LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Glucagon-like peptide-1 (GLP-1) receptor agonists have revolutionized type 2 diabetes and obesity treatment, but many carry an FDA boxed warning regarding thyroid C-cell tumors, including medullary thyroid carcinoma (MTC). If you have a family history of thyroid cancer, understanding which types pose contraindications is essential. The warning specifically applies to personal or family history of MTC or multiple endocrine neoplasia syndrome type 2 (MEN 2)—not other thyroid cancer types like papillary or follicular carcinoma. While rodent studies showed thyroid tumors, no clear causal relationship exists in humans. This article clarifies who should avoid GLP-1 medications, necessary screening, and alternative treatment options for high-risk patients.
Quick Answer: GLP-1 receptor agonists are contraindicated only in patients with personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2), not other thyroid cancer types.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists have transformed the management of type 2 diabetes and obesity, offering significant benefits in glycemic control and weight reduction. However, many of these medications carry a boxed warning from the FDA regarding a potential risk of thyroid C-cell tumors, including medullary thyroid carcinoma (MTC). This warning stems from preclinical studies in rodents that demonstrated dose-dependent and treatment-duration-dependent thyroid C-cell tumors at clinically relevant exposures.
It is crucial to understand that no clear causal relationship has been established between GLP-1 receptor agonists and thyroid cancer in humans. The rodent findings may not directly translate to human risk due to significant species differences in thyroid C-cell biology and GLP-1 receptor expression. Rodents have substantially higher densities of GLP-1 receptors on thyroid C-cells compared to humans, and their thyroid physiology differs markedly from that of humans.
Despite the absence of confirmed human cases directly attributable to GLP-1 therapy, the FDA requires this warning as a precautionary measure for many GLP-1 medications. Post-marketing surveillance and observational studies have yielded mixed results, though the absolute risk appears very low given the rarity of MTC. Clinicians must carefully evaluate individual patient risk factors, particularly personal or family history of MTC or multiple endocrine neoplasia syndrome type 2 (MEN 2), before prescribing these agents. Understanding this nuanced risk-benefit profile enables informed shared decision-making between healthcare providers and patients considering GLP-1 therapy.
The FDA boxed warning specifically contraindicates certain GLP-1 receptor agonists in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with multiple endocrine neoplasia syndrome type 2 (MEN 2). This contraindication applies to semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), exenatide extended-release (Bydureon BCise), tirzepatide (Mounjaro, Zepbound), and the combination product Xultophy (insulin degludec/liraglutide). Notably, exenatide immediate-release (Byetta) and lixisenatide (Adlyxin, and in Soliqua) do not carry this boxed warning or contraindication.
MTC is a rare form of thyroid cancer originating from parafollicular C-cells, accounting for approximately 3-4% of all thyroid malignancies. Unlike the more common papillary or follicular thyroid cancers, MTC can occur in hereditary forms associated with MEN 2, an autosomal dominant syndrome caused by mutations in the RET proto-oncogene. Approximately 25% of MTC cases are hereditary, while 75% occur sporadically without identifiable family history.
The FDA warning does not extend to family history of other thyroid cancer types, such as papillary or follicular carcinoma, which have different cellular origins and pathophysiology. Patients with family history of these more common thyroid cancers are not automatically excluded from GLP-1 therapy based on this specific contraindication. However, clinicians should maintain heightened awareness and conduct thorough risk assessment.
It is important to distinguish between family history of MTC specifically and general thyroid cancer history. A detailed family history should include the specific type of thyroid cancer, age at diagnosis, and whether multiple family members have been affected, as these factors help determine hereditary risk and appropriate screening strategies.
