LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management. A common concern among patients and healthcare providers is whether tirzepatide causes hypoglycemia. Understanding this medication's glucose-dependent mechanism is essential for safe prescribing. Unlike older diabetes drugs such as sulfonylureas or insulin, tirzepatide stimulates insulin release primarily when blood glucose is elevated, significantly reducing intrinsic hypoglycemia risk. However, the clinical context—particularly concurrent medications—plays a crucial role in determining overall safety. This article examines tirzepatide's hypoglycemia profile, risk factors, symptom recognition, and strategies for safe combination therapy.
Quick Answer: Tirzepatide has a low intrinsic risk of causing hypoglycemia when used alone or with medications like metformin or SGLT2 inhibitors, but hypoglycemia risk increases substantially when combined with insulin or sulfonylureas.
Tirzepatide (Mounjaro, Zepbound) is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). Importantly, while Mounjaro treats diabetes, Zepbound is not indicated for glycemic control. This dual-action medication works by enhancing insulin secretion in a glucose-dependent manner, meaning it stimulates insulin release primarily when blood glucose levels are elevated. This mechanism is fundamentally different from older diabetes medications like sulfonylureas or insulin itself.
The glucose-dependent nature of tirzepatide's action is clinically significant for hypoglycemia risk. When blood sugar levels fall into the normal or low range, tirzepatide's stimulation of insulin secretion diminishes accordingly. Additionally, tirzepatide slows gastric emptying, which moderates the rate at which glucose enters the bloodstream after meals, and suppresses glucagon secretion primarily during hyperglycemia. This glucose-dependent glucagon suppression helps prevent high blood sugar without impairing the body's counterregulatory response to hypoglycemia.
Clinical trials in the SURPASS program have demonstrated that tirzepatide effectively reduces hemoglobin A1C levels by approximately 1.6% to 2.4% on average, with effects varying by baseline A1C, dose, and individual response. The medication is administered once weekly via subcutaneous injection, with doses ranging from 2.5 mg (starting dose) up to 15 mg for diabetes management. Understanding how tirzepatide regulates blood sugar through glucose-dependent mechanisms is essential for both healthcare providers and patients when assessing the medication's safety profile, particularly regarding hypoglycemia risk.
When used as monotherapy or with medications that do not independently cause hypoglycemia, tirzepatide has a low intrinsic risk of causing clinically significant hypoglycemia. In pivotal clinical trials (SURPASS program), the incidence of Level 2 hypoglycemia (blood glucose <54 mg/dL) with tirzepatide monotherapy was less than 0.6%, similar to rates observed with placebo. This favorable safety profile stems directly from its glucose-dependent mechanism of action, which inherently limits insulin secretion when blood glucose approaches normal levels.
The FDA prescribing information for tirzepatide confirms that hypoglycemia is not a common adverse effect when the medication is used alone or combined with metformin, SGLT2 inhibitors, or thiazolidinediones—all medications that do not independently cause hypoglycemia. Most adverse effects reported with tirzepatide are gastrointestinal in nature, including nausea (12-22%), diarrhea (12-16%), and vomiting (4-9%), which are generally mild to moderate and decrease over time.
For individuals without diabetes using tirzepatide (Zepbound) for weight management, clinically significant hypoglycemia is rare unless combined with medications that independently lower blood glucose.
However, it is important to distinguish between tirzepatide's intrinsic hypoglycemia risk and the increased risk that occurs when it is combined with insulin or insulin secretagogues (such as sulfonylureas or meglitinides). In these combination scenarios, the risk of hypoglycemia increases substantially—not because of tirzepatide itself, but because these other medications can drive blood sugar below normal levels regardless of glucose concentration. Clinical data show higher hypoglycemia rates when tirzepatide is combined with basal insulin or sulfonylureas. Therefore, while tirzepatide does not inherently cause hypoglycemia, the clinical context and concurrent medications significantly influence overall risk.
