LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide cause nosebleeds? This question concerns many patients starting Mounjaro or Zepbound for diabetes or weight management. Tirzepatide is a dual GIP and GLP-1 receptor agonist that has transformed treatment for type 2 diabetes and obesity. While the medication has a well-documented side effect profile dominated by gastrointestinal symptoms, nosebleeds are not recognized as an established adverse effect in FDA prescribing information or clinical trial data. Understanding the relationship between tirzepatide and epistaxis helps patients distinguish medication effects from coincidental symptoms and guides appropriate clinical management.
Quick Answer: Nosebleeds are not a recognized side effect of tirzepatide according to FDA prescribing information and clinical trial data.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This medication works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
According to the FDA prescribing information, the most commonly reported adverse effects differ slightly between indications. For Mounjaro (diabetes indication), gastrointestinal effects predominate, including nausea (12-24%), diarrhea (13-22%), decreased appetite (9-11%), vomiting (6-10%), constipation (5-7%), and abdominal pain (5-9%). For Zepbound (obesity indication), similar effects occur but with higher rates of constipation (17-26%) and additional common reactions including dyspepsia, gastroesophageal reflux disease, and hair loss (alopecia). These effects typically occur during dose escalation and often diminish over time.
Other documented side effects include injection site reactions, fatigue, and hypoglycemia (particularly when used with insulin or sulfonylureas). More serious but rare adverse events include pancreatitis, gallbladder disease, acute kidney injury (usually secondary to dehydration), and hypersensitivity reactions. The medication carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Understanding the established side effect profile is essential when evaluating new or unexpected symptoms during treatment. While gastrointestinal effects dominate the adverse event profile, patients and clinicians should remain vigilant for any unusual symptoms that may warrant further evaluation.
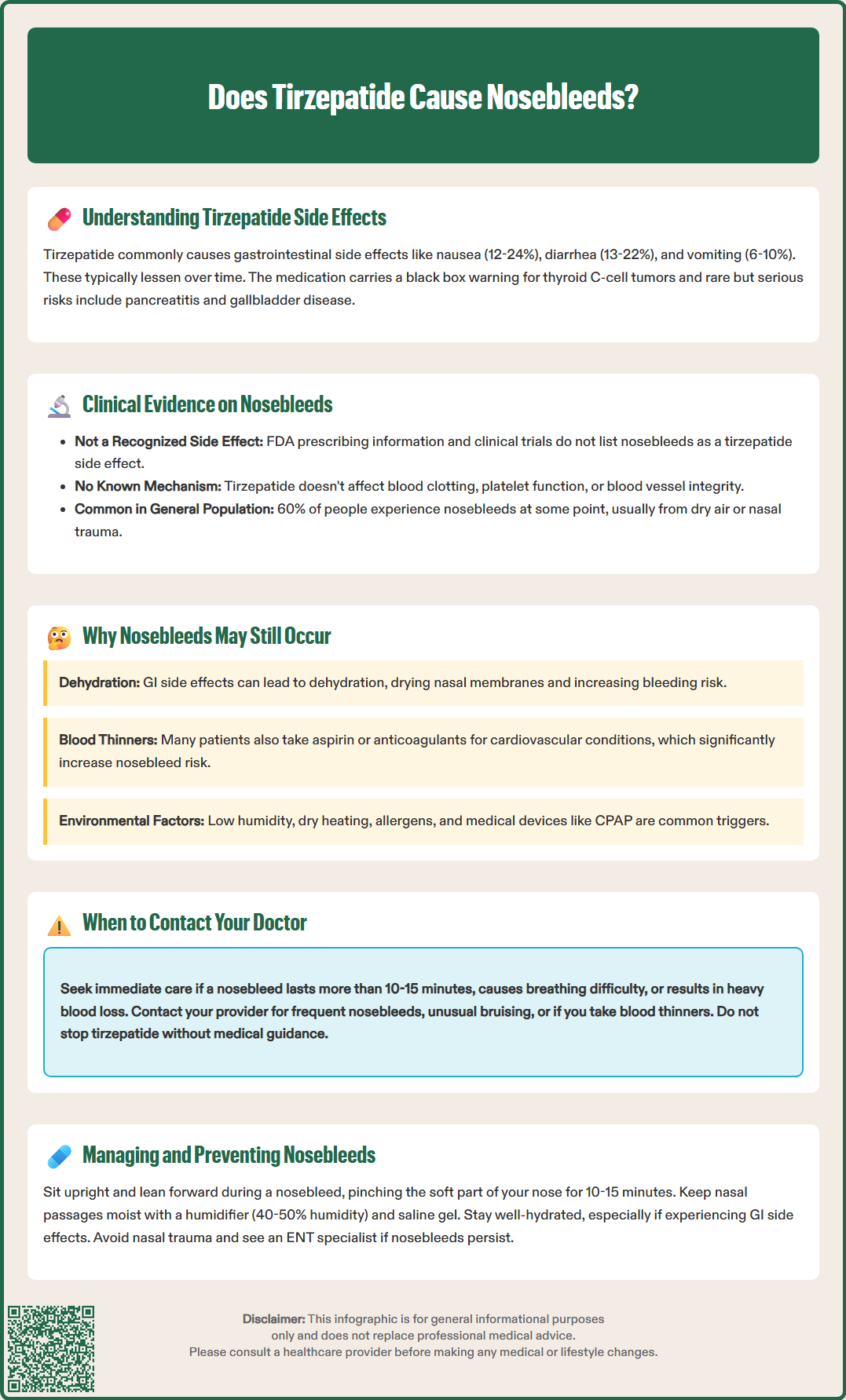
Nosebleeds (epistaxis) are not listed as a recognized or common side effect in the FDA-approved prescribing information for tirzepatide (Mounjaro or Zepbound). Extensive clinical trial data from the SURPASS program (for diabetes) and SURMOUNT trials (for weight management) involving thousands of participants did not identify epistaxis as a significant adverse event associated with tirzepatide use.
There is currently no established pharmacological mechanism by which tirzepatide would directly cause nosebleeds. The medication does not affect platelet function, coagulation pathways, or vascular integrity in ways that would predispose patients to bleeding. Unlike anticoagulants, antiplatelet agents, or certain other medications with known bleeding risks, GLP-1 and GIP receptor agonists do not interfere with normal hemostatic mechanisms.
