LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
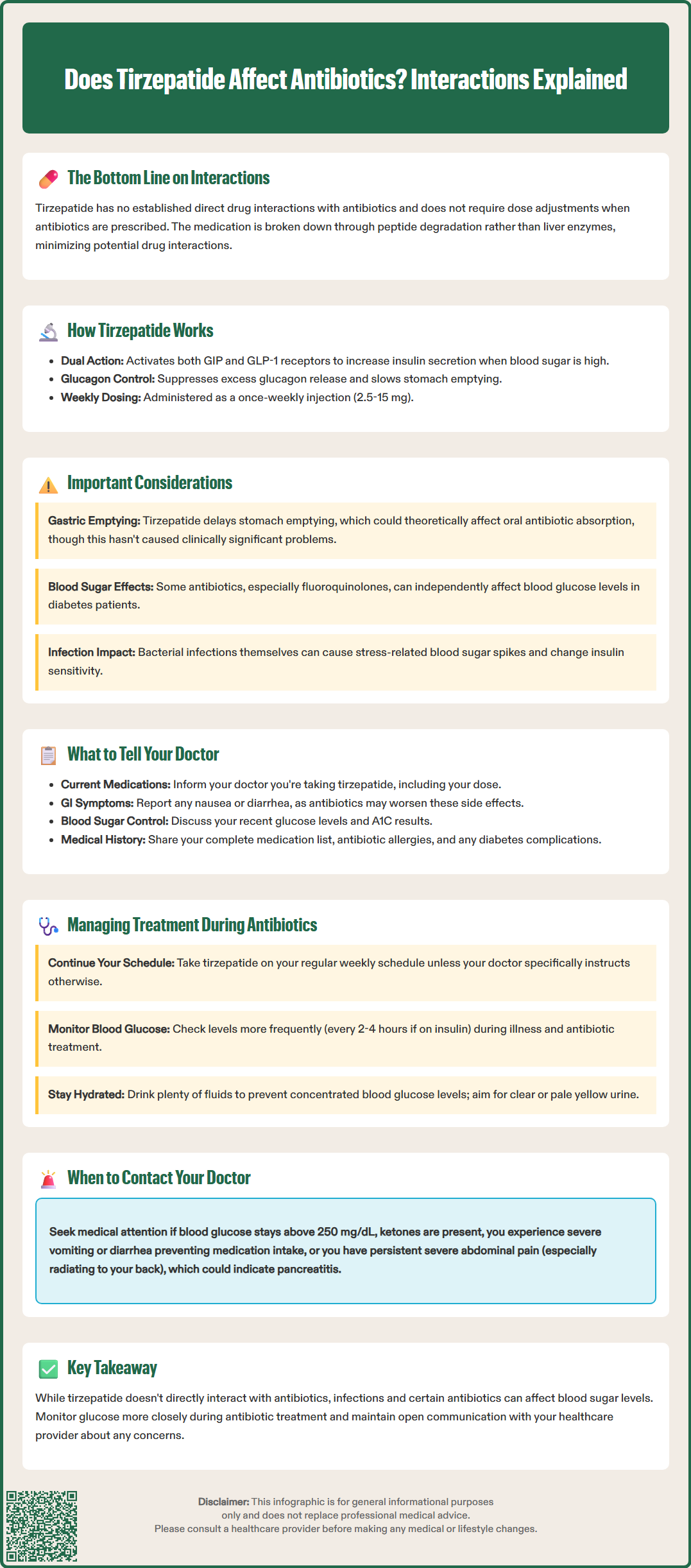
Tirzepatide (Mounjaro, Zepbound) is a dual GIP and GLP-1 receptor agonist used for type 2 diabetes and weight management. As more patients use this medication, questions about potential drug interactions naturally arise, particularly with commonly prescribed antibiotics. According to FDA prescribing information, tirzepatide does not have established direct interactions with antibiotic medications. However, understanding how these medications work together—and how illness itself affects diabetes control—remains important for safe, effective treatment. This article examines the current evidence on tirzepatide and antibiotic use, practical management strategies, and what patients should discuss with their healthcare providers.
Quick Answer: Tirzepatide does not have established direct interactions with antibiotics according to FDA prescribing information.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for type 2 diabetes management and chronic weight management. As patients increasingly use this medication, questions arise about potential interactions with other commonly prescribed drugs, including antibiotics.
According to the FDA prescribing information, there are no established direct pharmacokinetic or pharmacodynamic interactions between tirzepatide and antibiotic medications. Antibiotics are not listed among medications requiring specific dose adjustments when used with tirzepatide. This reflects the distinct mechanisms by which these drug classes operate within the body.
