LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is an FDA-approved GLP-1 receptor agonist used to treat type 2 diabetes and manage chronic weight in adults with obesity. While gastrointestinal side effects like nausea and diarrhea are well-documented, some patients report experiencing leg cramps during treatment. Although leg cramps are not listed as an official adverse effect in FDA prescribing information, understanding the potential indirect mechanisms—including dehydration, electrolyte imbalances, and nutritional changes—can help patients and clinicians address this symptom effectively while continuing therapy.
Quick Answer: Leg cramps are not listed as an official side effect of semaglutide in FDA labeling, but may occur indirectly through dehydration, electrolyte imbalances, or nutritional changes associated with treatment.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity. Marketed under brand names including Ozempic, Wegovy, and Rybelsus, semaglutide works by mimicking the action of the naturally occurring hormone GLP-1, which enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and promotes satiety. Semaglutide is not indicated for the treatment of type 1 diabetes.
The most commonly reported adverse effects of semaglutide are gastrointestinal in nature, reflecting its mechanism of action on the digestive system. According to FDA prescribing information, these include nausea, vomiting, diarrhea, abdominal pain, and constipation. These symptoms typically occur during dose initiation or escalation and often diminish over time as the body adjusts to the medication.
Other documented adverse effects include injection site reactions, fatigue, dizziness, and headache. More serious but less common risks include pancreatitis, gallbladder disease, acute kidney injury (particularly in the setting of dehydration from gastrointestinal symptoms), and hypoglycemia when used in combination with insulin or insulin secretagogues. Postmarketing reports have identified cases of intestinal obstruction and ileus.
Diabetic retinopathy complications may occur in patients with pre-existing retinopathy, particularly with rapid improvement in glycemic control. Patients with a history of diabetic retinopathy should be monitored appropriately.
The FDA label includes a boxed warning regarding the risk of thyroid C-cell tumors observed in rodent studies. Semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). For Wegovy specifically, the medication should be discontinued when pregnancy is recognized.
Understanding the established side effect profile of semaglutide provides important context when evaluating less commonly reported symptoms, such as leg cramps, which patients may experience during treatment.
Leg cramps are not listed as a recognized adverse effect in the official FDA prescribing information for semaglutide products. The clinical trials that supported FDA approval did not identify muscle cramps or leg cramps as occurring at a significantly higher rate in semaglutide-treated patients compared to placebo groups. This means there is no established direct causal relationship between semaglutide and leg cramps based on current regulatory documentation.
However, post-marketing surveillance and patient reports suggest that some individuals taking semaglutide do experience leg cramps during treatment. These anecdotal reports have appeared in patient forums, social media discussions, and clinical practice observations. It is important to distinguish between a documented adverse drug reaction and symptoms that may occur coincidentally or through indirect mechanisms during treatment with any medication.
The absence of leg cramps from official labeling does not definitively rule out a connection, as post-marketing experience sometimes reveals adverse effects not detected in pre-approval trials due to sample size limitations, duration of follow-up, or patient population differences. The FDA's Adverse Event Reporting System (FAERS) allows healthcare providers and patients to report suspected adverse events, contributing to ongoing safety monitoring. However, it's important to note that FAERS reports are hypothesis-generating and cannot establish incidence rates or confirm causality.
When evaluating whether semaglutide might be contributing to leg cramps in an individual patient, clinicians must consider the temporal relationship between medication initiation or dose escalation and symptom onset, the presence of alternative explanations, and whether symptoms resolve with dose adjustment or discontinuation. A thorough assessment of other potential causes is essential before attributing leg cramps specifically to semaglutide therapy.
Suspected adverse reactions can be reported to the FDA MedWatch program at www.fda.gov/medwatch or by calling 1-800-FDA-1088.