However, the absence of a documented association does not mean patients taking tirzepatide cannot experience nosebleeds. Epistaxis is a common occurrence in the general population, with approximately 60% of people experiencing at least one nosebleed during their lifetime. Most nosebleeds are benign and result from local factors such as dry air, nasal trauma, or irritation rather than systemic medication effects.
If you experience nosebleeds while taking tirzepatide, it is more likely coincidental or related to other factors rather than a direct drug effect. Nevertheless, any new or concerning symptom during medication therapy warrants appropriate clinical evaluation to rule out other underlying causes and ensure patient safety. Your healthcare provider can help determine whether the nosebleeds require investigation or represent a benign, self-limited condition.
While tirzepatide itself does not directly cause nosebleeds, several indirect factors associated with its use or the treatment context may contribute to epistaxis in some patients. Understanding these potential connections can help identify modifiable risk factors and guide appropriate management.
Dehydration from gastrointestinal side effects represents one plausible indirect mechanism. Tirzepatide commonly causes nausea, vomiting, and diarrhea, particularly during initial treatment and dose escalation. These symptoms can lead to reduced fluid intake and increased fluid losses, resulting in dehydration. Dehydration causes drying of nasal mucous membranes, making them more fragile and susceptible to bleeding. Maintaining adequate hydration is essential for patients experiencing gastrointestinal symptoms.
Concurrent medications and comorbidities often provide alternative explanations for nosebleeds. Many patients taking tirzepatide for diabetes or obesity have cardiovascular comorbidities requiring antiplatelet therapy (aspirin, clopidogrel) or anticoagulation (warfarin, direct oral anticoagulants). These medications significantly increase bleeding risk, including epistaxis. Additionally, patients may use nasal decongestants, corticosteroid nasal sprays, or have underlying conditions such as hypertension that predispose to nosebleeds. Uncontrolled hypertension is a particularly common risk factor for epistaxis.
Environmental factors remain the most common cause of epistaxis regardless of medication use. Low humidity environments, seasonal changes, heating systems during winter months, and nasal irritation from allergens or infections frequently trigger nosebleeds. CPAP or oxygen therapy can also contribute to nasal dryness. These factors should be considered before attributing epistaxis to medication effects.
Medical devices and interventions such as nasogastric tubes, nasal cannulas, or recent nasal procedures may also increase the risk of epistaxis in patients who happen to be taking tirzepatide.