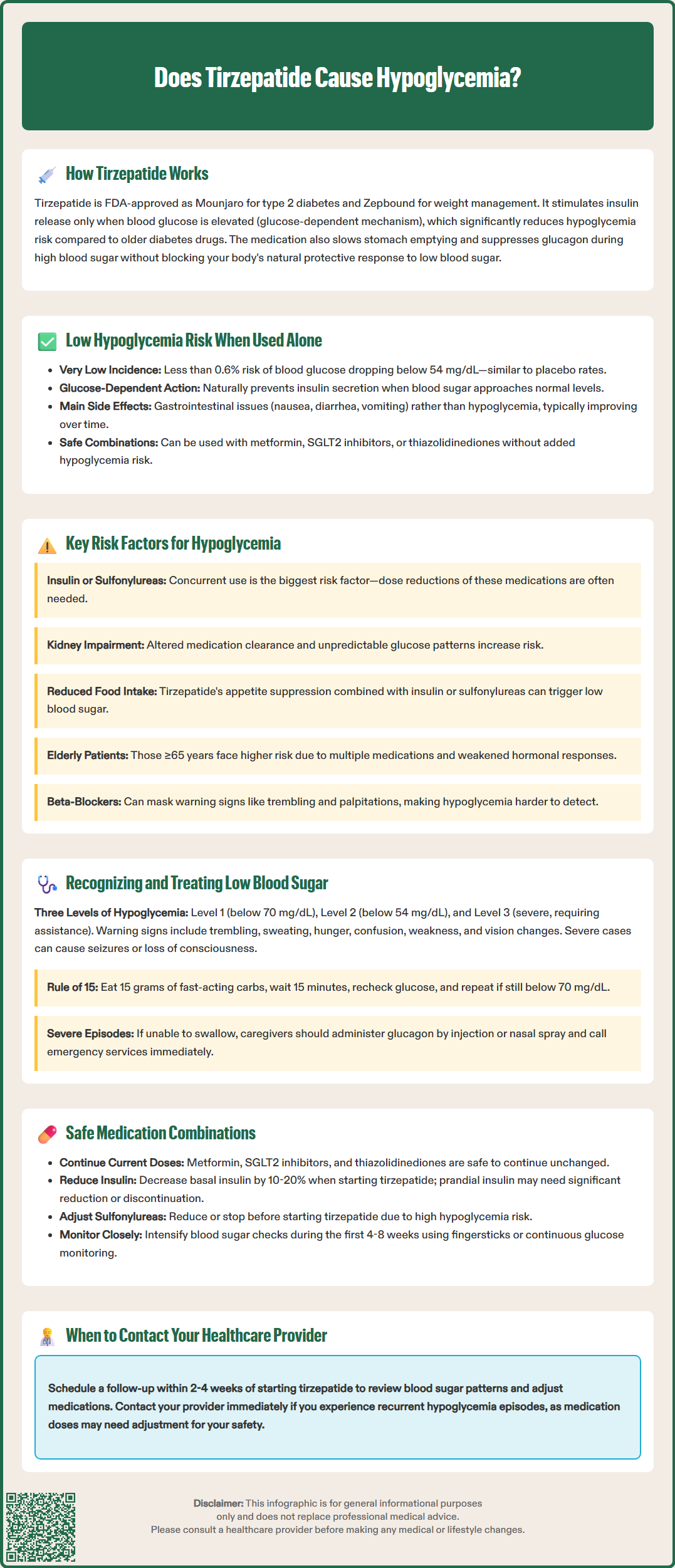
Several patient-specific and medication-related factors can elevate the risk of hypoglycemia in individuals taking tirzepatide. The most significant risk factor is concurrent use of insulin or insulin secretagogues (sulfonylureas like glipizide or glyburide, and meglitinides like repaglinide). These medications stimulate insulin release or provide exogenous insulin independent of glucose levels, creating a pharmacological environment where hypoglycemia becomes more likely. The American Diabetes Association (ADA) guidelines recommend considering dose reduction of these agents when initiating GLP-1 receptor agonists like tirzepatide, with individualization based on A1C and glucose patterns.
Renal impairment represents another important consideration. While tirzepatide can be used across all stages of chronic kidney disease without dose adjustment per FDA labeling, patients with reduced kidney function may have altered clearance of concurrent medications, particularly insulin and sulfonylureas, potentially prolonging their hypoglycemic effects. Additionally, patients with renal disease often have unpredictable glucose patterns and reduced gluconeogenesis capacity, making hypoglycemia recovery more challenging.
Beta-blockers may mask the adrenergic symptoms of hypoglycemia (trembling, palpitations), making early recognition more difficult. Inadequate caloric intake, increased physical activity, or alcohol consumption can precipitate hypoglycemia in any patient with diabetes, but these factors become more relevant when tirzepatide is combined with other glucose-lowering agents. Tirzepatide's appetite-suppressing effects may lead to significantly reduced food intake, which, when combined with insulin or sulfonylureas, creates a mismatch between medication effect and available glucose. Significant gastrointestinal side effects can further reduce intake and potentially affect renal function, increasing hypoglycemia risk.
Elderly patients (≥65 years) may have increased vulnerability due to polypharmacy, irregular eating patterns, and diminished counterregulatory responses to hypoglycemia. Finally, hepatic impairment can affect gluconeogenesis and medication metabolism, though tirzepatide itself does not require dose adjustment in liver disease. Healthcare providers should carefully assess these risk factors before initiating tirzepatide and adjust concurrent diabetes medications accordingly.
