LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

GLP-1 receptor agonist fatigue mechanism is an important consideration for clinicians managing patients on medications like semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro, Zepbound). Fatigue affects approximately 5-11% of patients taking these agents, according to FDA prescribing information. While no single direct mechanism has been definitively established, fatigue likely results from multiple factors including substantial caloric restriction, gastrointestinal side effects, dehydration, and metabolic adaptation during weight loss. Understanding these contributing mechanisms enables healthcare providers to implement targeted management strategies, optimize treatment tolerability, and distinguish medication-related fatigue from potentially serious underlying conditions requiring further evaluation.
Quick Answer: GLP-1 receptor agonist-related fatigue likely results from multiple indirect mechanisms including substantial caloric restriction, gastrointestinal side effects causing dehydration and nutritional deficits, and metabolic adaptation during weight loss, rather than a single direct pharmacological effect.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications that mimic the action of the naturally occurring incretin hormone GLP-1. These agents are FDA-approved primarily for the management of type 2 diabetes mellitus and, for specific products (Wegovy, Saxenda, Zepbound), for chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity. Common medications in this class include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro, Zepbound), though tirzepatide is technically a dual GLP-1/GIP receptor agonist.
The primary mechanism of action involves binding to GLP-1 receptors located throughout the body, particularly in pancreatic beta cells, the gastrointestinal tract, and the central nervous system. In pancreatic tissue, GLP-1 receptor agonists enhance glucose-dependent insulin secretion and suppress inappropriate glucagon release, thereby improving glycemic control without significantly increasing hypoglycemia risk. In the gastrointestinal system, these medications slow gastric emptying, which prolongs satiety and reduces postprandial glucose excursions.
Additionally, GLP-1 receptor agonists act on appetite-regulating centers in the hypothalamus, reducing hunger signals and promoting weight loss. The American Diabetes Association (ADA) recommends GLP-1 receptor agonists with proven cardiovascular benefit as preferred agents for patients with type 2 diabetes who have established atherosclerotic cardiovascular disease or indicators of high cardiovascular risk. Clinical trials have shown reductions in major adverse cardiovascular events, including myocardial infarction and stroke, with several agents in this class.
Importantly, these medications carry boxed warnings for medullary thyroid carcinoma risk and are contraindicated in patients with personal or family history of MEN2 or medullary thyroid carcinoma. Understanding these multisystem effects is essential when evaluating potential adverse effects, including fatigue, as the widespread distribution of GLP-1 receptors means these medications influence numerous physiological processes beyond glucose metabolism.
Fatigue is listed as a common adverse effect in FDA prescribing information for several GLP-1 receptor agonists. According to the Wegovy label, fatigue occurs in approximately 11% of patients versus placebo, while Saxenda reports fatigue in 5-9% of patients. Clinical experience suggests that some individuals experience increased tiredness, particularly during treatment initiation or dose escalation. The reported incidence varies across specific agents and doses, with fatigue sometimes grouped with asthenia or malaise in adverse event reporting.
Several indirect mechanisms may contribute to fatigue in patients taking GLP-1 receptor agonists. A significant factor is often the substantial caloric restriction that accompanies treatment. These medications markedly reduce appetite and food intake, with patients commonly reporting early satiety and decreased interest in eating. When caloric intake drops significantly, the resulting energy deficit can manifest as fatigue, weakness, or reduced exercise tolerance. This effect may be particularly pronounced in patients experiencing rapid weight loss.
Gastrointestinal side effects represent another potential contributor to fatigue. Nausea, vomiting, and diarrhea are among the most common adverse effects of GLP-1 receptor agonists, with frequencies varying by product and dose. For example, nausea occurs in approximately 44% of patients taking Wegovy, 40% with Saxenda, and 27% with Ozempic (highest dose). Persistent gastrointestinal symptoms can lead to reduced nutritional intake, dehydration, and electrolyte disturbances, all of which may present as fatigue. Patients who experience severe or prolonged nausea may develop food aversions that further compromise nutritional status.
Additionally, the metabolic changes associated with significant weight loss and improved glycemic control may temporarily affect energy levels as the body adapts to a new physiological state. Some patients report feeling less energetic during the initial months of treatment, with gradual improvement as weight stabilizes and metabolic adaptation occurs.
