LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Weight loss injections, particularly GLP-1 receptor agonists like semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro), have raised questions about potential cancer risks. While rodent studies prompted FDA Boxed Warnings for thyroid C-cell tumors, large-scale clinical trials in humans have not demonstrated increased overall cancer incidence with these medications. Current evidence does not establish a causal relationship between GLP-1-based weight loss injections and most cancers in humans. Understanding the distinction between animal study findings, theoretical concerns, and actual human data is essential for patients and providers making informed treatment decisions.
Quick Answer: Current clinical evidence does not show that weight loss injections cause cancer in humans, though FDA Boxed Warnings exist for thyroid C-cell tumors based on rodent studies.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro)—which is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist—have gained widespread attention for their effectiveness in treating obesity and type 2 diabetes. As their use has expanded, questions about potential cancer risks have emerged, prompting both patients and healthcare providers to seek clarity on the safety profile of these medications.
The concern about cancer risk stems primarily from preclinical animal studies and post-marketing surveillance data. These medications work by mimicking naturally occurring hormones that regulate appetite, slow gastric emptying, and influence insulin secretion. While these mechanisms effectively promote weight loss, their theoretical long-term effects on cellular processes remain an area of ongoing investigation.
It is important to distinguish between theoretical concerns, findings from animal studies, and actual evidence in human populations. The FDA requires extensive safety monitoring for all weight loss medications, and manufacturers must report adverse events, including cancer diagnoses. Current evidence from clinical trials does not establish a causal relationship between these medications and most cancers in humans, though specific warnings exist for certain tumor types, particularly thyroid cancers, based on animal data.
Patients considering or currently using weight loss injections should understand that while some precautionary warnings exist, these medications have undergone rigorous testing and continue to be monitored for safety. The decision to use these treatments should involve a comprehensive discussion of individual risk factors, family history, and the balance between metabolic benefits and potential concerns.
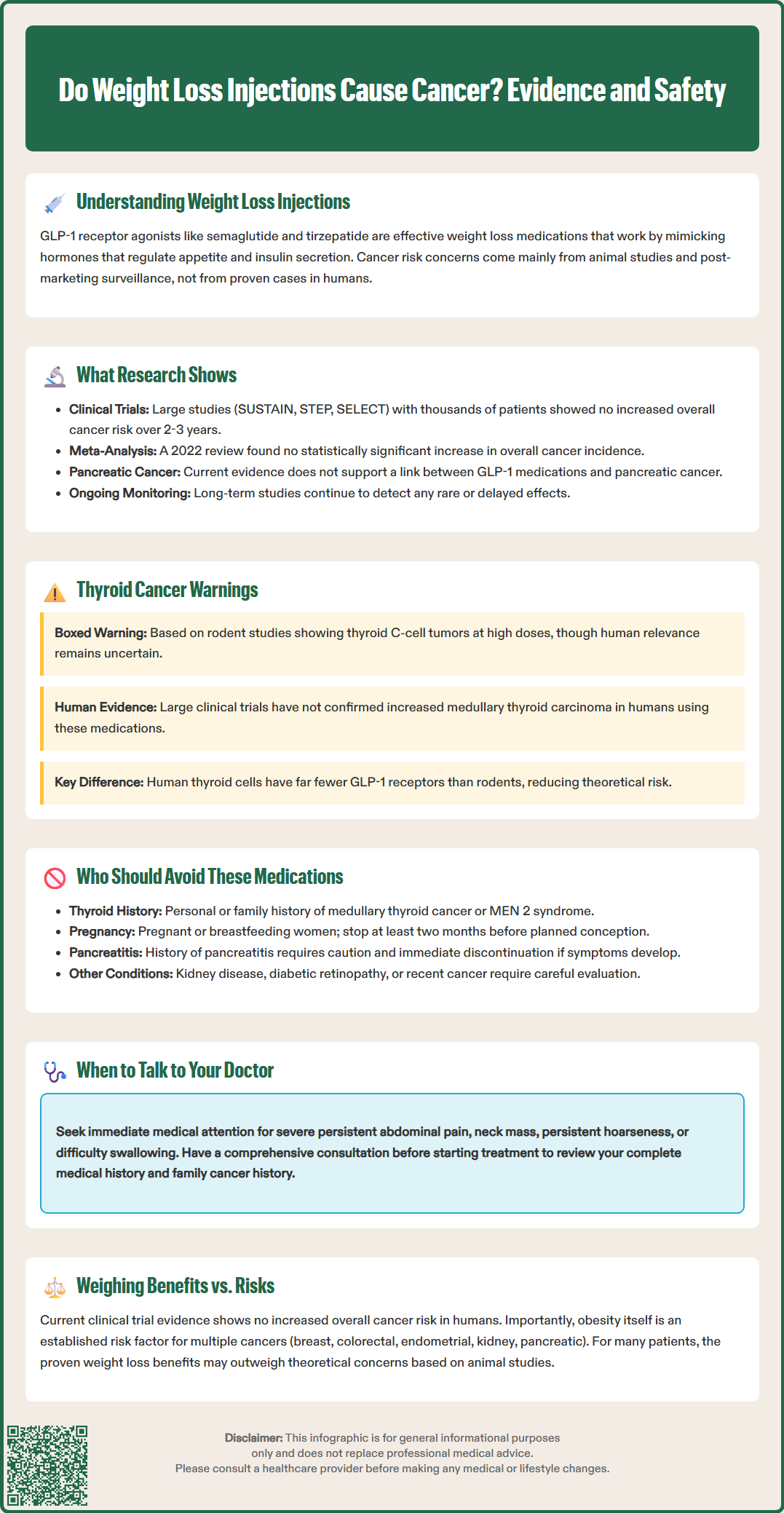
Large-scale clinical trials and real-world studies have examined the relationship between GLP-1-based medications and cancer incidence, though it's important to note these studies were not specifically designed or powered to detect differences in cancer outcomes. The SUSTAIN and STEP trial programs for semaglutide, involving thousands of participants followed for up to two years, did not demonstrate an increased overall cancer risk compared to placebo groups. Similarly, the SELECT cardiovascular outcome trial, which followed over 17,000 patients with obesity but without diabetes for more than three years, found no significant elevation in cancer rates among semaglutide users.
