LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Weight regain after bariatric surgery affects many patients within 2–5 years post-operatively, prompting growing interest in pharmacologic interventions. Guidelines for pharmacologic therapy for weight regain after bariatric surgery with GLP-1 receptor agonists have evolved as these medications demonstrate promising efficacy in this population. GLP-1 receptor agonists such as semaglutide and liraglutide work by enhancing satiety, reducing appetite, and improving metabolic parameters—mechanisms that complement the physiological effects of surgery. Current recommendations from the American Society for Metabolic and Bariatric Surgery and the Endocrine Society support considering these agents as part of comprehensive management when lifestyle modifications prove insufficient and specific clinical criteria are met.
Quick Answer: Guidelines recommend considering GLP-1 receptor agonists for weight regain after bariatric surgery when BMI remains ≥27 kg/m² with comorbidities or ≥30 kg/m², lifestyle modifications are insufficient, and no anatomical complications require surgical revision.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight regain following bariatric surgery represents a significant clinical challenge, with studies suggesting it affects a substantial proportion of patients within 2–5 years post-operatively. While bariatric procedures such as Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy produce substantial initial weight loss, physiological adaptations and behavioral factors can contribute to gradual weight recurrence.
The mechanisms underlying weight regain are multifactorial and include metabolic adaptation with decreased energy expenditure, hormonal changes affecting appetite regulation, anatomical alterations such as gastric pouch or stoma dilation, and psychosocial factors including maladaptive eating behaviors. Research indicates that the body's homeostatic mechanisms actively defend against sustained weight loss through increased hunger signaling and reduced satiety hormone production.
It is important to note that no universal definition of clinically significant weight regain exists. Research and clinical practice commonly use various thresholds, including regaining more than 25% of maximum weight lost or achieving a body mass index (BMI) above 35 kg/m² with obesity-related comorbidities. Early identification is essential, as progressive weight regain can lead to recurrence of type 2 diabetes, hypertension, obstructive sleep apnea, and other obesity-related conditions that had previously improved or resolved.
The American Society for Metabolic and Bariatric Surgery (ASMBS) emphasizes that weight regain should not be viewed as surgical failure but rather as a chronic disease requiring ongoing management. A comprehensive evaluation is warranted to identify contributing factors, including assessment of surgical anatomy, eating patterns, physical activity levels, psychological factors, and metabolic parameters. Patients with concerning symptoms such as persistent vomiting, severe abdominal pain, or gastrointestinal bleeding should be promptly referred to their bariatric surgery team for evaluation. This comprehensive assessment forms the foundation for developing an individualized treatment plan that may include behavioral interventions, nutritional counseling, exercise prescription, psychological support, and increasingly, pharmacologic therapy.
Current clinical guidelines from major professional organizations provide evolving recommendations for pharmacologic management of weight regain after bariatric surgery. The ASMBS 2022 guidelines acknowledge that anti-obesity medications (AOMs) represent a valuable tool in the comprehensive management of post-bariatric weight regain, though evidence remains limited compared to primary obesity treatment.
The Endocrine Society's Clinical Practice Guideline on pharmacological management of obesity recommends considering AOMs for patients who experience weight regain after bariatric surgery, particularly when lifestyle modifications prove insufficient. Expert consensus suggests considering pharmacotherapy when there is:
Significant weight regain from nadir weight
BMI ≥27 kg/m² with obesity-related comorbidities or BMI ≥30 kg/m²
Absence of anatomical complications requiring surgical revision
Adequate adherence to nutritional and behavioral recommendations
Patient willingness to engage in long-term pharmacotherapy
The American Association of Clinical Endocrinologists (AACE) and American College of Endocrinology (ACE) guidelines emphasize that pharmacologic therapy should complement, not replace, lifestyle interventions and ongoing bariatric surgical follow-up. Medication selection should consider the patient's comorbidity profile, previous medication responses, potential drug interactions, and individual preferences.
FDA-approved medications for chronic weight management include GLP-1 receptor agonists (semaglutide injection, liraglutide), combination agents (phentermine/topiramate ER, naltrexone/bupropion ER), and lipase inhibitors (orlistat). While all are approved for obesity treatment, evidence specifically in post-bariatric populations varies considerably.
