LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for chronic weight management, commonly affects bowel movements as part of its mechanism of action. This dual GIP and GLP-1 receptor agonist slows gastric emptying and alters gut motility, leading to gastrointestinal effects in many patients. Understanding how tirzepatide influences digestive function—and recognizing when bowel changes require medical attention—helps patients manage these effects while maintaining treatment adherence. This guide provides evidence-based strategies for navigating bowel-related symptoms during tirzepatide therapy.
Quick Answer: Tirzepatide commonly causes bowel changes including diarrhea (12-18%) and constipation (6-16%) by slowing gastric emptying and altering gut motility throughout the digestive tract.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). Understanding its mechanism of action helps explain why gastrointestinal effects, including changes in bowel movements, are among the most commonly reported adverse events.
The medication works by mimicking naturally occurring incretin hormones that regulate blood glucose and appetite. GLP-1 receptor activation slows gastric emptying—the rate at which food leaves the stomach and enters the small intestine. This delayed gastric emptying is most pronounced after the first dose and typically attenuates over time with continued treatment. This effect contributes to increased satiety and improved glycemic control but also affects the overall digestive process, potentially influencing gut motility throughout the gastrointestinal tract.
Clinical trials have consistently demonstrated that gastrointestinal adverse effects occur in a substantial proportion of patients initiating tirzepatide therapy. Both the SURPASS program (type 2 diabetes) and SURMOUNT program (obesity) reported nausea, diarrhea, and constipation among the most frequent treatment-emergent adverse events, particularly during dose escalation phases. These effects result from the medication's pharmacological action on GI receptors rather than representing an allergic or idiosyncratic reaction.
The intensity and duration of bowel changes typically correlate with dosing patterns. Most patients experience the greatest GI impact during the first few weeks after starting treatment or following dose increases. The FDA-approved prescribing information recommends gradual dose titration specifically to minimize gastrointestinal tolerability issues, allowing the digestive system time to adapt to the medication's effects on gut function.
Importantly, tirzepatide is not recommended for patients with severe gastroparesis. Additionally, the delayed gastric emptying can reduce the absorption of oral medications, including oral contraceptives. Patients using oral contraceptives should use an additional non-oral contraceptive method for 4 weeks after tirzepatide initiation and for 4 weeks after each dose escalation.
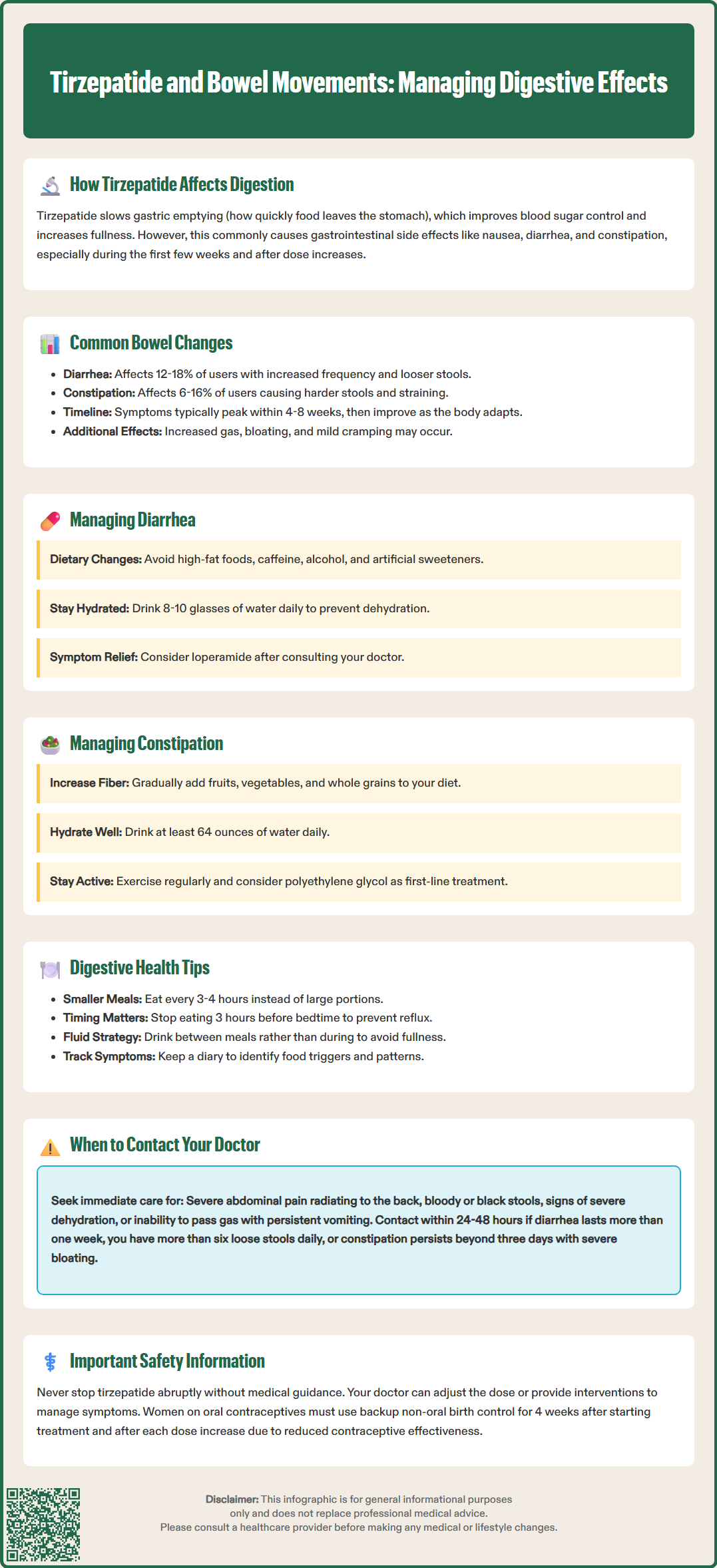
Patients taking tirzepatide may experience a spectrum of bowel-related changes, with diarrhea and constipation representing the most frequently reported alterations. According to FDA labeling data, the frequency of these effects varies by indication and dose. For Mounjaro (type 2 diabetes), diarrhea occurred in approximately 12-13% of patients, while constipation affected roughly 6% of participants. For Zepbound (obesity), rates were higher—approximately 18% for diarrhea and 16% for constipation. These percentages typically increased at higher maintenance doses.