While most nosebleeds are benign and self-limited, certain characteristics warrant prompt medical evaluation. Patients taking tirzepatide should contact their healthcare provider if they experience any of the following concerning features:
Severe or prolonged bleeding requires immediate attention. If a nosebleed continues for more than 10-15 minutes despite appropriate first aid measures (applying a topical vasoconstrictor if available, pinching the soft part of the nose, and leaning forward), seek medical care. Heavy bleeding that fills the mouth or throat, causes difficulty breathing, or results in significant blood loss necessitates emergency evaluation.
Frequent or recurrent nosebleeds merit investigation even if individual episodes are minor. If you experience recurrent episodes despite preventive measures, discuss this with your provider. While unlikely to be medication-related, recurrent epistaxis may indicate underlying conditions requiring evaluation, including hypertension, coagulation disorders, or structural nasal abnormalities.
Associated symptoms that accompany nosebleeds warrant clinical assessment. Contact your provider if nosebleeds occur with unusual bruising, bleeding from other sites (gums, gastrointestinal tract), petechiae (small red spots on skin), severe headaches, visual changes, or signs of anemia (fatigue, pallor, shortness of breath). These features may suggest systemic bleeding disorders or other serious conditions.
Medication interactions should be reviewed. If you take anticoagulants, antiplatelet agents, or other medications affecting hemostasis, inform your provider about any bleeding episodes. Patients on these medications should seek more urgent evaluation for persistent nosebleeds. Dose adjustments or additional monitoring may be necessary.
Your healthcare provider can perform appropriate investigations including blood pressure measurement, complete blood count, coagulation studies if indicated, and nasal examination to identify the cause and guide management. Never discontinue tirzepatide without medical guidance, as the nosebleeds are unlikely to be medication-related and stopping treatment may compromise your diabetes or weight management goals.
Effective management of nosebleeds involves both immediate treatment of acute episodes and preventive strategies to reduce recurrence risk. These approaches are appropriate regardless of medication use and do not require discontinuation of tirzepatide.
Immediate management of acute nosebleeds follows standard first aid principles. Sit upright and lean slightly forward to prevent blood from flowing down the throat. If available and not contraindicated, apply a topical vasoconstrictor such as oxymetazoline (Afrin) to the bleeding nostril. Then pinch the soft part of your nose (not the bony bridge) firmly for 10-15 minutes without releasing pressure to check if bleeding has stopped. Breathe through your mouth during this time. Apply a cold compress to the bridge of the nose to promote vasoconstriction. Avoid lying down, tilting your head back, or packing the nose with tissue, as these actions can worsen bleeding or cause blood to drain into the throat.
Preventive measures focus on maintaining nasal moisture and avoiding trauma. Use a humidifier in your bedroom, particularly during winter months or in dry climates, to maintain ambient humidity between 40-50%. Apply a thin layer of petroleum jelly or saline nasal gel inside the nostrils twice daily to keep mucous membranes moist. Saline nasal sprays used several times daily can also help maintain hydration. Avoid picking or blowing your nose forcefully, and sneeze with your mouth open to reduce nasal pressure.
Optimize hydration status, especially if experiencing gastrointestinal side effects from tirzepatide. Maintain adequate fluid intake to prevent dehydration-related mucosal drying. Rather than following a fixed recommendation, aim for pale yellow urine as a sign of good hydration. If you have heart or kidney disease, follow your healthcare provider's specific fluid intake guidance.
Address modifiable risk factors by reviewing all medications with your healthcare provider, controlling blood pressure if elevated, and avoiding nasal irritants such as tobacco smoke and harsh chemical fumes. If nosebleeds persist despite these measures, your provider may refer you to an otolaryngologist (ENT specialist) for specialized evaluation and potential cauterization of bleeding vessels if a specific bleeding site is identified.
No, nosebleeds (epistaxis) are not listed in the FDA prescribing information for Mounjaro or Zepbound and were not identified as significant adverse events in clinical trials involving thousands of participants.
Yes, gastrointestinal side effects like nausea, vomiting, and diarrhea may lead to dehydration, which can dry nasal mucous membranes and increase susceptibility to nosebleeds. Maintaining adequate hydration is important during treatment.
Contact your healthcare provider if nosebleeds last more than 10-15 minutes despite first aid, occur frequently, or are accompanied by unusual bruising, bleeding from other sites, or signs of anemia.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.