Importantly, current guidelines stress that AOMs should be prescribed as part of a comprehensive weight management program that includes dietary counseling, physical activity, behavioral therapy, and regular monitoring. The decision to initiate pharmacotherapy requires shared decision-making, discussing realistic expectations, potential adverse effects, cost considerations, and the likely need for indefinite treatment duration. Response assessment and discontinuation thresholds should follow FDA-labeled guidance for each specific medication.
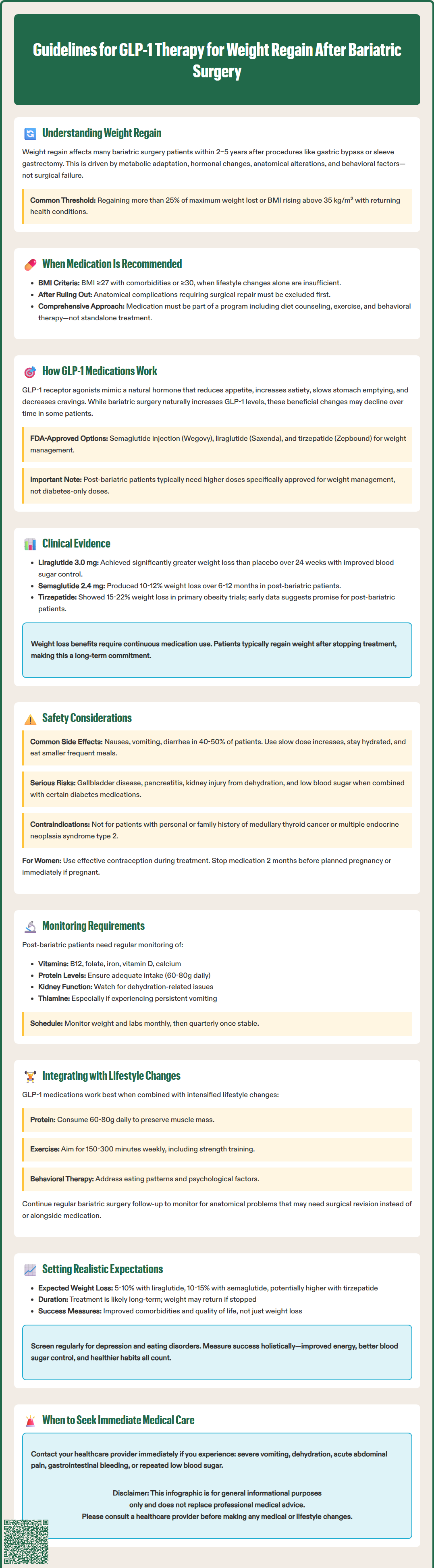
Glucagon-like peptide-1 (GLP-1) receptor agonists have emerged as particularly promising pharmacologic agents for managing weight regain after bariatric surgery, leveraging mechanisms that complement the physiological effects of surgical intervention. These medications work by mimicking endogenous GLP-1, an incretin hormone that plays crucial roles in glucose homeostasis and appetite regulation.
The mechanism of action of GLP-1 receptor agonists includes multiple pathways relevant to post-bariatric weight management. These agents bind to GLP-1 receptors in the pancreas, enhancing glucose-dependent insulin secretion and suppressing glucagon release. Centrally, they act on hypothalamic and brainstem nuclei to reduce appetite and increase satiety. Additionally, GLP-1 receptor agonists slow gastric emptying, which may be beneficial in some post-surgical patients. These medications also appear to reduce food reward signaling and hedonic eating behaviors.
Bariatric surgery itself increases endogenous GLP-1 levels, particularly after RYGB, contributing to improved glycemic control and weight loss. Some research suggests these beneficial hormonal changes may not be sustained in all patients over time, potentially contributing to weight regain in some cases.
Several GLP-1 receptor agonists are available, with varying pharmacokinetic profiles and approved indications. Semaglutide injection (Wegovy®) and liraglutide (Saxenda®) carry FDA approval specifically for chronic weight management in addition to their diabetes indications. Tirzepatide (Zepbound®), a dual GLP-1/GIP receptor agonist, represents a newer agent with robust weight loss efficacy. Oral semaglutide (Rybelsus®) is FDA-approved for type 2 diabetes management only, not for weight management. The choice among agents depends on factors including dosing frequency (daily versus weekly), route of administration, insurance coverage, patient preference, and comorbidity profile. Clinical experience suggests that higher-dose formulations approved for weight management (rather than diabetes-only doses) are generally necessary to achieve meaningful weight loss in the post-bariatric population.