Diarrhea characteristics typically include increased stool frequency, looser consistency, and occasionally urgency. Most cases are mild to moderate in severity and self-limiting. The diarrhea associated with tirzepatide differs from infectious gastroenteritis—it generally lacks fever, severe cramping, or bloody stools. The mechanism likely involves altered intestinal transit time in susceptible individuals.
Constipation patterns manifest as decreased bowel movement frequency, harder stool consistency, straining, or a sensation of incomplete evacuation. This paradoxical effect—opposite to diarrhea—may result from excessive slowing of gut motility in certain patients or from dietary changes that accompany reduced appetite. Some patients report alternating between constipation and looser stools as their bodies adjust to treatment.
Other bowel-related symptoms may include increased flatulence, abdominal bloating, and mild cramping. These effects often accompany the primary bowel changes and reflect the medication's impact on digestive function. The temporal pattern is important: symptoms typically peak within the first 4-8 weeks of therapy or after dose escalation, then often improve as physiological adaptation occurs. While many patients experience significant improvement over time, some may have persistent mild symptoms that remain tolerable and do not require treatment discontinuation.
Less common but important gastrointestinal-related adverse events include pancreatitis and gallbladder disease, which can present with specific abdominal pain patterns and require prompt medical evaluation.
Effective management of bowel changes during tirzepatide therapy involves both preventive strategies and symptomatic interventions. A proactive approach can significantly improve treatment tolerability and reduce the likelihood of discontinuation due to gastrointestinal adverse effects.
For diarrhea management, dietary modifications form the foundation of conservative treatment. Patients should consider temporarily reducing intake of high-fat foods, caffeine, alcohol, and artificial sweeteners, all of which can exacerbate loose stools. The BRAT diet (bananas, rice, applesauce, toast) may provide short-term symptomatic relief during acute episodes but is not nutritionally complete for extended use. Adequate hydration is essential—patients should aim for 8-10 glasses of water daily to replace fluid losses and prevent dehydration. Oral rehydration solutions containing electrolytes may be beneficial for more significant diarrhea.
Over-the-counter antidiarrheal medications such as loperamide (Imodium) can be used for symptomatic relief, but patients should consult their healthcare provider before regular use. These agents should not be used if fever, bloody stools, or severe abdominal pain are present, as these symptoms may indicate a more serious condition requiring medical evaluation.
For constipation management, increasing dietary fiber intake through fruits, vegetables, whole grains, and fiber supplements (such as psyllium) can promote regular bowel movements. However, fiber should be increased gradually to avoid worsening bloating. Physical activity stimulates intestinal motility and should be encouraged. Adequate fluid intake—at least 64 ounces daily—is crucial for preventing and treating constipation.
Over-the-counter options include osmotic laxatives (polyethylene glycol) as first-line therapy. Magnesium-containing products (magnesium hydroxide/milk of magnesia) should be avoided in patients with kidney disease. Stool softeners (docusate sodium) have limited evidence for effectiveness in chronic constipation. Stimulant laxatives should be reserved for short-term use under medical guidance.
General strategies applicable to both conditions include eating smaller, more frequent meals rather than large portions, which can overwhelm the slowed digestive system. Keeping a symptom diary helps identify dietary triggers and patterns. If gastrointestinal symptoms are severe or persistent, healthcare providers may consider temporarily pausing tirzepatide, reducing the dose, or extending the titration interval. Patients should never adjust their tirzepatide dose independently.
Patients should be alert for signs of dehydration that could lead to acute kidney injury, especially with severe diarrhea. Decreased urination, dark urine, dizziness, or extreme thirst warrant prompt medical attention.
While most bowel changes associated with tirzepatide are self-limited and manageable, certain symptoms warrant prompt medical evaluation. Patients should understand the distinction between expected medication effects and potentially serious complications requiring clinical assessment.
