LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Hair loss due to GLP-1 medications has emerged as a concern for patients using these increasingly popular drugs for diabetes and weight management. GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) can be associated with temporary hair shedding, documented in FDA prescribing information. This hair loss typically results from rapid weight reduction rather than direct drug effects on hair follicles. Understanding the mechanisms, prevalence, and management strategies helps patients and clinicians address this generally reversible side effect while maintaining the substantial metabolic benefits these medications provide.
Quick Answer: Hair loss associated with GLP-1 medications is typically temporary telogen effluvium caused by rapid weight loss rather than direct drug effects on hair follicles.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications originally developed for type 2 diabetes management and now widely prescribed for chronic weight management. These agents include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist, not a pure GLP-1 medication. These medications work by mimicking naturally occurring intestinal hormones that regulate blood glucose and appetite.
The mechanism of action involves multiple pathways. These agents enhance glucose-dependent insulin secretion from pancreatic beta cells, suppress inappropriate glucagon release, slow gastric emptying, and act on central nervous system appetite centers to promote satiety. These combined effects lead to improved glycemic control in patients with diabetes and significant weight reduction in both diabetic and non-diabetic individuals. Clinical trials have demonstrated weight loss ranging from approximately 10% with GLP-1 agents at weight management doses (e.g., semaglutide 2.4 mg in the STEP trials) to over 20% with tirzepatide at higher doses (SURMOUNT trials).
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which typically diminish over time. More serious but less common risks include pancreatitis and gallbladder disease. These medications carry a boxed warning about thyroid C-cell tumors observed in rodent studies and are contraindicated in patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Weight management formulations are contraindicated during pregnancy. Hypoglycemia risk increases when used with insulin or sulfonylureas. The FDA labels for these medications provide comprehensive safety information, with alopecia (hair loss) specifically listed in the Wegovy and Zepbound prescribing information. As GLP-1 use has expanded dramatically, understanding the full spectrum of effects helps contextualize reports of hair-related changes during treatment.
Hair loss, or alopecia, has been reported by patients using GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists. This adverse effect is now documented in FDA-approved prescribing information for some agents in this class. According to the Wegovy (semaglutide 2.4 mg) label, alopecia was reported in 3.5% of patients versus 1.0% on placebo. The Zepbound (tirzepatide) label similarly notes alopecia as an adverse reaction. The relationship between these medications and hair shedding appears to be primarily associated with rapid weight loss rather than a direct pharmacological effect on hair follicles.
Reports from patient experiences and post-marketing surveillance suggest that hair thinning or increased shedding may occur several months after initiating therapy, typically coinciding with periods of rapid weight loss. The true prevalence remains uncertain beyond what is documented in clinical trials. Hair loss has been documented with various GLP-1 and GIP/GLP-1 agents, though causality and whether this represents a true class effect remain unproven.
The temporal relationship between starting therapy and noticing hair changes typically spans 3 to 6 months, which aligns with the natural hair growth cycle and the timing of telogen effluvium—a common form of temporary hair shedding triggered by physiological stress. Clinical distinction between medication-induced effects and weight-loss-associated changes remains challenging. Current evidence does not support permanent hair follicle damage from these medications, and most reported cases describe temporary shedding with eventual regrowth. Healthcare providers should acknowledge patient concerns about hair changes while providing appropriate context about the likely multifactorial nature of this phenomenon and its generally self-limited course.
