LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide help with autoimmune disease? This question arises as tirzepatide gains attention for its metabolic benefits in type 2 diabetes and weight management. Tirzepatide is a dual GIP and GLP-1 receptor agonist approved by the FDA under the brand names Mounjaro and Zepbound. While emerging research explores potential anti-inflammatory properties of GLP-1 receptor agonists, tirzepatide has no FDA approval for autoimmune conditions such as rheumatoid arthritis, lupus, or inflammatory bowel disease. This article examines tirzepatide's mechanism, approved uses, preliminary evidence on immune function, and established treatment options for autoimmune diseases.
Quick Answer: Tirzepatide is not approved for autoimmune disease treatment and has no established clinical evidence demonstrating efficacy for these conditions.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved for the treatment of type 2 diabetes and chronic weight management. Marketed under the brand names Mounjaro and Zepbound, this medication addresses key metabolic pathways involved in glucose regulation and weight control.
The mechanism of action involves simultaneous activation of both GIP and GLP-1 receptors, which are incretin hormones naturally produced in the gastrointestinal tract. GLP-1 receptor activation enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. The addition of GIP receptor agonism may complement these effects, though the precise contributions of dual receptor activation remain under investigation.
Tirzepatide is administered as a once-weekly subcutaneous injection, with dosing typically initiated at 2.5 mg for 4 weeks, then increased in 2.5 mg increments to a target dose of 5-15 mg based on glycemic control and tolerability. The medication demonstrates substantial efficacy in reducing hemoglobin A1c levels and promoting weight loss, with reductions of up to 21% of body weight observed in clinical trials of patients with obesity without diabetes, and approximately 12-15% in those with type 2 diabetes.
While tirzepatide's primary therapeutic targets are metabolic disorders, emerging research has begun exploring potential secondary effects on inflammatory pathways and immune function. However, it is important to emphasize that tirzepatide is not approved for, nor specifically designed to treat, autoimmune diseases. Any effects on immune function remain investigational and require rigorous clinical evaluation before therapeutic claims can be substantiated.
The US Food and Drug Administration has approved tirzepatide for two distinct but related indications. In May 2022, the FDA approved Mounjaro (tirzepatide) as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. This approval was based on the SURPASS clinical trial program, which demonstrated superior glycemic control compared to placebo, semaglutide 1 mg, and insulin degludec across multiple studies.
In November 2023, the FDA granted approval for Zepbound (tirzepatide) for chronic weight management in adults with obesity (body mass index ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbid condition such as hypertension, dyslipidemia, type 2 diabetes, obstructive sleep apnea, or cardiovascular disease. This indication is supported by the SURMOUNT clinical trial program, which demonstrated substantial and sustained weight reduction.
Key approved indications include:
Type 2 diabetes mellitus management (Mounjaro)
Chronic weight management in obesity or overweight with comorbidities (Zepbound)
Use as adjunct to lifestyle modification (diet and exercise)
It is critical to recognize that tirzepatide has no FDA approval for the treatment, prevention, or management of autoimmune diseases. Conditions such as rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, psoriasis, multiple sclerosis, and other autoimmune disorders are not within the approved therapeutic scope of this medication. There is no established evidence for autoimmune diseases; off-label use should generally be limited to clinical trials or specialist-directed care.