Immediate medical attention is necessary if patients experience severe, persistent abdominal pain, particularly epigastric pain that radiates to the back (possible pancreatitis) or right upper quadrant pain with fever or yellowing of the skin/eyes (possible gallbladder disease). If pancreatitis is suspected, patients should stop taking tirzepatide and seek urgent medical care. Bloody or black tarry stools require urgent evaluation to exclude gastrointestinal bleeding. Signs of severe dehydration—including dizziness upon standing, decreased urination, extreme thirst, or confusion—necessitate same-day assessment. Persistent vomiting that prevents adequate fluid or medication intake also requires prompt intervention.
Symptoms suggesting possible bowel obstruction or ileus—severe abdominal distension, inability to pass gas, persistent vomiting, and complete absence of bowel movements—warrant emergency evaluation.
Contact your healthcare provider within 24-48 hours if diarrhea persists beyond one week despite conservative management, or if you experience more than six loose stools daily. Constipation lasting more than three days without bowel movement, especially if accompanied by severe bloating or abdominal distension, warrants medical consultation. New or worsening abdominal pain that interferes with daily activities should be evaluated. Unintentional weight loss exceeding expected therapeutic goals may indicate malabsorption or inadequate nutrition.
Routine follow-up discussion should address bowel changes that, while not severe, significantly impact quality of life or treatment adherence. Patients experiencing persistent symptoms beyond 8-12 weeks may benefit from dose adjustment or additional interventions. Those with pre-existing gastrointestinal conditions—inflammatory bowel disease, irritable bowel syndrome, or gastroparesis—should maintain closer monitoring and more frequent communication with their healthcare team.
The American Diabetes Association Standards of Care recommends regular assessment of medication tolerability, including gastrointestinal symptoms, at each clinical encounter. Patients should never discontinue tirzepatide abruptly without medical guidance, as alternative management strategies may effectively address bowel symptoms while preserving the medication's metabolic benefits.
Optimizing digestive health during tirzepatide therapy requires a comprehensive approach addressing diet, lifestyle, and medication management. These strategies can help minimize bowel-related adverse effects and support overall treatment success.
Dietary considerations play a central role in gastrointestinal tolerance. Patients should limit high-fat meals, which can exacerbate nausea and diarrhea by further delaying gastric emptying. Incorporate easily digestible proteins such as chicken, fish, eggs, and plant-based options. Avoid trigger foods commonly associated with GI distress, including spicy dishes, fried foods, and highly processed items. Probiotic-rich foods—yogurt, kefir, sauerkraut, and kimchi—may support healthy gut microbiota, though evidence specific to tirzepatide users remains limited.
Meal timing and portion control significantly impact symptom severity. Eat smaller meals every 3-4 hours rather than three large meals daily. This approach prevents overwhelming the slowed digestive system. Avoid eating within 3 hours of bedtime to reduce nocturnal reflux and morning nausea. Chew food thoroughly and eat slowly, allowing at least 20-30 minutes per meal to facilitate proper digestion.
Hydration strategies extend beyond simple water intake. Distribute fluid consumption throughout the day rather than drinking large volumes at once. Limit beverages with meals to prevent excessive fullness; instead, hydrate between meals. Herbal teas, particularly ginger, may provide additional digestive support for some patients, though evidence is limited. Peppermint tea should be avoided in those with reflux as it can worsen symptoms. Avoid carbonated beverages if experiencing bloating.
Lifestyle modifications include regular physical activity, which promotes healthy gut motility. Aim for at least 150 minutes of moderate-intensity exercise weekly, as recommended by the U.S. Department of Health and Human Services. Stress management through mindfulness, adequate sleep, or relaxation techniques may reduce stress-related bowel symptoms. Establish a consistent daily routine for meals and bathroom visits to support regular bowel patterns.
Medication administration should follow FDA-approved guidelines: inject tirzepatide once weekly on the same day each week, with or without meals. If a dose is missed and the next scheduled dose is more than 4 days away, administer the missed dose; if less than 4 days away, skip the missed dose and administer the next dose on the regularly scheduled day. Proper injection technique and site rotation prevent local reactions that might indirectly affect comfort.
Women using oral contraceptives should use an additional non-oral contraceptive method for 4 weeks after tirzepatide initiation and for 4 weeks after each dose escalation, as tirzepatide may reduce the effectiveness of oral contraceptives. Maintain open communication with your healthcare provider about all medications and supplements, as some may interact with tirzepatide or independently affect bowel function. Never share medications or adjust doses without professional guidance.
Most bowel changes peak within the first 4-8 weeks of tirzepatide therapy or after dose increases, then typically improve as the body adapts. While many patients experience significant improvement over time, some may have persistent mild symptoms that remain tolerable.
Over-the-counter options like loperamide for diarrhea or polyethylene glycol for constipation can be used, but patients should consult their healthcare provider before regular use. Avoid antidiarrheals if fever, bloody stools, or severe abdominal pain are present.
Seek immediate medical attention for severe abdominal pain, bloody or black stools, signs of severe dehydration, or persistent vomiting. Contact your provider within 24-48 hours if diarrhea persists beyond one week or constipation lasts more than three days despite conservative management.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.