LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Weight loss injections like semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro) have transformed obesity treatment, but many patients wonder about their impact on liver health. These glucagon-like peptide-1 (GLP-1) receptor agonists work by mimicking natural hormones to reduce appetite and promote weight loss. Understanding how these medications interact with the liver is essential for safe use. Clinical evidence suggests these injections have a favorable hepatic safety profile and may even benefit certain liver conditions. However, knowing potential risks, warning signs, and who should avoid these treatments ensures informed decision-making between patients and healthcare providers.
Quick Answer: Weight loss injections like semaglutide and tirzepatide generally do not cause liver damage and may improve liver health in patients with fatty liver disease.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections primarily include glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy, Ozempic) and tirzepatide (Zepbound, Mounjaro), which is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. These medications work through multiple physiological mechanisms to promote weight reduction by mimicking naturally occurring incretin hormones.
The primary mechanism involves binding to receptors in the pancreas, brain, and gastrointestinal tract. In the pancreas, these agents enhance glucose-dependent insulin secretion while suppressing inappropriate glucagon release, improving glycemic control without causing hypoglycemia in most patients. Centrally, they act on hypothalamic appetite centers to increase satiety and reduce food intake. They also slow gastric emptying, prolonging the feeling of fullness after meals and reducing overall caloric consumption.
These medications are administered subcutaneously, typically once weekly for most formulations. After injection, the active compound enters systemic circulation and distributes throughout the body. The liver plays a role in the overall metabolic response to these agents, though improvements in insulin sensitivity are largely secondary to weight loss and improved glycemic control. Importantly, these medications are primarily eliminated through proteolytic degradation rather than hepatic metabolism, which has implications for their safety profile in patients with liver conditions.
Clinical trials have demonstrated average weight loss of 15-22% of body weight over 68-72 weeks with semaglutide and tirzepatide, significantly exceeding results from lifestyle modification alone. In the United States, Wegovy and Zepbound are FDA-approved for chronic weight management, while Ozempic and Mounjaro are indicated for type 2 diabetes. Understanding how these medications interact with hepatic function is essential for appropriate patient selection and monitoring.