Hypoglycemia is classified according to ADA guidelines as: Level 1 (<70 mg/dL and ≥54 mg/dL), Level 2 (<54 mg/dL), and Level 3 (severe hypoglycemia requiring assistance from another person, regardless of glucose value). Early recognition of hypoglycemic symptoms is crucial for prompt intervention and prevention of severe episodes. Common symptoms include:
Autonomic symptoms: Trembling, palpitations, sweating, anxiety, hunger, and tingling sensations
Neuroglycopenic symptoms: Difficulty concentrating, confusion, weakness, drowsiness, vision changes, difficulty speaking, and headache
Severe symptoms: Seizures, loss of consciousness, or inability to self-treat
Patients taking tirzepatide with insulin or sulfonylureas should be educated to recognize these warning signs and respond appropriately. Some individuals, particularly those with longstanding diabetes or recurrent hypoglycemia, may develop hypoglycemia unawareness—a dangerous condition where autonomic warning symptoms are diminished or absent, allowing blood sugar to drop to dangerous levels without recognition.
Immediate management follows the "Rule of 15": consume 15 grams of fast-acting carbohydrate (4 glucose tablets, 4 ounces of fruit juice, or 1 tablespoon of honey), wait 15 minutes, and recheck blood glucose. If levels remain below 70 mg/dL, repeat the treatment. Once blood glucose normalizes, if the next meal is more than 1-2 hours away, consume a snack containing protein and complex carbohydrates to prevent recurrence. For patients taking alpha-glucosidase inhibitors, pure glucose (glucose tablets or gel) should be used rather than sucrose-containing foods.
Patients should avoid driving until blood glucose has normalized and symptoms have resolved completely.
Severe hypoglycemia requires emergency intervention. Family members and caregivers should be trained to administer glucagon via injection (Gvoke, Zegalogue) or nasal spray (Baqsimi) if the patient is unconscious or unable to swallow safely. Emergency medical services should be contacted immediately. Patients experiencing recurrent hypoglycemia should contact their healthcare provider promptly for medication adjustment—this typically involves reducing insulin or sulfonylurea doses rather than discontinuing tirzepatide, which provides important glycemic and weight benefits.
Optimizing tirzepatide therapy requires careful consideration of concurrent diabetes medications to minimize hypoglycemia risk while maintaining glycemic control. The FDA label and clinical practice guidelines provide specific recommendations for safe combination therapy based on the hypoglycemia risk profile of each medication class.
Low-risk combinations include tirzepatide with metformin, SGLT2 inhibitors (empagliflozin, dapagliflozin, canagliflozin), or thiazolidinediones (pioglitazone). These medications do not independently cause hypoglycemia and can be continued at current doses when initiating tirzepatide. Metformin, in particular, is often maintained as foundational therapy due to its low cost, weight neutrality, and long-term clinical experience. SGLT2 inhibitors offer additional cardiovascular and renal protection, making them valuable combination partners.
High-risk combinations requiring dose adjustment include insulin and sulfonylureas. When adding tirzepatide to existing insulin therapy, consider an initial 10-20% reduction in basal insulin dose, with greater reductions (up to 20-30%) for patients with A1C levels near target. Prandial insulin often requires significant reduction or discontinuation when adding tirzepatide, as the incretin effect and delayed gastric emptying substantially reduce postprandial glucose excursions. For sulfonylureas, dose reduction or discontinuation should be strongly considered before initiating tirzepatide, as these medications provide diminishing benefit when combined with more effective agents and substantially increase hypoglycemia risk.
Monitoring strategies should be intensified during the first 4-8 weeks after initiating tirzepatide or adjusting doses. Patients on insulin should develop an individualized self-monitoring of blood glucose (SMBG) plan, including fasting, pre-meal, and bedtime readings, with additional checks if hypoglycemia symptoms occur. Those using continuous glucose monitoring (CGM) should review trend data regularly and adjust alert thresholds to provide early warning of declining glucose levels. Healthcare providers should schedule follow-up within 2-4 weeks of starting tirzepatide to review glucose patterns, assess tolerability, and make necessary medication adjustments. This proactive approach ensures that patients receive the metabolic benefits of tirzepatide while minimizing hypoglycemia risk through appropriate medication management.
When used as monotherapy, tirzepatide has a very low risk of causing clinically significant hypoglycemia (less than 0.6% incidence), similar to placebo, due to its glucose-dependent mechanism of action that limits insulin secretion when blood sugar approaches normal levels.
Yes, when adding tirzepatide to existing insulin therapy, healthcare providers typically recommend an initial 10-20% reduction in basal insulin dose to minimize hypoglycemia risk. Prandial insulin often requires significant reduction or discontinuation, and adjustments should be individualized based on glucose monitoring.
Follow the Rule of 15: consume 15 grams of fast-acting carbohydrate (such as 4 glucose tablets or 4 ounces of fruit juice), wait 15 minutes, and recheck blood glucose. If levels remain below 70 mg/dL, repeat the treatment and contact your healthcare provider if hypoglycemia occurs frequently.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.