LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Does tirzepatide affect birth control? This question matters for anyone taking oral contraceptive pills while using tirzepatide (Mounjaro or Zepbound) for type 2 diabetes or weight management. The FDA prescribing information includes specific guidance about potential interactions between tirzepatide and oral contraceptives. Because tirzepatide delays gastric emptying—slowing how quickly food and medications move through your digestive system—it may reduce absorption of birth control pills, particularly during the first weeks of treatment and after dose increases. Understanding this interaction helps ensure reliable contraception while benefiting from tirzepatide therapy.
Quick Answer: Tirzepatide may reduce absorption of oral birth control pills due to delayed gastric emptying, prompting FDA recommendations for backup contraception during initial treatment and dose escalations.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This medication works through multiple complementary mechanisms to improve glycemic control and promote weight loss.
The drug enhances insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it stimulates insulin release only when blood glucose levels are elevated. This mechanism reduces the risk of hypoglycemia when used alone, though this risk increases when tirzepatide is combined with insulin or sulfonylureas. Tirzepatide also suppresses glucagon secretion, which helps prevent the liver from releasing excess glucose into the bloodstream.
Beyond its effects on glucose metabolism, tirzepatide slows gastric emptying, which prolongs the time food remains in the stomach. This delayed gastric emptying contributes to increased satiety and reduced appetite, supporting weight loss efforts. The medication also acts on areas of the brain involved in appetite regulation, further reducing food intake.
Administered as a once-weekly subcutaneous injection, tirzepatide has a half-life of approximately five days, allowing for sustained therapeutic effects. Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which typically diminish over time as the body adjusts to the medication. Understanding how tirzepatide affects digestion and absorption is particularly relevant when considering potential interactions with oral medications, including hormonal contraceptives.
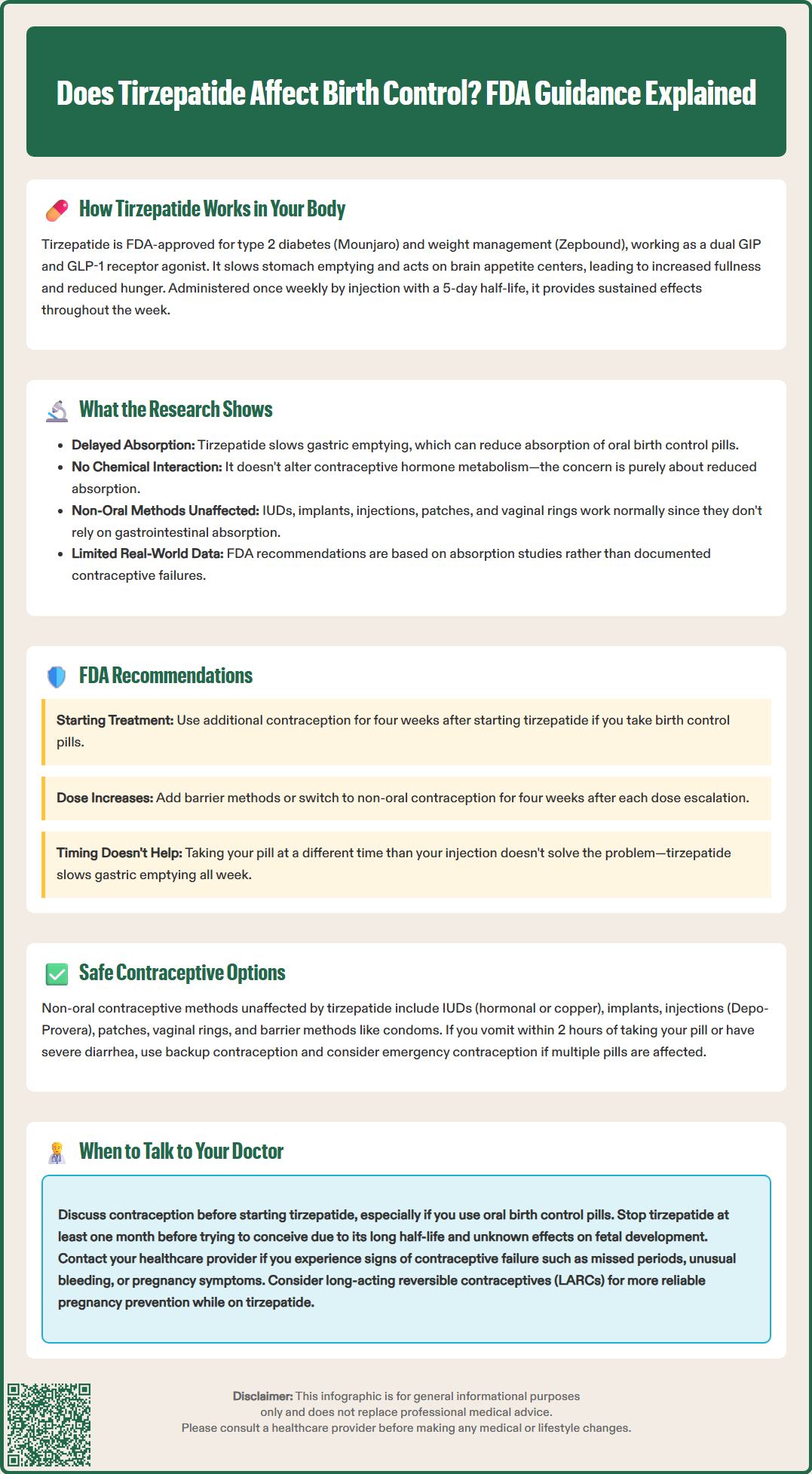