A comprehensive meta-analysis published in 2022 examining data from randomized controlled trials involving GLP-1 receptor agonists found no statistically significant increase in overall cancer incidence. These findings provide some reassurance regarding the general cancer safety profile of this drug class in human populations, though the limited duration of most studies must be acknowledged when interpreting these results.
However, research has identified specific areas requiring continued vigilance. Rodent studies demonstrated an increased incidence of thyroid C-cell tumors (medullary thyroid carcinoma) at doses proportionally higher than those used in humans. While the relevance of these findings to human risk remains uncertain due to differences in receptor expression between species, they prompted the inclusion of Boxed Warnings on medication labels. Post-marketing surveillance has also examined potential associations with pancreatic cancer, given the pancreatic effects of these medications, though current evidence does not support a causal relationship.
Ongoing pharmacovigilance studies continue to monitor long-term cancer outcomes as these medications are used by increasingly diverse populations over extended periods. The American Diabetes Association and American Association of Clinical Endocrinologists acknowledge the current evidence base while emphasizing the need for continued post-marketing surveillance to detect rare or delayed adverse effects that may not emerge in clinical trials of limited duration.
The FDA maintains rigorous oversight of weight loss medications through pre-approval clinical trials, post-marketing surveillance systems, and periodic safety reviews. For GLP-1-based medications approved for weight management, the FDA has reviewed extensive safety data encompassing both short-term and intermediate-term outcomes. The agency's Adverse Event Reporting System (FAERS) continuously collects reports of adverse events, including cancer diagnoses, among patients using these medications, though such reports do not establish causation.
Regarding cancer specifically, the current FDA-approved prescribing information for these medications does not indicate a broad cancer risk in humans beyond the Boxed Warning for thyroid C-cell tumors based on rodent data. The FDA notes that cancer diagnoses reported during treatment may reflect detection of pre-existing malignancies or represent background incidence rates rather than drug-induced tumors, particularly given the relatively short duration of most treatment courses compared to typical cancer development timelines.
The FDA requires specific warnings in prescribing information based on animal study findings and theoretical concerns. For semaglutide, tirzepatide, and most long-acting GLP-1 receptor agonists, labels contain a Boxed Warning about thyroid C-cell tumor findings in rodents and contraindications for patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). These warnings reflect a precautionary approach based on animal data rather than confirmed human risk.
Manufacturers are required to report serious adverse events to the FDA, while healthcare providers and patients are encouraged to voluntarily submit reports through the MedWatch program. This ongoing surveillance system allows the FDA to identify potential safety signals that may not have been apparent in pre-approval trials. The agency periodically updates prescribing information and issues safety communications when new evidence warrants changes to clinical practice recommendations.
GLP-1-based agents indicated for chronic weight management (semaglutide [Wegovy] and tirzepatide [Zepbound]) carry an FDA Boxed Warning—the agency's most serious safety alert—regarding the risk of thyroid C-cell tumors. Most long-acting GLP-1 receptor agonists (including semaglutide, liraglutide, and dulaglutide) also carry this warning, though not every short-acting agent does. This warning stems from studies in rodents where these medications caused dose-dependent and treatment-duration-dependent increases in thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), at clinically relevant exposures.
Medullary thyroid carcinoma is a rare form of thyroid cancer originating from parafollicular C-cells, which produce calcitonin. In rodents, GLP-1 receptors are expressed on thyroid C-cells, and chronic stimulation may promote cellular proliferation. However, the relevance of these findings to humans remains uncertain because human thyroid C-cells express GLP-1 receptors at much lower levels than rodent C-cells, suggesting potentially different susceptibility to GLP-1-mediated effects.