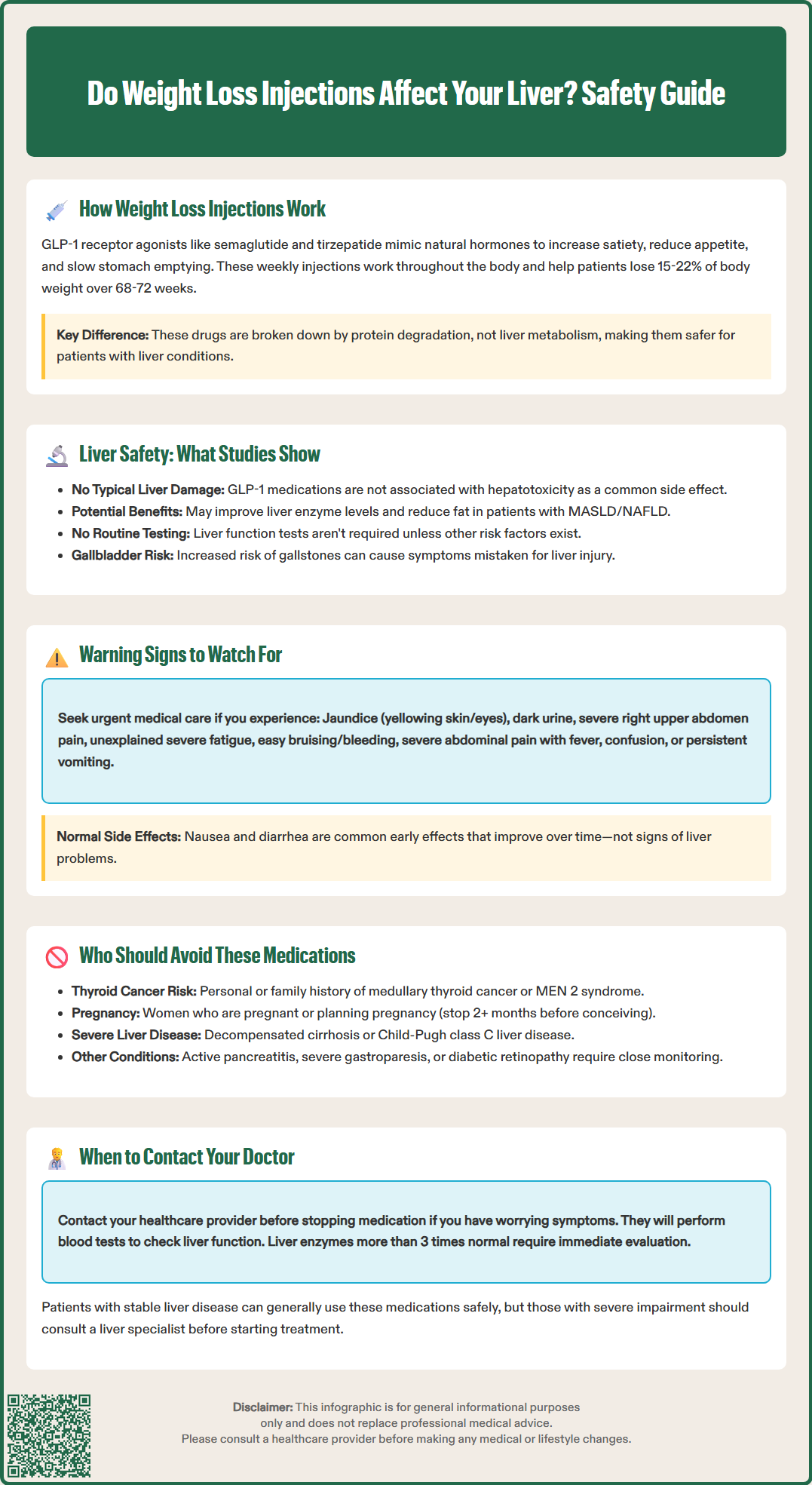
Extensive clinical research has evaluated the hepatic safety profile of GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists, with generally reassuring findings. Large-scale randomized controlled trials and post-marketing surveillance data indicate that these medications do not typically cause clinically significant liver injury in most patients. The FDA-approved prescribing information for semaglutide and tirzepatide does not list hepatotoxicity as a common adverse effect.
Emerging evidence suggests potential hepatoprotective benefits, particularly in patients with metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease (NAFLD). Multiple studies have demonstrated improvements in liver enzyme levels and hepatic steatosis in patients treated with these agents. A 2021 phase 2 trial published in The New England Journal of Medicine showed that semaglutide significantly improved NASH resolution but did not achieve statistically significant improvement in fibrosis stage compared to placebo.
Routine liver function monitoring is not specifically required by FDA labels for patients on these medications unless other risk factors are present. However, clinicians should maintain appropriate vigilance, as isolated cases of elevated transaminases have been reported in post-marketing surveillance.
An important consideration is the increased risk of gallbladder disease, including cholelithiasis and cholecystitis, associated with these medications and rapid weight loss in general. These gallbladder complications can cause right upper quadrant pain and abnormal liver function tests that may mimic hepatic injury.
Patients with pre-existing liver disease, including compensated cirrhosis, can generally use these medications safely, though careful clinical judgment is warranted. There is limited data on use in patients with decompensated cirrhosis or severe hepatic impairment (Child-Pugh class C), and consultation with hepatology specialists is advisable in these cases. The overall evidence supports a favorable hepatic safety profile for weight loss injections in appropriately selected patients.
While serious liver complications from GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists are uncommon, patients and healthcare providers should remain alert to potential warning signs that warrant medical evaluation. Early recognition of hepatic dysfunction allows for timely intervention and appropriate management decisions.