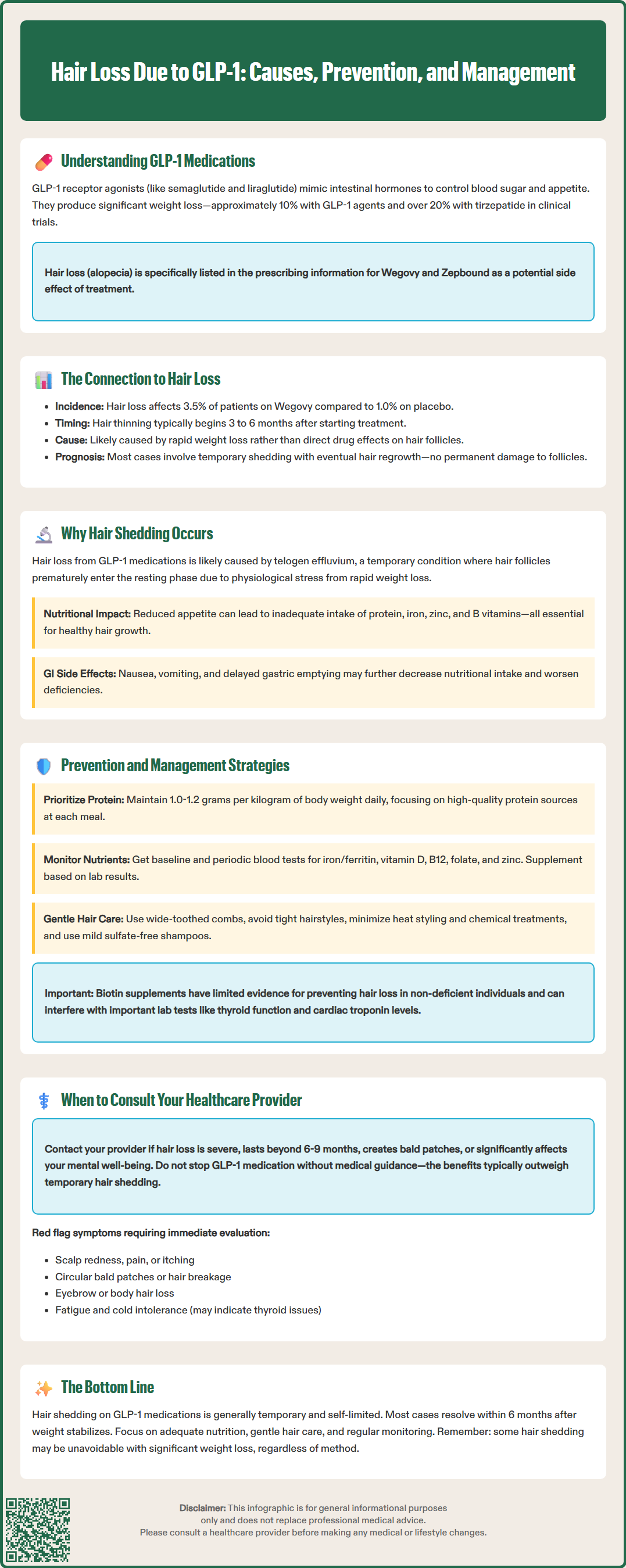
The mechanisms underlying hair loss during GLP-1 therapy likely involve multiple contributing factors rather than a single direct drug effect. The most plausible explanation centers on telogen effluvium, a form of temporary hair shedding that occurs when a significant proportion of hair follicles prematurely enter the resting (telogen) phase of the hair growth cycle. This condition commonly follows major physiological stressors, including rapid weight loss, caloric restriction, and nutritional deficiencies.
Rapid weight reduction, a hallmark of GLP-1 therapy, represents a metabolic stress that can trigger telogen effluvium. When the body experiences substantial caloric deficit and metabolic changes, it may prioritize essential functions over non-essential processes like hair growth. Studies of patients undergoing bariatric surgery or following very-low-calorie diets have documented similar patterns of hair shedding, typically beginning 2 to 4 months after the weight loss period begins. The hair growth cycle's natural timeline explains this delay: follicles that enter telogen phase require several months before the hair shaft is released and shedding becomes noticeable.
Nutritional factors play a significant role. Patients on GLP-1 medications often experience reduced appetite and early satiety, potentially leading to inadequate intake of essential nutrients critical for hair health. Key deficiencies that may contribute to hair loss include:
Protein: Insufficient protein intake impairs keratin production, the structural protein of hair
Iron: Low iron stores and anemia commonly cause diffuse hair shedding
Zinc: Essential for hair follicle function and protein synthesis
B vitamins: Support cellular metabolism in rapidly dividing hair follicle cells
Additionally, the gastrointestinal effects of GLP-1 medications—including nausea, vomiting, and delayed gastric emptying—may reduce nutritional intake even further. The physiological stress of adapting to significant metabolic changes, combined with potential micronutrient deficiencies, creates conditions conducive to temporary hair shedding. It remains uncertain whether GLP-1 receptor activation itself has any direct effect on hair follicle biology, though current evidence does not support this mechanism.
Proactive nutritional management represents the cornerstone of preventing and managing hair loss during GLP-1 treatment. Patients should work with healthcare providers or registered dietitians to ensure adequate intake of essential nutrients despite reduced appetite. Protein intake deserves particular attention, with recommendations typically ranging from 1.0-1.2 grams per kilogram of body weight daily, individualized based on clinical status. Patients with kidney disease may require modified protein goals under medical supervision. High-quality protein sources should be prioritized at each meal, even when portions are smaller than pre-treatment intake.
