LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist marketed as Ozempic, Wegovy, and Rybelsus, is FDA-approved for type 2 diabetes and chronic weight management. Patients with autoimmune diseases often require treatment for these metabolic conditions, raising important questions about semaglutide safety in this population. While no absolute contraindications exist based solely on autoimmune disease presence, clinicians must consider individual patient factors, disease activity, and potential medication interactions. This article examines the current evidence on semaglutide use in autoimmune disease patients, addressing safety considerations, monitoring protocols, and clinical decision-making to guide appropriate prescribing in this complex patient population.
Quick Answer: Semaglutide has no absolute contraindications based solely on autoimmune disease presence and can be prescribed when indicated for diabetes or weight management with individualized risk-benefit assessment.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Available under brand names including Ozempic, Wegovy, and Rybelsus, this medication mimics the action of endogenous GLP-1, a naturally occurring incretin hormone that plays a central role in glucose homeostasis and appetite regulation.
The primary mechanism of action involves binding to GLP-1 receptors on pancreatic beta cells, which stimulates glucose-dependent insulin secretion. This means insulin release occurs only when blood glucose levels are elevated, reducing the risk of hypoglycemia compared to other antidiabetic agents, though this risk increases when used with insulin or sulfonylureas. Simultaneously, semaglutide suppresses glucagon secretion from pancreatic alpha cells, further contributing to improved glycemic control. Beyond pancreatic effects, the medication slows gastric emptying and acts on central nervous system pathways to reduce appetite and food intake, mechanisms that underlie its efficacy in weight management.
Semaglutide has a prolonged half-life of approximately one week, allowing for once-weekly subcutaneous administration in its injectable forms. The oral formulation utilizes absorption-enhancing technology to overcome the typical degradation of peptide medications in the gastrointestinal tract. Clinical trials have demonstrated reductions in hemoglobin A1c levels and weight loss that vary by dose and population—with higher doses (such as Wegovy 2.4 mg) achieving approximately 15% weight loss in obesity trials, with more modest effects at lower doses used for diabetes. Some formulations also have cardiovascular risk reduction indications in specific populations. Understanding these fundamental pharmacologic properties provides essential context when considering semaglutide use in patients with complex medical conditions, including those with autoimmune diseases.
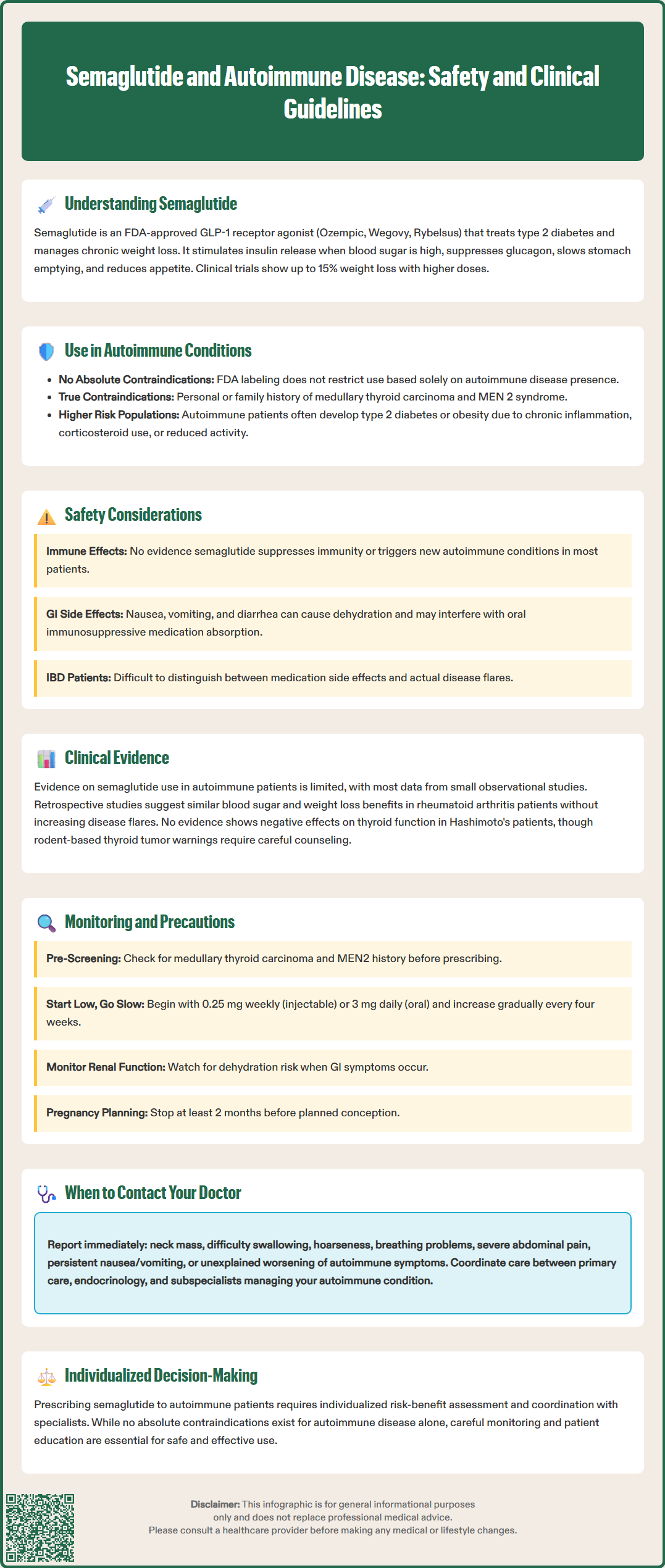
Patients with autoimmune diseases frequently require treatment for type 2 diabetes or obesity, conditions that occur at higher rates in certain autoimmune populations. The prevalence of metabolic dysfunction in autoimmune disease may relate to chronic inflammation, corticosteroid therapy, reduced physical activity due to disease burden, or shared genetic susceptibilities. Consequently, clinicians often encounter questions about the safety and appropriateness of semaglutide in this patient population.
