritus, induration in 1–3% of patients), increased heart rate (particularly with liraglutide), gallbladder disease (including gallstones and cholecystitis), and potential dehydration-related acute kidney injury. Worsening of diabetic retinopathy has been observed primarily with semaglutide during rapid glycemic improvement, particularly in patients with pre-existing retinopathy. Patients should report persistent injection site changes, unexplained neck masses, severe gastrointestinal symptoms, or signs of pancreatitis promptly for appropriate clinical assessment and management.
GLP-1 injections typically cause less discomfort than many other injectable medications due to their very fine needles (29–32 gauge) and short length (4–8 mm). Most patients describe the sensation as a brief pinch similar to a mosquito bite, lasting only 1–2 seconds.
Allow your medication to reach room temperature before injecting (typically 30 minutes), ensure the alcohol swab dries completely before injection, rotate injection sites systematically, and follow your specific device's Instructions for Use. Never reuse needles, as dull needles cause more tissue trauma and discomfort.
Contact your healthcare provider if you experience severe pain, significant swelling, signs of infection (increasing redness, warmth, purulent drainage), or allergic reaction symptoms (difficulty breathing, facial swelling, severe rash). Mild tenderness resolving within minutes is normal, but persistent or worsening pain requires clinical evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.