The FDA prescribing information for tirzepatide includes specific guidance regarding oral contraceptive use, reflecting concerns about potential interactions. Because tirzepatide delays gastric emptying, it could affect the absorption of oral medications taken concurrently, including birth control pills. Pharmacokinetic studies have shown reduced exposure to ethinyl estradiol and progestins after tirzepatide initiation, with the greatest effect occurring after initial doses and dose escalations.
Pharmacology studies have demonstrated that tirzepatide's effect on gastric emptying is most pronounced during the first few weeks of treatment and with dose escalations. The FDA label specifically states that for oral hormonal contraceptives (both combined and progestin-only pills), patients should switch to a non-oral contraceptive method or add a barrier method for four weeks after initiation and for four weeks after each dose escalation. This precautionary recommendation aims to ensure contraceptive efficacy during periods when gastric emptying may be most significantly affected.
There is no direct evidence that tirzepatide chemically interacts with hormonal contraceptives or alters their metabolism through hepatic enzyme systems. Unlike some medications that induce or inhibit cytochrome P450 enzymes, tirzepatide does not appear to affect the metabolic pathways responsible for breaking down contraceptive hormones. The concern is purely mechanical—related to absorption rather than metabolism.
Clinical trials of tirzepatide did not specifically evaluate contraceptive failure rates, and real-world data on this interaction remains limited. The precautionary approach recommended by the FDA reflects an abundance of caution rather than documented contraceptive failures. Patients using non-oral contraceptive methods (intrauterine devices, implants, injections, patches, or vaginal rings) are not affected by these absorption concerns, as these methods do not rely on gastrointestinal absorption.
If you are taking oral contraceptive pills and starting tirzepatide or increasing your dose, the FDA recommends implementing additional contraceptive protection. Specifically, you should either switch to a non-oral contraceptive method or add a barrier method (such as condoms) for four weeks after starting tirzepatide and for four weeks following each dose increase. This timeframe allows your body to adjust to the medication's effects on gastric emptying.
Non-oral contraceptive methods offer reliable alternatives that bypass concerns about gastrointestinal absorption entirely. These include:
Long-acting reversible contraceptives (LARCs): Intrauterine devices (hormonal or copper) and subdermal implants provide highly effective contraception without requiring daily administration or gastrointestinal absorption.