The evidence base for GLP-1 receptor agonists in post-bariatric weight regain continues to expand, though large randomized controlled trials remain limited compared to primary obesity treatment. Available data demonstrate meaningful efficacy with acceptable safety profiles in this specific population.
Liraglutide 3.0 mg (Saxenda®) was among the first GLP-1 receptor agonists studied systematically in post-bariatric patients. A randomized controlled trial by Wharton et al. (Obesity, 2020) evaluated liraglutide versus placebo in patients with weight regain after RYGB or sleeve gastrectomy. Results showed that liraglutide-treated patients achieved significantly greater weight loss compared to placebo over 24 weeks. Improvements in glycemic parameters and quality of life measures were also observed. The medication demonstrated efficacy regardless of surgical procedure type.
Semaglutide 2.4 mg (Wegovy®) has shown robust weight loss in primary obesity trials, with mean weight reductions of 14.9% in the STEP 1 trial published in the New England Journal of Medicine (2021). While dedicated large-scale trials in post-bariatric populations are ongoing, retrospective studies suggest efficacy in patients with weight regain. A retrospective cohort study by Smith et al. (Surgery for Obesity and Related Diseases, 2023) reported mean weight loss of approximately 10-12% with semaglutide in post-bariatric patients over 6–12 months, though results varied considerably between individuals.
Tirzepatide (Zepbound® for weight management; Mounjaro® for diabetes) demonstrated significant weight loss in the SURMOUNT-1 trial published in the New England Journal of Medicine (2022), with mean reductions of 15–22% depending on dose. Early real-world data suggest promising results in post-bariatric patients, though formal trials are limited.
Important considerations include that most studies enrolled patients 1–5 years post-surgery with moderate weight regain. Evidence for use in early post-operative periods (<12 months) or in patients with severe weight regain approaching pre-surgical weights remains limited. Additionally, durability of effect requires ongoing treatment, with weight regain typically occurring upon medication discontinuation.
Safety considerations for GLP-1 receptor agonist use in post-bariatric surgery patients require careful attention, as this population may have unique vulnerabilities and altered pharmacokinetics compared to patients without surgical history. While these medications are generally well-tolerated, specific adverse effects and monitoring parameters warrant clinical vigilance.
Common adverse effects include gastrointestinal symptoms such as nausea (reported in 40–50% of patients), vomiting, diarrhea, constipation, and abdominal discomfort. These effects are typically dose-dependent, most prominent during dose escalation, and often improve with continued use. In post-bariatric patients who may already experience gastrointestinal sensitivity, gradual dose titration is particularly important. Strategies to minimize symptoms include slower titration schedules, maintaining adequate hydration, and consuming smaller, more frequent meals. For oral semaglutide (Rybelsus®), it must be taken on an empty stomach with no more than 4 ounces of plain water, at least 30 minutes before food, beverages, or other medications.
Serious adverse effects requiring monitoring include:
Hypoglycemia: While GLP-1 receptor agonists have low intrinsic hypoglycemia risk due to glucose-dependent mechanisms, risk increases with concomitant insulin or sulfonylurea use. Dose adjustments of these medications may be necessary, particularly in patients with diabetes.
Gallbladder disease: Rapid weight loss increases cholelithiasis risk. Patients should be counseled on symptoms of cholecystitis and cholelithiasis.
Pancreatitis: Although causality remains debated, acute pancreatitis has been reported. These medications should be used with caution in patients with a history of pancreatitis. Patients with severe, persistent abdominal pain require evaluation.
Acute kidney injury: Dehydration from gastrointestinal side effects may lead to acute kidney injury. Adequate hydration and renal function monitoring are important, especially during dose escalation.
Diabetic retinopathy complications: For patients with diabetes and retinopathy, rapid improvement in glucose control with semaglutide may be associated with temporary worsening of retinopathy.
Intestinal obstruction: Rare cases of ileus/intestinal obstruction have been reported in postmarketing surveillance.