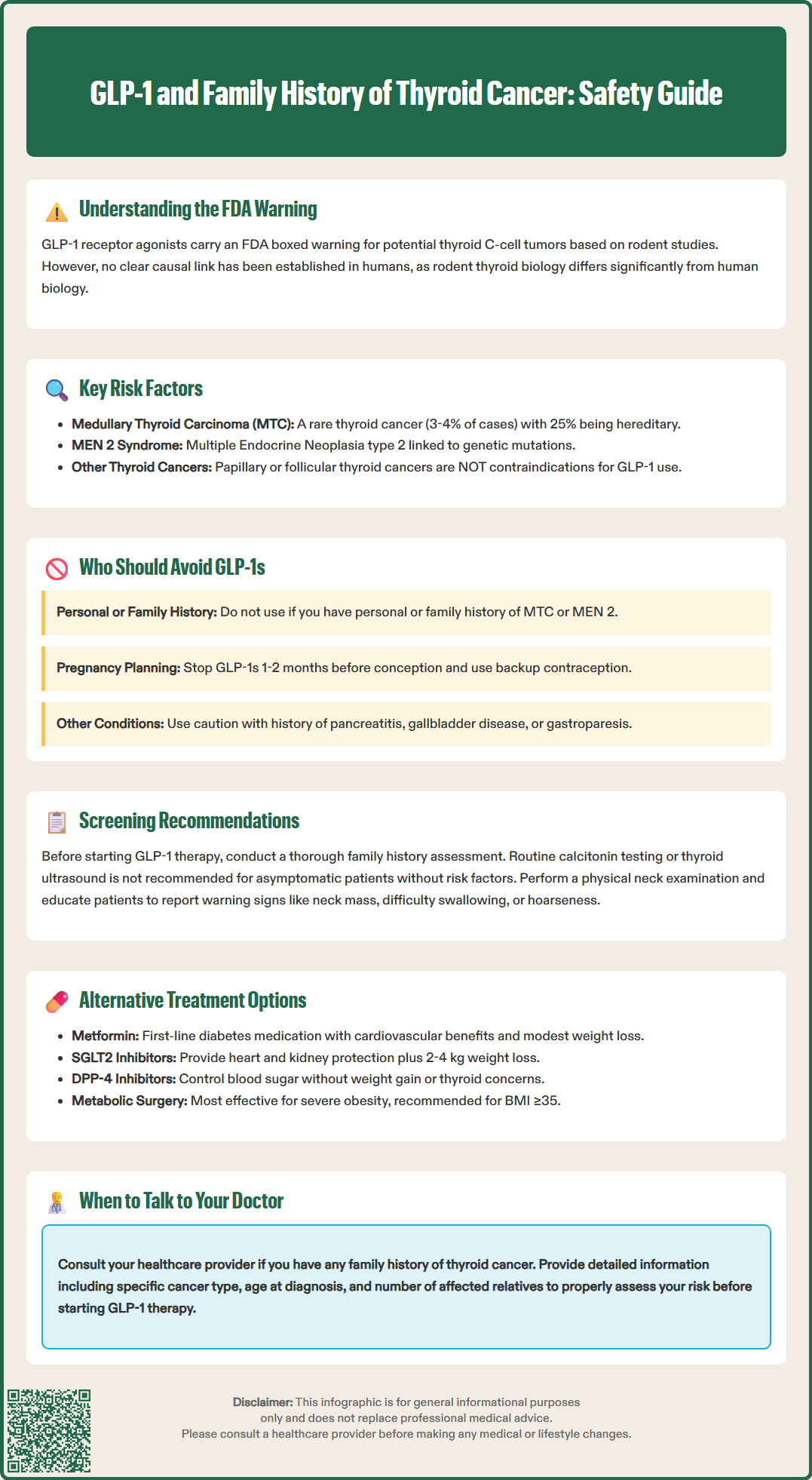
Absolute contraindications to GLP-1 receptor agonists with the boxed warning include patients with a personal history of MTC, family history of MTC, or known MEN 2 syndrome. These individuals should not receive these specific GLP-1 medications due to the theoretical risk suggested by animal studies, even though human causality remains unproven. The precautionary principle guides this recommendation given the serious nature of MTC and the availability of alternative therapeutic options.
Patients with MEN 2 syndrome warrant particular attention, as this hereditary condition predisposes to MTC, pheochromocytoma, and parathyroid adenomas. MEN 2 has two main subtypes: MEN 2A (the most common, featuring MTC, pheochromocytoma, and hyperparathyroidism) and MEN 2B (characterized by MTC, pheochromocytoma, marfanoid habitus, and mucosal neuromas). Genetic testing for RET mutations can identify affected individuals and at-risk family members.
Additional cautions apply to patients with thyroid nodules or elevated calcitonin levels, which warrant appropriate diagnostic evaluation rather than automatic exclusion from therapy. Patients with a history of pancreatitis should be considered for alternative agents when possible; if GLP-1 therapy is initiated, it should be discontinued promptly if pancreatitis is suspected.
GLP-1 receptor agonists have been associated with increased risk of gallbladder disease (cholelithiasis, cholecystitis) and may worsen symptoms in patients with gastroparesis due to delayed gastric emptying. Other populations requiring careful consideration include those with diabetic retinopathy (particularly with rapid glycemic improvement) and individuals with renal impairment.
Pregnant women should avoid GLP-1 receptor agonists. Women planning pregnancy should discontinue these medications according to product-specific guidance (e.g., semaglutide at least 2 months before planned conception; tirzepatide approximately 1 month before). Women using oral contraceptives should be advised that delayed gastric emptying, particularly with tirzepatide, may reduce contraceptive efficacy.