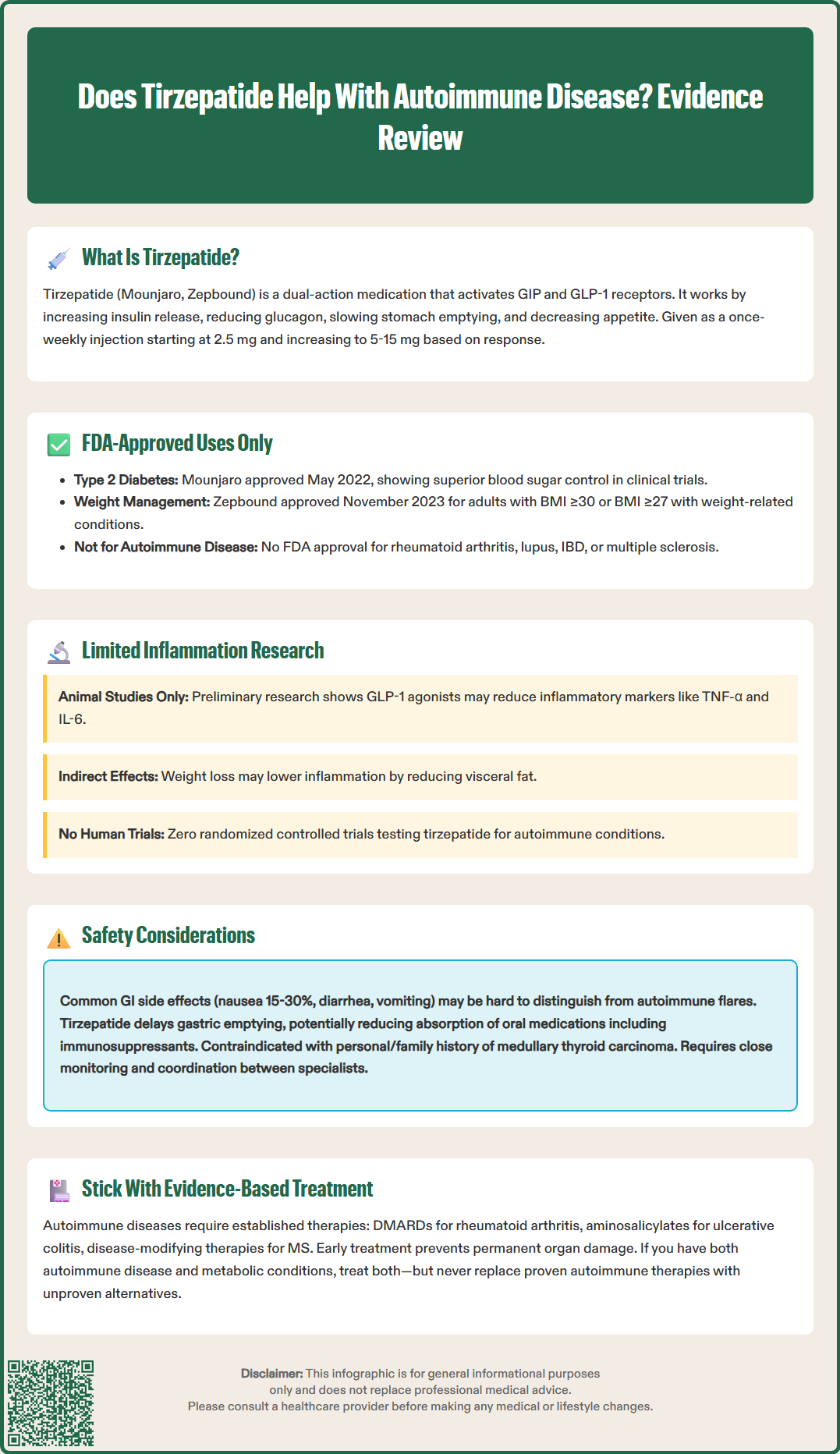
While tirzepatide is not designed or approved for autoimmune disease treatment, preliminary research has identified potential anti-inflammatory properties associated with GLP-1 receptor agonists as a drug class. These observations have generated scientific interest in whether metabolic medications might exert secondary effects on immune function, though substantial uncertainty remains regarding clinical significance.
GLP-1 receptors are expressed not only in pancreatic tissue but also in various immune cells, including macrophages, lymphocytes, and monocytes. Preclinical studies suggest that GLP-1 receptor activation may modulate inflammatory cytokine production, reduce oxidative stress, and influence immune cell trafficking. Some animal models have demonstrated reduced levels of pro-inflammatory markers such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and C-reactive protein following GLP-1 agonist administration.
Important limitations include:
Most evidence derives from preclinical or observational studies
No randomized controlled trials specifically evaluate tirzepatide for autoimmune disease
Mechanisms remain incompletely understood
Clinical translation of anti-inflammatory effects is uncertain
There is currently no established clinical evidence that tirzepatide effectively treats autoimmune diseases. Patients with autoimmune conditions should not consider tirzepatide as a therapeutic option for their underlying immune disorder. Any potential immunomodulatory effects require rigorous investigation through properly designed clinical trials before therapeutic recommendations can be made.
Patients with autoimmune diseases considering tirzepatide for its approved indications (type 2 diabetes or weight management) require careful clinical evaluation and monitoring. While there is no absolute contraindication to tirzepatide use in autoimmune disease, several safety considerations warrant attention.
The most common adverse effects of tirzepatide are gastrointestinal, including nausea (occurring in 15-30% of patients), diarrhea, vomiting, constipation, and abdominal discomfort. These effects are typically dose-dependent, most prominent during dose escalation, and tend to diminish over time. For patients with inflammatory bowel disease (Crohn's disease or ulcerative colitis), distinguishing medication-related gastrointestinal symptoms from disease flares may prove challenging and requires close clinical monitoring. Tirzepatide is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis.