Injectable contraceptives: Depot medroxyprogesterone acetate (Depo-Provera) administered every three months offers effective pregnancy prevention independent of digestive function.
Transdermal and vaginal methods: Contraceptive patches and vaginal rings deliver hormones through the skin or vaginal mucosa, avoiding the gastrointestinal tract entirely. Note that the transdermal patch may have reduced efficacy in people with higher body weight (typically >198 pounds).
Barrier methods: Condoms, diaphragms, and cervical caps provide non-hormonal options that can be used alone or in combination with other methods.
If you prefer to continue oral contraceptives, consistent use of barrier methods during the specified risk periods is essential. Taking your birth control pill at a different time of day from your tirzepatide injection does not eliminate the concern, as tirzepatide's effect on gastric emptying persists throughout the week between doses.
If you experience vomiting or severe diarrhea while taking oral contraceptives and tirzepatide, follow CDC guidance for missed pills: use back-up contraception if vomiting occurs within 2 hours of taking a pill, and consider emergency contraception if multiple pills are affected during the first or third week of the pack.
For individuals using tirzepatide for weight management who are not sexually active or who have other reasons pregnancy is not a concern, these precautions may not apply. However, if there is any possibility of pregnancy, following FDA guidance helps ensure contraceptive reliability and prevents unintended pregnancy during treatment.
You should discuss contraception with your healthcare provider before starting tirzepatide if you are of reproductive age and sexually active. This conversation is particularly important if you currently rely on oral contraceptive pills as your primary method of pregnancy prevention. Your doctor can help you evaluate whether switching to an alternative contraceptive method or adding barrier protection is most appropriate for your situation.
Schedule a consultation if you experience any signs of contraceptive failure while taking tirzepatide, including missed periods (if not expected with your contraceptive method), unusual bleeding patterns, or symptoms of early pregnancy such as breast tenderness, nausea beyond what is expected from tirzepatide, or fatigue. While there is no official link between tirzepatide and contraceptive failure, any concerning symptoms warrant medical evaluation.
If you are planning pregnancy, inform your healthcare provider before conception. According to FDA prescribing information, tirzepatide should be discontinued at least one month before a planned pregnancy due to its long half-life and the lack of adequate data on fetal effects. If pregnancy occurs while taking tirzepatide, the medication should be discontinued immediately. Your doctor can help you transition to appropriate diabetes or weight management strategies that are safe during pregnancy planning and can ensure your contraceptive method is appropriate during this transition period.
Additional situations requiring discussion include:
Difficulty tolerating tirzepatide's gastrointestinal effects: Severe or persistent nausea, vomiting, or diarrhea may further complicate oral medication absorption.
Dose escalations: Each time your tirzepatide dose increases, revisit contraceptive protection strategies.
Concerns about contraceptive effectiveness: If you have questions about your current method or experience breakthrough bleeding.
Interest in long-term contraception: Your provider can discuss whether transitioning to a LARC might offer both convenience and certainty.
Breastfeeding considerations: Limited data exists on tirzepatide use during lactation; discuss risks and benefits with your healthcare provider.
Your healthcare team, including your primary care physician, endocrinologist, and gynecologist, can collaborate to ensure both your metabolic health goals and reproductive health needs are appropriately addressed. Open communication about all medications, including contraceptives, helps optimize treatment safety and effectiveness while taking tirzepatide.
Yes, but the FDA recommends using backup contraception (barrier method) or switching to non-oral contraceptives for four weeks after starting tirzepatide and after each dose increase, as delayed gastric emptying may reduce pill absorption.
Non-oral contraceptive methods including IUDs, implants, injections (Depo-Provera), patches, vaginal rings, and barrier methods are all safe with tirzepatide since they do not rely on gastrointestinal absorption.
The FDA recommends using backup contraception or switching to non-oral methods for four weeks after initiating tirzepatide and for four weeks following each dose escalation to ensure contraceptive reliability during periods of maximum gastric emptying effects.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.