Currently, there are no absolute contraindications to semaglutide use based solely on the presence of an autoimmune condition. The FDA-approved prescribing information does not list autoimmune diseases as contraindications, and clinical practice guidelines from the American Diabetes Association do not restrict GLP-1 receptor agonist use in patients with autoimmune disorders. However, the known contraindications that clinicians must observe include personal or family history of medullary thyroid carcinoma and multiple endocrine neoplasia syndrome type 2 (MEN 2), both related to thyroid C-cell concerns identified in rodent studies.
Important cautions include avoiding use in patients with severe gastroparesis or other severe gastrointestinal disease, monitoring for diabetic retinopathy complications (particularly in patients with pre-existing retinopathy), and avoiding use during pregnancy with a recommended washout period of at least 2 months before planned conception. Patients with a history of pancreatitis warrant careful consideration, as this condition represents a risk factor for recurrence.
While patients with various autoimmune conditions have been included in clinical trials of semaglutide, they typically were not primary study populations. Real-world evidence suggests that these patients can benefit from semaglutide therapy when indicated for diabetes or weight management. The decision to prescribe should involve individualized risk-benefit assessment, considering the patient's specific autoimmune diagnosis, disease activity, concurrent immunosuppressive medications, and overall health status. Coordination with the patient's rheumatologist, gastroenterologist, or other specialist managing the autoimmune condition is advisable to ensure comprehensive care and appropriate monitoring.
A critical question for clinicians and patients concerns whether semaglutide directly affects immune system function or could theoretically exacerbate autoimmune disease activity. Current evidence suggests that GLP-1 receptor agonists do not have significant immunosuppressive or immunostimulatory properties that would be expected to substantially alter autoimmune disease course. GLP-1 receptors are expressed on various immune cells, including T lymphocytes and macrophages, and preclinical research has identified potential anti-inflammatory effects of GLP-1 signaling, but the clinical significance of these observations remains uncertain.
Some laboratory and animal studies have suggested that GLP-1 receptor activation may reduce inflammatory cytokine production and modulate immune cell function in ways that could theoretically be beneficial in inflammatory conditions. However, these findings have not translated into established clinical applications for autoimmune disease treatment, and semaglutide is not prescribed for immunomodulatory purposes. Based on available evidence, there is no clear indication that semaglutide triggers new-onset autoimmune conditions or worsens existing autoimmune disease activity in most patients, though systematic studies are limited.
The most relevant safety considerations for patients with autoimmune diseases relate to semaglutide's known adverse effect profile rather than direct immune effects. Gastrointestinal symptoms—including nausea, vomiting, diarrhea, and constipation—occur commonly, particularly during dose escalation. These symptoms can lead to dehydration and potentially acute kidney injury in susceptible individuals. For patients with inflammatory bowel disease, distinguishing between medication side effects and disease flares may be challenging. Additionally, patients taking immunosuppressive medications may have altered responses to infections, and any medication causing significant gastrointestinal symptoms could affect absorption of oral immunosuppressants.
Rare but serious adverse effects include pancreatitis, gallbladder disease, hypersensitivity reactions (including anaphylaxis and angioedema), and, for Wegovy specifically, suicidal ideation. Some autoimmune conditions and their treatments may independently increase these risks. Clinicians should maintain awareness that the overall safety profile of semaglutide in autoimmune disease populations has not been extensively studied in dedicated trials.
The clinical evidence specifically examining semaglutide use in patients with autoimmune diseases remains limited, with most data derived from subgroup analyses of larger trials or observational studies rather than dedicated prospective investigations. Major cardiovascular outcomes trials such as SUSTAIN-6 and PIONEER-6 included patients with various comorbidities, but did not specifically report outcomes in autoimmune disease subgroups, representing a knowledge gap in this area.