Nutritional monitoring is critical in post-bariatric patients receiving GLP-1 receptor agonists, as both surgery and medication-induced reduced intake can compound deficiency risks. Recommended monitoring includes:
Complete blood count, comprehensive metabolic panel
Vitamin B12, folate, iron studies, vitamin D, calcium, parathyroid hormone
Thiamine in patients with persistent vomiting
Protein intake assessment and albumin/prealbumin levels
Contraindications include personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2, as GLP-1 receptor agonists carry a boxed warning based on rodent studies showing thyroid C-cell tumors. Pregnancy is an absolute contraindication; women of childbearing potential should use effective contraception. For tirzepatide, patients should be advised that oral contraceptive effectiveness may be reduced during initiation and dose escalation; non-oral or backup contraception methods should be considered. For semaglutide, discontinuation at least 2 months before planned conception is recommended. For all GLP-1 receptor agonists, discontinuation is advised upon recognition of pregnancy.
Successful management of post-bariatric weight regain with GLP-1 receptor agonists requires integration within a comprehensive, multidisciplinary care framework rather than medication as monotherapy. This approach optimizes outcomes and addresses the multifactorial nature of weight regain.
Lifestyle intervention remains foundational and should be intensified concurrently with medication initiation. Dietary counseling should focus on high-protein intake (60–80 g daily), adequate hydration, vitamin and mineral supplementation adherence, and avoidance of high-calorie liquids and grazing behaviors. Registered dietitians with bariatric expertise can provide meal planning strategies that accommodate both surgical anatomy and medication-related appetite changes. Physical activity recommendations should target 150–300 minutes of moderate-intensity exercise weekly, with resistance training to preserve lean body mass during weight loss.
Behavioral and psychological support addresses emotional eating, stress management, body image concerns, and medication adherence. Cognitive-behavioral therapy has demonstrated efficacy in post-bariatric populations. Screening for depression, anxiety, and eating disorders should occur regularly, as these conditions may contribute to weight regain and affect treatment response.
Surgical follow-up must continue despite medication initiation. Regular assessment by the bariatric surgery team ensures anatomical integrity, identifies potential surgical complications, and monitors for nutritional deficiencies. Upper endoscopy or contrast studies may be indicated if anatomical issues such as gastrojejunal anastomosis dilation are suspected, as these may require surgical revision rather than or in addition to pharmacotherapy.
Monitoring and adjustment protocols should include:
Weight and vital signs at each visit (initially monthly, then quarterly)
Assessment of medication tolerance and adherence
Evaluation of eating behaviors and physical activity
Laboratory monitoring as outlined previously
Reassessment of weight-related comorbidities
Realistic expectations should be established through shared decision-making. Patients should understand that expected weight loss varies by medication (approximately 5-10% with liraglutide, 10-15% with semaglutide, and potentially higher with tirzepatide), though responses in post-bariatric patients may differ from those in primary obesity treatment. Medication is likely long-term or indefinite, and weight regain may occur upon discontinuation. Treatment success should be defined not only by weight loss but also by improvements in comorbidities, quality of life, and prevention of further weight gain. If response is inadequate after the FDA-recommended evaluation period at therapeutic doses, consider switching to an alternative agent or referring for surgical revision evaluation in appropriate candidates. Combination pharmacotherapy, while sometimes used in clinical practice, is generally off-label with limited evidence in post-bariatric populations and requires careful monitoring.
Patients should be instructed to seek immediate medical attention for red-flag symptoms including intractable vomiting, severe dehydration, acute abdominal pain, gastrointestinal bleeding, or recurrent hypoglycemia, which may indicate surgical complications requiring urgent evaluation by the bariatric surgery team.
GLP-1 receptor agonists should be considered when patients experience significant weight regain with BMI ≥27 kg/m² with obesity-related comorbidities or BMI ≥30 kg/m², lifestyle modifications have been insufficient, no anatomical complications require surgical revision, and patients are willing to engage in long-term pharmacotherapy.
Semaglutide injection (Wegovy) and liraglutide (Saxenda) are FDA-approved specifically for chronic weight management and can be used in post-bariatric patients. Tirzepatide (Zepbound), a dual GLP-1/GIP receptor agonist, is also approved for weight management, though evidence in post-bariatric populations is still emerging.
Monitoring includes regular assessment of weight, vital signs, medication tolerance, complete blood count, comprehensive metabolic panel, renal function, and nutritional parameters including vitamin B12, folate, iron, vitamin D, calcium, and protein status. Patients should also be monitored for gastrointestinal symptoms, hypoglycemia risk, and signs of gallbladder disease or pancreatitis.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.