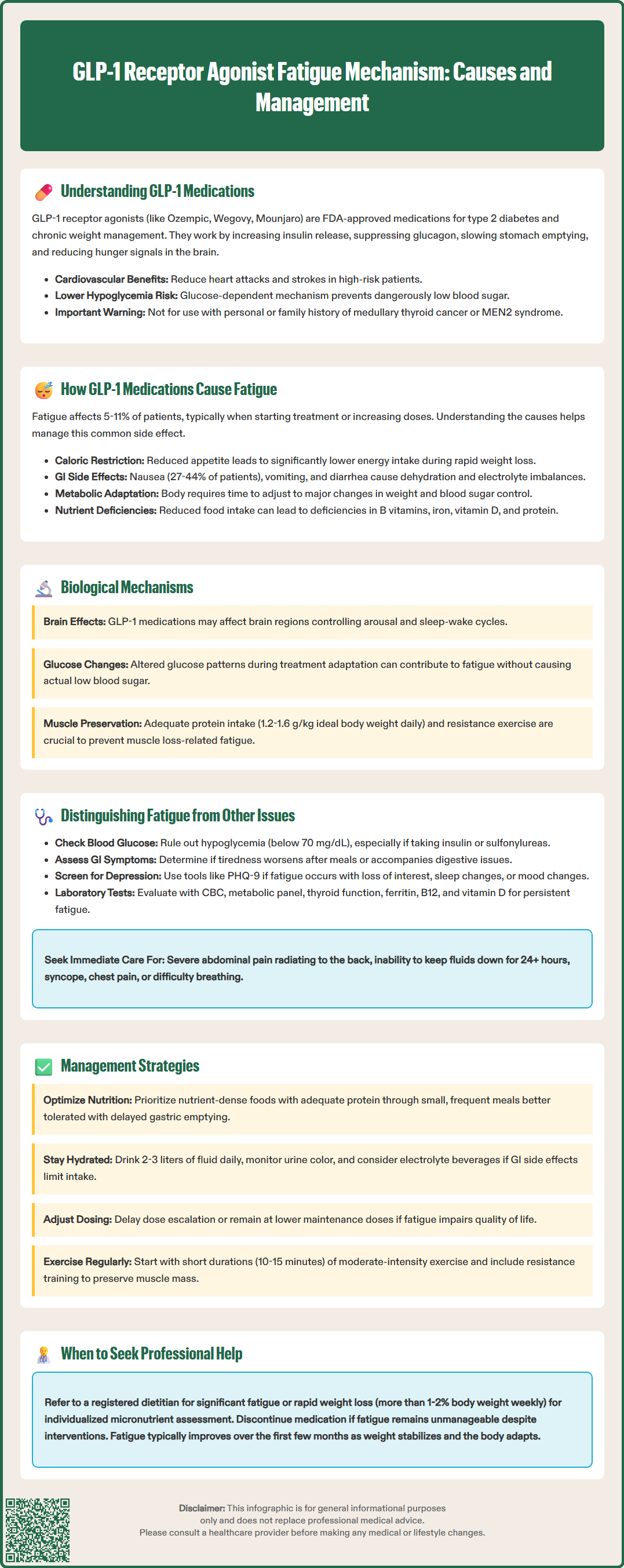
While there is no definitively established direct mechanism by which GLP-1 receptor agonists cause fatigue, several biological pathways warrant consideration. GLP-1 receptors are expressed in multiple brain regions, including areas involved in arousal, sleep-wake regulation, and energy homeostasis. Preclinical studies suggest that GLP-1 signaling in the central nervous system may influence neuronal activity patterns, though the clinical significance of these findings for human fatigue remains theoretical.
One proposed mechanism involves the effect of GLP-1 receptor agonists on glucose metabolism. Although these medications improve overall glycemic control, the combination of reduced food intake, delayed gastric emptying, and enhanced insulin secretion could theoretically affect glucose availability. It's important to note that clinically significant hypoglycemia is uncommon with GLP-1 receptor agonists unless they are used in combination with insulin or sulfonylureas. However, even without frank hypoglycemia, changes in glucose patterns during adaptation to therapy might contribute to fatigue in some individuals.
Nutritional deficiencies may develop as an indirect consequence of reduced and altered food intake. Patients consuming significantly fewer calories may not meet requirements for essential micronutrients, including B vitamins, iron, and vitamin D, all of which play crucial roles in energy metabolism. Inadequate protein intake is particularly concerning, as it can contribute to muscle loss during weight reduction. While GLP-1 receptor agonist therapy leads to greater relative fat loss than lean mass loss, preserving muscle tissue requires adequate protein intake and resistance exercise during weight reduction.
Dehydration represents another plausible mechanism, especially in patients experiencing gastrointestinal side effects. Reduced fluid intake due to nausea, combined with fluid losses from vomiting or diarrhea, can lead to volume depletion. Even mild dehydration can impair physical and cognitive performance, manifesting as fatigue, difficulty concentrating, and reduced exercise capacity. Electrolyte imbalances, particularly hyponatremia or hypokalemia, may accompany dehydration and further contribute to weakness and tiredness.
Accurate characterization of fatigue in patients taking GLP-1 receptor agonists requires careful clinical assessment to distinguish true fatigue from related symptoms and to identify potentially serious underlying causes. Fatigue should be differentiated from hypoglycemia, which can present with similar symptoms including weakness, shakiness, and difficulty concentrating. Patients taking GLP-1 receptor agonists in combination with insulin or sulfonylureas face increased hypoglycemia risk and should be counseled to check blood glucose when experiencing these symptoms. Documented glucose levels below 70 mg/dL indicate hypoglycemia requiring prompt evaluation and medication review, particularly if using insulin or sulfonylureas.