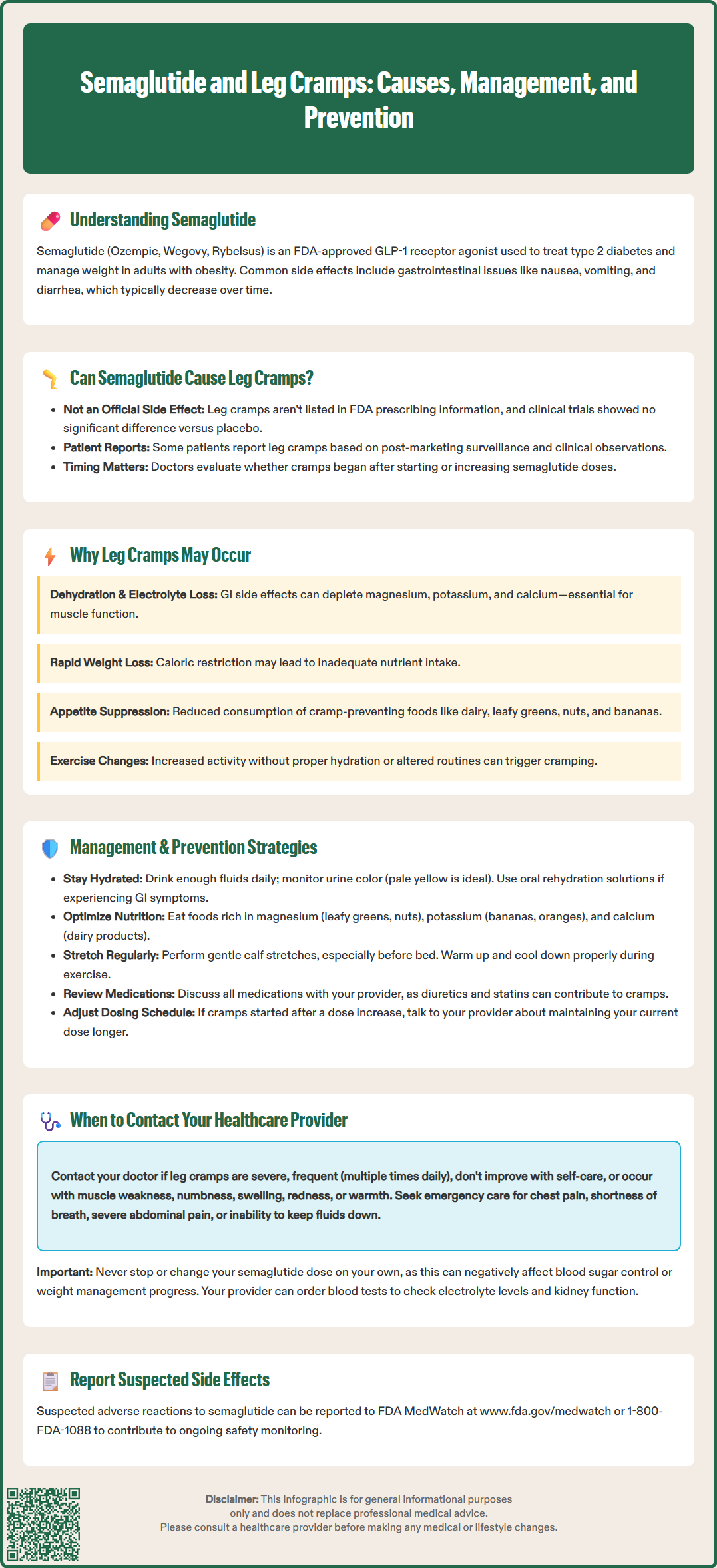
While semaglutide does not directly cause leg cramps through its pharmacological mechanism, several indirect pathways related to its effects and the physiological changes during treatment may potentially contribute to muscle cramping in susceptible individuals.
Dehydration and electrolyte imbalances represent a plausible mechanism. Semaglutide commonly causes gastrointestinal side effects including nausea, vomiting, and diarrhea, particularly during the initial weeks of treatment or following dose increases. These symptoms can lead to reduced fluid intake and increased fluid losses, resulting in dehydration. Additionally, vomiting and diarrhea can deplete essential electrolytes including sodium, potassium, magnesium, and calcium—all of which play critical roles in normal muscle contraction and relaxation. Electrolyte disturbances, particularly hypomagnesemia and hypokalemia, are well-established causes of muscle cramps.
Rapid weight loss associated with semaglutide treatment may also contribute. Patients using semaglutide for weight management often experience significant caloric restriction due to reduced appetite and early satiety. Inadequate nutritional intake, particularly of minerals and vitamins, can predispose individuals to muscle cramps. Furthermore, rapid changes in body composition and fluid distribution during weight loss may temporarily affect muscle function.
Reduced dietary intake may lead to insufficient consumption of cramp-preventing nutrients. Magnesium, potassium, and calcium are commonly obtained through foods that patients may eat less of when experiencing appetite suppression, such as dairy products, leafy greens, nuts, and bananas.
Changes in physical activity patterns during treatment may also play a role. Some patients increase exercise as part of their weight management program, potentially leading to muscle fatigue and cramping if hydration and electrolyte replacement are inadequate. Conversely, fatigue—a reported side effect of semaglutide—might alter activity patterns in ways that affect muscle conditioning.
It is important to note that leg cramps are common in the general population, with up to 60% of adults reporting nocturnal leg cramps. Multiple other causes should be considered including peripheral vascular disease, neuropathy, medication effects from other drugs (particularly diuretics, beta-agonists, and statins), hypothyroidism, pregnancy, and musculoskeletal conditions.
If you experience leg cramps while taking semaglutide, several evidence-based strategies may help manage and prevent these symptoms while continuing treatment.