Key symptoms that may indicate liver problems include:
Jaundice: Yellowing of the skin or whites of the eyes, indicating elevated bilirubin levels
Dark urine: Tea-colored or cola-colored urine, particularly when accompanied by pale stools
Persistent abdominal pain: Especially right upper quadrant discomfort that doesn't resolve
Unexplained fatigue: Severe tiredness disproportionate to activity level
Nausea and vomiting: Persistent symptoms not attributable to the medication's known gastrointestinal effects
Loss of appetite: Beyond the expected appetite suppression from the medication
Easy bruising or bleeding: Suggesting impaired hepatic synthesis of clotting factors
Urgent medical attention is needed for:
Severe right upper quadrant pain with fever
Confusion or disorientation
Rapidly worsening jaundice
Persistent vomiting
It's important to distinguish between the common gastrointestinal side effects of these medications—such as nausea, vomiting, and diarrhea, which typically occur early in treatment and improve over time—and symptoms potentially indicating hepatic dysfunction. The former are expected pharmacological effects related to delayed gastric emptying, while the latter represent potential safety concerns requiring investigation.
Patients experiencing any concerning symptoms should contact their healthcare provider promptly rather than discontinuing medication independently. Clinical evaluation should include a thorough history, physical examination, and laboratory assessment including comprehensive metabolic panel with liver function tests (AST, ALT, alkaline phosphatase, bilirubin, albumin, and prothrombin time/INR). Significant elevations in transaminases (typically >3 times the upper limit of normal) or any elevation accompanied by symptoms warrant careful evaluation and possible medication discontinuation pending further assessment. Concurrent elevation of ALT/AST >3× upper limit of normal with bilirubin >2× upper limit of normal (Hy's law) is particularly concerning and requires immediate drug cessation and specialist evaluation.
While GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists have demonstrated safety in diverse patient populations, certain individuals should avoid these medications or use them only with extreme caution under specialized supervision. Careful patient selection optimizes safety outcomes and minimizes potential complications.
Absolute contraindications include:
Personal or family history of medullary thyroid carcinoma: These medications carry a boxed warning regarding thyroid C-cell tumors based on rodent studies
Multiple endocrine neoplasia syndrome type 2 (MEN 2): Increased risk of medullary thyroid carcinoma
Previous serious hypersensitivity reaction: To semaglutide, tirzepatide, or any formulation component
Pregnancy considerations: These medications are not recommended during weight management in pregnancy due to limited safety data and potential fetal risks. Patients should discontinue treatment when pregnancy is recognized. Due to the long half-life of these medications, women planning pregnancy should consider stopping treatment at least 2 months before planned conception.
Relative contraindications and special populations requiring careful consideration:
Patients with severe hepatic impairment (Child-Pugh class C) should generally avoid these medications due to insufficient safety data. Those with decompensated cirrhosis, characterized by ascites, hepatic encephalopathy, or variceal bleeding, require alternative weight management approaches. The physiological stress of rapid weight loss may exacerbate hepatic decompensation in vulnerable patients.
Individuals with active pancreatitis or history of pancreatitis should use these medications cautiously, as they have been associated with pancreatitis in rare cases. Patients with severe gastrointestinal disease, including gastroparesis, may experience symptom exacerbation due to delayed gastric emptying.
Those with diabetic retinopathy should be monitored closely, particularly during periods of rapid glycemic improvement, as temporary worsening of retinopathy has been observed. Patients with renal impairment can generally use semaglutide and tirzepatide without dose adjustment, though monitoring for dehydration from gastrointestinal side effects is important.
Patients should be monitored for depression and suicidal ideation, particularly when using these medications for weight management, as noted in FDA prescribing information.
Shared decision-making between patients and healthcare providers, incorporating individual risk factors, comorbidities, and treatment goals, ensures appropriate medication selection and monitoring strategies for optimal safety and efficacy outcomes.
Yes, patients with metabolic dysfunction-associated steatotic liver disease (MASLD) can generally use GLP-1 receptor agonists safely. Clinical studies show these medications may actually improve liver enzyme levels and reduce hepatic steatosis, though consultation with your healthcare provider is essential for individualized assessment.
Routine liver function monitoring is not specifically required by FDA labels for these medications unless other risk factors are present. Your healthcare provider will determine appropriate monitoring based on your individual medical history and any pre-existing liver conditions.
Contact your healthcare provider immediately if you develop jaundice (yellowing of skin or eyes), dark urine, persistent right upper quadrant abdominal pain, unexplained severe fatigue, or persistent vomiting. These symptoms may indicate liver dysfunction requiring prompt medical evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.