Before initiating GLP-1 receptor agonist therapy, clinicians should conduct a comprehensive personal and family history assessment focusing specifically on thyroid disorders and endocrine neoplasia syndromes. Key questions should address any personal history of thyroid nodules, thyroid cancer, or thyroid surgery, as well as detailed family history of MTC, MEN 2, or other endocrine tumors across multiple generations. Documentation should include the specific cancer type when known, as this distinction is clinically significant.
Routine measurement of serum calcitonin levels or thyroid ultrasound screening before starting GLP-1 therapy is not recommended in asymptomatic patients without specific risk factors. The American Diabetes Association does not advocate for routine calcitonin screening due to concerns about false-positive results, low positive predictive value, and potential for unnecessary interventions. Calcitonin levels can be elevated in various benign conditions, including C-cell hyperplasia, chronic kidney disease, hypergastrinemia, and thyroiditis.
If calcitonin testing is performed for clinical reasons and results are elevated, confirmation with repeat testing is advisable. Interpretation should consider sex-specific reference ranges and assay variability. Persistently elevated levels (generally >50-100 pg/mL, though reference ranges vary by laboratory) warrant further evaluation. This typically includes thyroid ultrasound examination to assess for nodules or structural abnormalities, and potentially fine-needle aspiration biopsy of suspicious lesions. Patients with significantly elevated calcitonin levels or progressive increases should be referred to endocrinology for specialized evaluation.
Physical examination should include careful neck palpation to detect thyroid enlargement or nodules. Patients should be counseled about symptoms that might suggest thyroid pathology, including neck mass, dysphagia, hoarseness, or persistent cough, and instructed to report these promptly. While ongoing monitoring of calcitonin during GLP-1 therapy is not standard practice, patients should receive education about thyroid cancer warning signs and the importance of reporting new symptoms.
For patients with contraindications to GLP-1 receptor agonists, numerous effective alternatives exist for managing type 2 diabetes and obesity. Metformin offers proven cardiovascular benefits, weight neutrality or modest weight loss, and an excellent safety profile. While traditionally considered first-line therapy, current American Diabetes Association guidance emphasizes a person-centered approach to initial medication selection based on comorbidities, treatment goals, and patient preferences.
SGLT2 inhibitors (sodium-glucose cotransporter-2 inhibitors) such as empagliflozin, dapagliflozin, and canagliflozin represent excellent alternatives, providing cardiovascular and renal protection alongside modest weight loss (typically 2-4 kg). These agents work by promoting urinary glucose excretion and carry no thyroid cancer warnings. They are particularly valuable for patients with established cardiovascular disease, heart failure, or chronic kidney disease. Initiation and continuation depend on eGFR thresholds, which vary by specific agent.
DPP-4 inhibitors (dipeptidyl peptidase-4 inhibitors) like sitagliptin, linagliptin, and saxagliptin offer another option for glycemic control without weight gain and with minimal hypoglycemia risk. While they do not provide the weight loss benefits of GLP-1 agonists, they are well-tolerated and have no thyroid-related contraindications.
For weight management specifically, lifestyle modification remains foundational, incorporating medical nutrition therapy, structured physical activity programs, and behavioral counseling. When pharmacotherapy is needed, alternatives include phentermine-topiramate (Qsymia), which requires monitoring for psychiatric effects and is contraindicated in pregnancy; naltrexone-bupropion (Contrave), which requires blood pressure monitoring and is contraindicated in seizure disorders and uncontrolled hypertension; and orlistat (Xenical, Alli), which has gastrointestinal side effects but a long safety record.
Metabolic surgery represents the most effective intervention for severe obesity and often produces diabetes remission. Current guidelines from the American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity (IFSO) support consideration in patients with BMI ≥35 kg/m² regardless of comorbidities, or BMI 30-34.9 kg/m² with metabolic disease. Multidisciplinary care optimizes outcomes regardless of the chosen therapeutic approach.
Yes, family history of papillary or follicular thyroid cancer does not contraindicate GLP-1 therapy. The FDA warning applies only to medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2), which are different from common thyroid cancers.
Routine calcitonin screening is not recommended for asymptomatic patients without risk factors. Testing may cause false-positive results and unnecessary interventions, so it should only be performed when clinically indicated based on personal or family history of MTC or MEN 2.
Safe alternatives include metformin, SGLT2 inhibitors (empagliflozin, dapagliflozin), DPP-4 inhibitors (sitagliptin, linagliptin), and exenatide immediate-release or lixisenatide, which do not carry thyroid cancer warnings. Your healthcare provider can recommend the best option based on your individual needs.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.