However, the FDA label does caution that tirzepatide delays gastric emptying, which may impact the absorption of concomitantly administered oral medications. This effect is most pronounced after initial doses and diminishes over time. While this has not been specifically demonstrated to cause clinically significant problems with antibiotics in practice, it represents a theoretical consideration for oral antibiotic absorption timing.
Additionally, certain antibiotics, particularly fluoroquinolones, can themselves affect blood glucose levels, which becomes relevant for patients managing diabetes. Infections requiring antibiotic treatment can also independently affect glucose control through stress responses and inflammation.
Patients taking tirzepatide who require antibiotic therapy should understand that while direct medication interactions appear minimal, the underlying infection and potentially the antibiotic itself may impact diabetes management. Acute illness, particularly bacterial infections, can cause stress hyperglycemia and alter insulin sensitivity, necessitating closer glucose monitoring during the treatment period.
Tirzepatide functions through a novel dual-agonist mechanism, simultaneously activating both GIP and GLP-1 receptors. This dual action distinguishes it from single-agonist GLP-1 receptor agonists like semaglutide or dulaglutide. The medication enhances glucose-dependent insulin secretion from pancreatic beta cells, meaning insulin release occurs primarily when blood glucose levels are elevated, which reduces hypoglycemia risk.
Beyond insulin secretion, tirzepatide suppresses inappropriate glucagon release from pancreatic alpha cells, particularly in postprandial states when glucagon elevation would be counterproductive. This glucagon suppression helps prevent excessive hepatic glucose production. The medication also delays gastric emptying, with this effect being most pronounced after initial doses and diminishing over time. This gastric effect contributes to improved postprandial glucose control and promotes satiety, supporting weight loss.
Tirzepatide is administered as a once-weekly subcutaneous injection, with doses ranging from 2.5 mg to 15 mg depending on indication and tolerability. The medication undergoes proteolytic degradation (peptide catabolism), with a half-life of approximately five days. Importantly, tirzepatide is not metabolized through the cytochrome P450 enzyme system, and renal impairment has minimal impact on its exposure. This metabolic profile explains why tirzepatide has minimal potential for metabolism-based pharmacokinetic interactions with most medications, including antibiotics.
The FDA label notes that tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis. Additionally, the label cautions that tirzepatide may reduce the exposure of oral contraceptives taken concomitantly, particularly after initiation and dose escalation, potentially requiring alternative contraceptive methods.
The medication's pharmacology centers on peptide-based signaling rather than interference with bacterial cell walls, protein synthesis, or DNA replication—the targets of antibiotic therapy. This fundamental difference in mechanism provides reassurance regarding the absence of direct molecular interactions between tirzepatide and antimicrobial agents.
The FDA prescribing information for tirzepatide (Mounjaro, Zepbound) does not list specific interactions with antibiotics. While clinical trials such as the SURPASS program included patients who may have required antibiotic treatment during study participation, no formal analyses specifically addressing antibiotic co-administration have been published.
No specific antibiotic interactions are listed in the FDA label; however, absorption-based interactions are theoretically possible due to tirzepatide's effect on gastric emptying. This effect is most pronounced after initial doses and diminishes with continued treatment. For most antibiotics, this delayed absorption has not been demonstrated to result in treatment failures, though formal interaction studies are limited.
The theoretical consideration involves the delayed gastric emptying caused by tirzepatide, which could potentially affect the absorption rate of oral antibiotics. For antibiotics requiring specific timing relative to meals (such as certain fluoroquinolones), standard administration instructions remain appropriate. Medications with narrow therapeutic indices warrant particular attention, though most commonly prescribed oral antibiotics do not fall into this category.
It's worth noting that certain antibiotics, particularly fluoroquinolones, have been associated with blood glucose disturbances according to FDA safety communications. This antibiotic-specific effect on glucose levels is independent of any interaction with tirzepatide but represents an important clinical consideration for patients with diabetes.
The American Diabetes Association guidelines do not specifically address continuing or discontinuing GLP-1 receptor agonists or dual agonists like tirzepatide when antibiotics are prescribed. Clinical decision-making should focus on the patient's overall condition, ability to maintain adequate hydration, and glucose control rather than concerns about direct medication incompatibility. Patients should continue their prescribed tirzepatide regimen unless specifically instructed otherwise by their healthcare provider based on their clinical status.
When your healthcare provider prescribes antibiotics, comprehensive medication disclosure remains essential for safe care. Inform your doctor that you are taking tirzepatide, including your current dose and how long you have been on the medication. While tirzepatide does not interact with antibiotics directly, this information helps your provider make informed decisions about your overall care plan.