Gastrointestinal symptoms may be misattributed to fatigue or may coexist with and contribute to tiredness. Persistent nausea can create a general sense of malaise that patients describe as fatigue, while the physical effects of frequent vomiting or diarrhea can cause legitimate exhaustion. Clinicians should specifically inquire about the nature, timing, and associated features of fatigue. Fatigue that worsens after meals or is accompanied by abdominal discomfort may primarily reflect gastrointestinal side effects rather than a distinct energy problem.
Patients should be educated about red flag symptoms requiring immediate medical attention, including severe persistent abdominal pain (especially if radiating to the back, suggesting possible pancreatitis), right upper quadrant pain with fever or jaundice (potential gallbladder disease), inability to keep fluids down for more than 24 hours, syncope, chest pain, or difficulty breathing.
Depression and mood changes, though not commonly reported with GLP-1 receptor agonists, should be considered in the differential diagnosis of fatigue. The relationship between rapid weight loss, body image changes, and mood is complex. Some patients experience mood improvement with weight loss, while others may develop or experience worsening of depressive symptoms. Fatigue accompanied by anhedonia, sleep disturbances, or changes in appetite beyond those expected from the medication warrants evaluation for depression, potentially using validated screening tools like the PHQ-9.
Clinicians should also consider alternative medical explanations for new-onset fatigue, including thyroid dysfunction, anemia, sleep apnea (which may improve or persist despite weight loss), chronic kidney disease, or cardiovascular conditions. Basic laboratory evaluation is appropriate for patients with persistent or severe fatigue and should include complete blood count, comprehensive metabolic panel, thyroid-stimulating hormone, ferritin/iron studies, and vitamin B12 and vitamin D levels. The timing of fatigue onset relative to medication initiation provides important diagnostic information, though coincidental conditions may emerge during treatment.
Management of fatigue in patients taking GLP-1 receptor agonists begins with thorough assessment to identify contributing factors and exclude serious underlying conditions. For patients with fatigue primarily related to reduced caloric intake, nutritional counseling is essential. Patients should be encouraged to prioritize nutrient-dense foods and ensure adequate protein intake (typically 1.2-1.6 g/kg of ideal body weight daily during active weight loss, with higher amounts for those engaging in resistance training). Small, frequent meals may be better tolerated than larger meals given the delayed gastric emptying associated with these medications.
Hydration needs should be individualized based on activity level, climate, and comorbidities. Most adults require approximately 2-3 liters of fluid daily, but needs vary significantly. Patients should be counseled to monitor urine color (pale yellow indicating adequate hydration) and to increase fluid intake during exercise or hot weather. Those experiencing gastrointestinal side effects may benefit from oral rehydration solutions or electrolyte-containing beverages. If nausea limits fluid intake, patients should consult their prescriber about antiemetic medications. Ondansetron may be considered, though patients should be aware of potential side effects including constipation and, rarely, QT interval prolongation.
Dose adjustment strategies should be considered for patients with persistent fatigue that impairs quality of life. FDA labels for GLP-1 receptor agonists permit delaying dose escalation for tolerability issues. Some patients may need to remain at a lower maintenance dose rather than escalating to the maximum approved dose. This approach may result in less dramatic weight loss or glycemic improvement but can significantly improve tolerability and treatment adherence.
Physical activity, while challenging for fatigued patients, often improves energy levels over time. Patients should be encouraged to engage in regular moderate-intensity exercise, starting with short durations (10-15 minutes) if necessary and gradually increasing. Resistance training is particularly valuable for preserving lean muscle mass during weight loss. However, patients should be cautioned that exercise capacity may be temporarily reduced during the initial treatment period, and expectations should be adjusted accordingly.
Referral to a registered dietitian is appropriate for patients with significant fatigue, rapid weight loss (more than 1-2% body weight per week), or concerns about nutritional adequacy. Dietitians can assess micronutrient intake and recommend targeted supplementation when indicated. Vitamin and mineral supplementation should be individualized based on dietary intake assessment and laboratory findings rather than routinely prescribed. If fatigue persists despite these interventions, or if it is accompanied by other concerning symptoms, further medical evaluation is warranted to exclude alternative diagnoses. In some cases, discontinuation of the GLP-1 receptor agonist may be necessary if fatigue significantly impairs daily functioning and cannot be adequately managed through supportive measures.
GLP-1 receptor agonists cause fatigue primarily through indirect mechanisms including substantial caloric restriction from appetite suppression, gastrointestinal side effects leading to dehydration and nutritional deficits, and metabolic adaptation during weight loss. No single direct pharmacological mechanism has been definitively established.
According to FDA prescribing information, fatigue occurs in approximately 11% of patients taking Wegovy and 5-9% of patients taking Saxenda. The incidence varies by specific agent, dose, and individual patient factors.
Management strategies include ensuring adequate protein intake (1.2-1.6 g/kg ideal body weight daily), maintaining proper hydration, considering dose adjustment or delayed escalation, engaging in regular physical activity, and working with a registered dietitian. Laboratory evaluation should exclude alternative causes like thyroid dysfunction or anemia.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.