Micronutrient supplementation may be beneficial, though ideally guided by laboratory assessment rather than empiric supplementation. Baseline and periodic monitoring might include:
Complete blood count to assess for anemia
Ferritin levels (iron stores), with management of documented iron deficiency per clinical guidelines
Vitamin D, B12, and folate levels
Zinc levels if deficiency is suspected based on clinical presentation
Thyroid function tests to exclude concurrent thyroid dysfunction
A standard multivitamin may be appropriate for individuals with significantly reduced food intake, with targeted supplementation based on laboratory results. Some clinicians discuss biotin supplementation, though evidence for its efficacy in non-deficient states remains limited. Patients should be informed that biotin supplementation can interfere with certain laboratory tests, including thyroid function and cardiac troponin assays, as noted in FDA safety communications. Patients taking biotin should inform all healthcare providers and laboratory personnel about its use.
Gentle hair care practices can minimize mechanical hair loss during periods of increased shedding. Recommendations include using wide-toothed combs, avoiding tight hairstyles, minimizing heat styling and chemical treatments, and using mild, sulfate-free shampoos. Scalp massage may promote circulation, though evidence for its effectiveness is limited.
The rate of weight loss may influence hair shedding risk. While not always feasible or appropriate, a more gradual weight reduction approach might reduce metabolic stress and associated hair loss. However, any medication dosing or titration should follow FDA-approved schedules and be directed by healthcare providers. Patients should understand that some degree of hair shedding may be an unavoidable consequence of significant weight reduction, regardless of the method used to achieve it. For some patients, topical minoxidil (available over-the-counter) may help accelerate recovery from telogen effluvium, though this should be discussed with a healthcare provider.
While mild to moderate hair shedding during GLP-1 therapy often represents a self-limited condition that improves with time and nutritional optimization, certain circumstances warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience severe or progressive hair loss that continues beyond 6 to 9 months, involves large bald patches, or significantly impacts quality of life and psychological well-being.
Red flag symptoms that require evaluation include:
Hair loss accompanied by scalp changes such as redness, scaling, itching, or pain
Patchy hair loss in distinct circular areas (suggesting alopecia areata)
Hair breakage rather than shedding from the root
Loss of eyebrow or body hair in addition to scalp hair
Associated symptoms such as fatigue, cold intolerance, or unexplained weight changes beyond expected GLP-1 effects
These features may indicate alternative or additional diagnoses requiring specific treatment. Conditions to consider include androgenetic alopecia, autoimmune alopecia, thyroid disorders, tinea capitis (fungal infection), lichen planopilaris or other scarring alopecias, systemic illness, or other dermatologic conditions unrelated to GLP-1 therapy or weight loss.
Healthcare providers should conduct a thorough assessment including detailed history of the hair loss pattern, timeline, and associated symptoms. Physical examination should evaluate the scalp, hair density and distribution, and signs of other dermatologic or systemic conditions. A hair pull test—gently pulling on approximately 50-60 hairs—can help assess active shedding when performed by a clinician, with more than 5-6 hairs released suggesting active telogen effluvium. Laboratory investigation should include complete blood count, ferritin, thyroid function, and other tests based on clinical suspicion.
Referral to a dermatologist may be appropriate for diagnostic uncertainty, severe or atypical presentations, suspected scarring alopecia, or cases not improving with conservative management. In some instances, scalp biopsy may be necessary to establish a definitive diagnosis. Importantly, patients should not discontinue GLP-1 therapy without medical guidance, as the benefits for diabetes management or weight loss typically outweigh the temporary inconvenience of hair shedding. Telogen effluvium typically resolves within 6 months after the trigger stabilizes. Shared decision-making should weigh the significance of hair changes against treatment benefits, with reassurance that most cases resolve spontaneously as weight stabilizes and nutritional status improves. Documentation of hair loss concerns in the medical record ensures appropriate monitoring and follow-up care.
No, hair loss associated with GLP-1 medications is typically temporary telogen effluvium that resolves within 6 months after weight stabilizes. Current evidence does not support permanent hair follicle damage from these medications.
According to FDA prescribing information, alopecia was reported in 3.5% of patients taking Wegovy (semaglutide 2.4 mg) compared to 1.0% on placebo. The true prevalence may vary as post-marketing surveillance continues.
Ensure adequate protein intake (1.0-1.2 g/kg daily), work with your healthcare provider to monitor and address nutritional deficiencies (especially iron, zinc, and B vitamins), and practice gentle hair care. A registered dietitian can help optimize nutrition despite reduced appetite.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.