Discuss any gastrointestinal symptoms you are currently experiencing from tirzepatide, particularly nausea, vomiting, or diarrhea. These are common adverse effects, especially during dose escalation phases. If you are already experiencing significant GI symptoms, adding an antibiotic—which may also cause gastrointestinal upset—could compound these effects and impact your ability to maintain adequate hydration and nutrition. Your provider may select an antibiotic with a more favorable GI tolerability profile or provide additional supportive medications.
Provide information about your recent glucose control, including any patterns of hypoglycemia or hyperglycemia. Infections can significantly affect blood sugar levels, often causing elevations due to stress hormones and inflammatory responses. Your doctor needs to understand your baseline control to anticipate how the infection and antibiotic treatment might impact your diabetes management. This may prompt recommendations for more frequent glucose monitoring during your illness.
Key information to share includes:
Complete list of all medications, including over-the-counter drugs and supplements
Any history of antibiotic allergies or adverse reactions
Current diabetes control and recent A1C results
Presence of diabetes complications, particularly gastroparesis
Any upcoming procedures or schedule changes that might affect medication timing
If you experience severe vomiting or diarrhea during antibiotic treatment that prevents you from taking oral medications or maintaining hydration, contact your healthcare provider promptly. These situations may require temporary adjustments to your diabetes management plan, including possibly holding tirzepatide temporarily until oral intake and hydration improve.
Seek urgent medical attention if you develop persistent severe abdominal pain (especially if radiating to the back), with or without vomiting, as these could be symptoms of pancreatitis—a rare but serious potential complication of GLP-1 based therapies. Similarly, report symptoms of gallbladder disease, which can occur with weight loss medications.
Continue taking tirzepatide as prescribed during antibiotic treatment unless your healthcare provider specifically instructs otherwise. The medication's once-weekly dosing schedule should be maintained on your regular injection day. There is no need to adjust the timing of your tirzepatide dose relative to antibiotic administration, as no timing-dependent interactions have been established.
Increase the frequency of blood glucose monitoring during acute illness and antibiotic treatment. Infections commonly cause elevated blood glucose levels through stress hormone release (cortisol, epinephrine) and increased insulin resistance. During illness, monitor glucose more frequently based on your therapy and symptoms—every 2-4 hours may be appropriate if you use insulin. If your blood glucose exceeds 240 mg/dL, check for ketones, especially if you have type 1 diabetes or are insulin-dependent.
Patients taking tirzepatide with insulin or sulfonylureas should be particularly vigilant about hypoglycemia risk during illness, especially if food intake is reduced. Your healthcare provider may need to temporarily adjust these medications.
Maintain adequate hydration throughout antibiotic treatment, which becomes particularly important if you experience gastrointestinal side effects from either medication. Dehydration can concentrate blood glucose levels and impair kidney function, affecting both diabetes control and medication clearance. Aim for clear or pale yellow urine as an indicator of adequate hydration. If you are experiencing nausea, small frequent sips of water or electrolyte-containing beverages may be better tolerated than large volumes.
Practical management strategies include:
Setting reminders for both tirzepatide injections and antibiotic doses to ensure adherence
Keeping a symptom diary noting glucose readings, medication times, and any adverse effects
Having a sick-day management plan that includes glucose targets, ketone testing, and when to contact your provider
Maintaining adequate carbohydrate intake even if appetite is reduced, using easily digestible options if needed
Contact your healthcare provider if you experience persistent hyperglycemia (blood glucose consistently above 250 mg/dL), positive ketones, signs of diabetic ketoacidosis (excessive thirst, frequent urination, fruity breath odor, confusion), or inability to maintain oral intake due to severe nausea or vomiting. These situations may require temporary adjustments to your diabetes regimen, additional medications, or evaluation for complications.
Remember that if you're taking oral medications with a narrow therapeutic index or oral contraceptives, tirzepatide's effect on gastric emptying may reduce their exposure, particularly after initiation or dose increases of tirzepatide.
Yes, you can take antibiotics while on tirzepatide. The FDA prescribing information does not list specific interactions between tirzepatide and antibiotics, and no dose adjustments are required for either medication.
No, continue taking tirzepatide as prescribed during antibiotic treatment unless your healthcare provider specifically instructs otherwise. There is no need to adjust timing or discontinue tirzepatide based solely on antibiotic use.
Blood sugar changes during antibiotic treatment typically result from the underlying infection causing stress hormone release and increased insulin resistance, rather than from a direct interaction between tirzepatide and antibiotics. Some antibiotics, particularly fluoroquinolones, can also independently affect glucose levels.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.