Limited observational studies and case series have described GLP-1 receptor agonist use, including semaglutide, in patients with specific autoimmune diseases. In patients with type 2 diabetes and rheumatoid arthritis, retrospective analyses suggest that GLP-1 receptor agonists may provide glycemic and weight benefits comparable to those seen in the general diabetes population, without apparent increases in rheumatoid arthritis flares or complications, though these observations are based on small samples. Similarly, there are reports of patients with psoriasis and metabolic syndrome being treated with GLP-1 receptor agonists in clinical practice, with some suggesting potential improvements in inflammatory markers, though causality cannot be established from these observations.
For patients with autoimmune thyroid disease, particularly Hashimoto's thyroiditis, there is no evidence that semaglutide adversely affects thyroid function or autoantibody levels. However, the black box warning regarding thyroid C-cell tumors observed in rodent studies necessitates careful patient selection and counseling, even though the relevance to human thyroid disease remains unclear. Patients with inflammatory bowel disease represent a population requiring particular consideration, as gastrointestinal adverse effects of semaglutide could potentially be confused with disease activity, though there is limited evidence regarding whether the medication directly affects inflammatory bowel disease course.
The absence of large-scale, controlled studies specifically addressing semaglutide safety and efficacy in autoimmune disease populations represents a significant knowledge gap. Clinicians must therefore rely on general safety data, pharmacologic principles, and individualized clinical judgment when prescribing semaglutide to these patients. Ongoing pharmacovigilance and real-world evidence collection will be important for further characterizing the risk-benefit profile in this diverse patient population.
When prescribing semaglutide to patients with autoimmune diseases, clinicians should implement a structured approach to patient selection, education, and monitoring. Initial assessment should include a comprehensive review of the patient's autoimmune diagnosis, current disease activity, medication regimen (particularly immunosuppressants and corticosteroids), and history of complications such as pancreatitis or gallbladder disease. Screening for personal or family history of medullary thyroid carcinoma and MEN2 is essential, with patient counseling regarding symptoms such as neck mass, dysphagia, hoarseness, or dyspnea that warrant prompt evaluation. Routine calcitonin monitoring is not recommended unless clinically indicated.
Patient education should address both the expected benefits and potential adverse effects of semaglutide, with particular emphasis on gastrointestinal symptoms that may be difficult to distinguish from autoimmune disease manifestations. Patients should be instructed to report new or worsening abdominal pain, persistent nausea or vomiting, or changes in bowel habits, as these could represent medication side effects, autoimmune disease activity, or serious complications such as pancreatitis. Clear communication channels with both the prescribing clinician and the specialist managing the autoimmune condition should be established.
Monitoring protocols should include standard assessments for diabetes or weight management (hemoglobin A1c, weight, blood pressure) as well as considerations specific to the patient's autoimmune condition. Renal function should be monitored when significant gastrointestinal symptoms occur due to risk of dehydration and acute kidney injury. Patients with pre-existing diabetic retinopathy should have appropriate ophthalmologic follow-up. Women of childbearing potential should be counseled about pregnancy prevention and the need for a 2-month washout period before planned conception. For patients with inflammatory bowel disease, coordination with gastroenterology regarding symptom assessment is important. Those taking immunosuppressive medications should have appropriate laboratory monitoring per established protocols for those agents.
Dose escalation should follow standard protocols, typically starting with 0.25 mg weekly for injectable semaglutide and increasing gradually every four weeks as tolerated. For oral semaglutide (Rybelsus), the starting dose is 3 mg daily for one month, followed by 7 mg daily, with potential increase to 14 mg if needed. Slower titration may be considered for patients with significant gastrointestinal sensitivity or active inflammatory bowel disease. When used with insulin or sulfonylureas, consider reducing doses of these medications to mitigate hypoglycemia risk. Semaglutide is not recommended in patients with severe gastroparesis. Referral triggers include severe or persistent gastrointestinal symptoms, signs of pancreatitis, symptoms suggesting gallbladder disease, unexplained worsening of autoimmune disease activity, or any concerns about medication interactions with immunosuppressive therapy. Multidisciplinary communication between primary care, endocrinology, and relevant subspecialists optimizes outcomes and safety for this complex patient population.
Yes, there are no absolute contraindications to semaglutide based solely on autoimmune disease presence. The decision should involve individualized risk-benefit assessment considering the specific autoimmune diagnosis, disease activity, and concurrent medications, with coordination between the prescribing clinician and the specialist managing the autoimmune condition.
Current evidence suggests semaglutide does not have significant immunosuppressive or immunostimulatory properties that would substantially alter autoimmune disease course. While GLP-1 receptors are expressed on immune cells, there is no clear indication that semaglutide triggers new autoimmune conditions or worsens existing disease activity in most patients.
Monitoring should include standard assessments for diabetes or weight management plus renal function when gastrointestinal symptoms occur, coordination with specialists managing the autoimmune condition, and careful attention to distinguishing medication side effects from autoimmune disease manifestations. Patients should report new abdominal pain, persistent nausea, or changes in bowel habits promptly.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.