Observational data regarding thyroid cancer risk in humans using these medications have been mixed, and the human risk remains uncertain. Large clinical trials have not confirmed an increased incidence of medullary thyroid carcinoma in humans using GLP-1 medications, though these trials were not designed specifically to assess this rare outcome. The FDA maintains the warning as a precautionary measure given the seriousness of the animal findings and the relatively limited duration of human exposure data.
Patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2)—a genetic condition associated with increased MTC risk—should not use these medications. Healthcare providers should obtain a thorough personal and family history of thyroid disorders before prescribing. Patients who develop symptoms such as a neck mass, persistent hoarseness, or difficulty swallowing should be promptly referred to an endocrinologist or otolaryngologist for evaluation. Routine calcitonin monitoring or thyroid ultrasound screening is not recommended for asymptomatic patients without risk factors, as this approach has not been shown to improve outcomes and may lead to unnecessary interventions for benign findings.
Certain individuals should not use GLP-1-based medications for weight loss due to established contraindications or increased safety concerns. Absolute contraindications include a personal history of medullary thyroid carcinoma, family history of medullary thyroid carcinoma, or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Patients with a known hypersensitivity to semaglutide, tirzepatide, or any component of these formulations should also avoid these medications.
Individuals with a history of pancreatitis should use these medications with caution, and treatment should be promptly discontinued if pancreatitis is suspected. While current evidence does not establish a definitive link between GLP-1-based medications and pancreatic cancer, patients with a history of pancreatic neoplasms may warrant alternative weight management approaches. Healthcare providers should carefully evaluate the risk-benefit ratio in these situations, considering the metabolic benefits against theoretical concerns.
Pregnant or breastfeeding women should not use weight loss injections, as safety data in these populations are limited. Women of childbearing potential should use effective contraception during treatment. For semaglutide specifically, the FDA prescribing information recommends discontinuation at least two months before planned conception due to the long half-life of the drug. For tirzepatide, the prescribing information does not specify a preconception interval but advises discontinuation when pregnancy is recognized. These recommendations should be discussed with a healthcare provider for individualized guidance.
Additional populations requiring careful consideration include patients with kidney disease (specific recommendations vary by medication), those with a history of diabetic retinopathy (particularly if rapidly improving glycemic control), and individuals with active or recent malignancy. While these medications are not absolutely contraindicated in these groups, the decision to prescribe should involve thorough discussion of individual circumstances, close monitoring, and consideration of alternative treatments. Patients should disclose their complete medical history, including all cancer diagnoses, to ensure appropriate treatment selection.
Open communication with your healthcare provider about cancer concerns is essential when considering weight loss injections. Before starting treatment, schedule a comprehensive consultation to review your personal and family medical history, including any cancer diagnoses, thyroid disorders, or genetic conditions that may increase cancer risk. Bring a list of all current medications, supplements, and any previous adverse reactions to medications.
Key questions to discuss with your provider include: What is my individual cancer risk based on my medical and family history? Are there specific cancer types I should be more concerned about with these medications? What symptoms should prompt me to seek immediate medical attention? How will you monitor me during treatment, and what follow-up is recommended? Understanding that current evidence from clinical trials does not show increased overall cancer risk in humans can help contextualize the Boxed Warnings, which are based primarily on animal studies.
Your healthcare provider should explain the distinction between theoretical risks, animal study findings, and actual human evidence. They should also discuss the potential health benefits of weight loss, as obesity itself is an established risk factor for multiple cancer types, including breast, colorectal, endometrial, kidney, and pancreatic cancers. While definitive causal reduction in cancer risk with GLP-1 therapies is not established, the cardiovascular and metabolic benefits of significant weight loss may outweigh theoretical cancer concerns for many patients.
If you develop concerning symptoms during treatment, contact your healthcare provider promptly. Seek immediate medical attention for severe persistent abdominal pain (which could suggest pancreatitis). Symptoms such as a neck mass, persistent hoarseness, or difficulty swallowing warrant urgent referral to an endocrinologist or ear, nose, and throat specialist. Regular follow-up appointments allow for ongoing assessment of treatment response, side effects, and any new symptoms. Patients should feel empowered to ask questions, express concerns, and participate actively in shared decision-making regarding their weight management treatment plan.
The FDA Boxed Warning for GLP-1 medications like semaglutide and tirzepatide is based on rodent studies showing thyroid C-cell tumors, though the relevance to humans remains uncertain. Patients with personal or family history of medullary thyroid carcinoma or MEN 2 syndrome should not use these medications.
Large-scale clinical trials, including the SELECT cardiovascular outcome trial with over 17,000 participants, have not demonstrated increased overall cancer incidence with these medications compared to placebo groups.
Seek immediate medical attention for severe persistent abdominal pain, which could indicate pancreatitis. Contact your provider promptly for neck mass, persistent hoarseness, or difficulty swallowing, which warrant specialist referral.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.