Tirzepatide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies. While human relevance remains uncertain, tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Additional warnings include risks of pancreatitis, hypoglycemia (particularly when combined with insulin or sulfonylureas), acute kidney injury, acute gallbladder disease, diabetic retinopathy complications, and suicidal behavior or ideation (Zepbound).
Tirzepatide delays gastric emptying, which can affect the absorption of oral medications. This is particularly important for oral contraceptives, which may have reduced efficacy; patients should be advised to use non-oral or additional contraceptive methods, especially during dose initiation and escalation. Tirzepatide is not recommended during pregnancy or lactation, and women of reproductive potential should discontinue treatment if pregnancy is recognized.
Specific considerations for autoimmune disease patients:
Delayed gastric emptying may affect absorption of oral medications, including some immunosuppressants
Monitoring challenges in distinguishing disease activity from medication side effects
Importance of maintaining stable immunosuppression regimens
Patients should seek immediate medical attention for severe, persistent abdominal pain (potential pancreatitis or gallbladder disease), vision changes, severe vomiting/dehydration, neck mass/hoarseness, or allergic reactions. Close collaboration between endocrinology and rheumatology or immunology specialists is advisable when managing patients with complex autoimmune conditions requiring metabolic intervention.
Autoimmune diseases encompass a diverse group of conditions characterized by inappropriate immune system activation against self-antigens. Evidence-based management varies substantially depending on the specific autoimmune disorder, disease severity, organ involvement, and individual patient factors. Established therapeutic approaches have demonstrated efficacy through rigorous clinical trials and should remain the foundation of autoimmune disease management.
For rheumatoid arthritis, the American College of Rheumatology recommends disease-modifying antirheumatic drugs (DMARDs) as first-line therapy, with methotrexate being the most commonly prescribed conventional synthetic DMARD. Biologic agents targeting specific inflammatory pathways—including TNF-α inhibitors (adalimumab, etanercept), IL-6 inhibitors (tocilizumab), T-cell costimulation modulators (abatacept), and B-cell depleting agents (rituximab)—provide additional options for patients with inadequate response to conventional therapy. Janus kinase (JAK) inhibitors represent newer targeted synthetic DMARDs with demonstrated efficacy, though they carry boxed warnings regarding serious infections, malignancy, major adverse cardiovascular events, and thrombosis.
Inflammatory bowel disease management differs between ulcerative colitis and Crohn's disease. Aminosalicylates are primarily effective for ulcerative colitis but have limited to no role in Crohn's disease. Both conditions may require corticosteroids for acute flares, immunomodulators (azathioprine, 6-mercaptopurine), and biologic therapies (anti-TNF agents, vedolizumab, ustekinumab) for moderate to severe disease. Multiple sclerosis treatment includes disease-modifying therapies such as interferon beta, glatiramer acetate, and newer oral agents (fingolimod, dimethyl fumarate) or monoclonal antibodies (natalizumab, ocrelizumab).
Core principles of autoimmune disease management:
Early diagnosis and treatment initiation to prevent irreversible organ damage
Regular monitoring of disease activity and treatment response
Multidisciplinary care coordination
Patient education regarding medication adherence and potential adverse effects
Lifestyle modifications including smoking cessation, appropriate exercise, and stress management
Patients with autoimmune diseases and concurrent metabolic conditions such as type 2 diabetes or obesity should receive appropriate treatment for both conditions using evidence-based therapies. Tirzepatide may be considered for its approved metabolic indications in these patients, but it should not replace or delay established autoimmune disease treatments. Any questions regarding the appropriateness of tirzepatide in the context of autoimmune disease should be discussed with qualified healthcare providers familiar with the patient's complete medical history.
No, tirzepatide has no FDA approval for autoimmune disease treatment. It is approved only for type 2 diabetes mellitus and chronic weight management in adults with obesity or overweight with weight-related comorbidities.
Tirzepatide may be used for its approved indications in patients with autoimmune diseases, but requires careful monitoring. Gastrointestinal side effects may complicate disease assessment in conditions like inflammatory bowel disease, and drug interactions with immunosuppressants should be considered.
Evidence-based autoimmune disease treatments include disease-modifying antirheumatic drugs (DMARDs) like methotrexate, biologic agents targeting specific inflammatory pathways (TNF-α inhibitors, IL-6 inhibitors), JAK inhibitors, corticosteroids for acute flares, and immunomodulators. Treatment selection depends on the specific autoimmune condition and disease severity.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.