Optimize hydration status. Ensure adequate daily fluid intake based on your individual needs and thirst. Use urine color as a practical indicator—pale yellow suggests adequate hydration, while dark yellow or amber indicates the need for increased fluid intake. If experiencing significant nausea, vomiting, or diarrhea, consider oral rehydration solutions that contain balanced electrolytes. Patients with kidney disease, heart failure, or other conditions requiring fluid restrictions should follow their healthcare provider's specific guidance on fluid intake.
Address nutritional intake and electrolyte balance. Focus on consuming foods rich in key minerals:
Magnesium: leafy green vegetables, nuts, seeds, whole grains, and legumes
Potassium: bananas, oranges, potatoes, tomatoes, and avocados
Calcium: dairy products, fortified plant-based alternatives, and leafy greens
If dietary intake is limited due to appetite suppression, discuss with your healthcare provider whether supplementation is appropriate. Routine supplementation without documented deficiency is not recommended. Laboratory monitoring of electrolytes may be warranted in specific situations, such as persistent gastrointestinal symptoms, concurrent diuretic use, kidney disease, or older age.
Implement stretching and physical activity modifications. Regular gentle stretching of the calf muscles, particularly before bedtime, may reduce the frequency of nocturnal leg cramps. Avoid sudden increases in exercise intensity, and ensure proper warm-up and cool-down routines. Adequate rest between exercise sessions allows for muscle recovery.
Review all medications. Certain medications can contribute to leg cramps, including loop and thiazide diuretics, beta-agonists, and statins (which more commonly cause diffuse myalgia rather than focal cramps). If you take multiple medications, discuss with your healthcare provider whether any adjustments might be beneficial.
Consider dose adjustment timing. If leg cramps began or worsened after a dose increase, discuss with your provider whether temporarily maintaining the current dose longer before further escalation might allow your body more time to adjust.
Symptomatic relief measures during acute cramps include gentle stretching of the affected muscle, massage, application of heat or cold, and walking to promote circulation. Some patients find relief from warm baths before bedtime.
Important safety note: The FDA advises against using quinine or quinine-containing products (including tonic water) for leg cramps due to serious safety concerns.
While occasional mild leg cramps may not require immediate medical attention, certain features warrant prompt evaluation by your healthcare provider to rule out more serious underlying conditions or complications.
Contact your healthcare provider if you experience:
Severe or persistent cramps that do not respond to self-care measures or significantly impact your quality of life and daily activities
Frequent cramping occurring multiple times daily or nightly, disrupting sleep and functioning
Associated symptoms including muscle weakness, numbness, tingling, or changes in sensation, which may suggest neurological involvement
Swelling, redness, or warmth in the affected leg, which could indicate deep vein thrombosis or other vascular complications
Severe gastrointestinal symptoms with signs of dehydration such as decreased urination, dizziness, confusion, or rapid heartbeat
Cramps that began after starting semaglutide and persist despite adequate hydration and nutritional measures
Seek immediate medical attention (call 911) if you develop:
Chest pain, shortness of breath, or severe abdominal pain
Signs of severe dehydration including inability to keep down fluids, minimal urine output, or altered mental status
Symptoms suggesting acute kidney injury, such as significantly decreased urination, swelling, or confusion
Your healthcare provider can perform a comprehensive evaluation including physical examination, review of your medication regimen, and laboratory testing to assess electrolyte levels, kidney function, and other relevant parameters. Blood tests measuring sodium, potassium, magnesium, calcium, and creatinine can identify correctable abnormalities. Additional investigations such as vitamin D, B12, thyroid function, or creatine kinase levels may be considered based on clinical presentation.
In some cases, temporary dose reduction, slower titration, or additional supportive measures may be recommended to manage symptoms while continuing semaglutide therapy. Never discontinue or adjust your semaglutide dose without consulting your healthcare provider, as abrupt changes may affect glycemic control in diabetes management or weight management progress. A collaborative approach with your healthcare team ensures both symptom management and optimal therapeutic outcomes from semaglutide treatment.
Leg cramps are not listed as a recognized adverse effect in FDA prescribing information for semaglutide. However, some patients report experiencing cramps during treatment, potentially due to indirect factors like dehydration, electrolyte imbalances from gastrointestinal side effects, or nutritional changes associated with reduced appetite.
Maintain adequate hydration, consume foods rich in magnesium, potassium, and calcium, perform regular calf stretching (especially before bedtime), and avoid sudden increases in exercise intensity. If gastrointestinal symptoms are significant, consider oral rehydration solutions to replace lost electrolytes.
Contact your healthcare provider if cramps are severe, frequent, or persistent despite self-care measures, or if accompanied by muscle weakness, numbness, swelling, redness, or signs of dehydration. Laboratory testing may be needed to assess electrolyte levels and kidney function.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.