LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Holding GLP-1 prior to colonoscopy has become an important consideration as these medications gain widespread use for diabetes and weight management. GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) slow gastric emptying, which may affect procedural safety during sedation. Current US guidance from the American Society of Anesthesiologists and gastroenterology societies emphasizes individualized risk assessment rather than routine medication holds. Most patients can safely continue therapy with appropriate precautions, including a 24-hour liquid diet before the procedure. Understanding when medication adjustments may be warranted requires clear communication between patients and their healthcare teams.
Quick Answer: Most patients taking GLP-1 medications can safely continue therapy before colonoscopy with a 24-hour liquid diet and individualized risk assessment, though some higher-risk patients may benefit from temporary medication holds.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists have become widely prescribed medications for type 2 diabetes and weight management in the United States. These drugs—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—work by mimicking a natural hormone that regulates blood sugar and appetite. Tirzepatide (Mounjaro, Zepbound) works through a similar but distinct mechanism as a dual GIP/GLP-1 receptor agonist. These medications' effects on gastric function create important considerations for patients scheduled to undergo colonoscopy or other endoscopic procedures.
These medications slow gastric emptying, meaning food and liquids remain in the stomach longer than normal. This pharmacologic effect, while beneficial for glycemic control and satiety, has prompted discussions about potential safety considerations during procedures requiring sedation or anesthesia. In some patients, particularly those recently starting therapy or experiencing gastrointestinal symptoms, gastric contents may be retained even after appropriate fasting periods.
The concern has gained attention as use of these medications has expanded dramatically. Some anesthesiologists and gastroenterologists have reported cases of retained gastric contents in certain patients who followed standard pre-procedure fasting instructions while continuing their GLP-1 medications. This has led medical societies to issue guidance on managing these medications before elective procedures. Current evidence suggests a risk-stratified approach, with most patients able to continue therapy with appropriate precautions, while some higher-risk individuals may benefit from temporary medication adjustments. This requires individualized assessment and clear communication between patients and their healthcare teams.
The primary safety consideration with GLP-1 receptor agonists before colonoscopy centers on pulmonary aspiration during sedation. Aspiration occurs when gastric contents enter the respiratory tract, potentially causing aspiration pneumonitis (chemical lung injury), aspiration pneumonia (infectious complication), or acute airway obstruction. While aspiration during procedural sedation is relatively uncommon, it carries significant morbidity when it does occur.
GLP-1 medications delay gastric emptying through multiple mechanisms. They activate GLP-1 receptors in the gastric fundus and antrum, reducing gastric motility and pyloric relaxation. This slowed transit means that food consumed before a procedure may remain in the stomach longer than expected, despite patients following standard nil-per-os (NPO) fasting guidelines. Some small studies using gastric ultrasound and upper endoscopy have documented retained food particles in the stomachs of certain patients taking GLP-1 agonists after overnight fasting periods.
The degree of gastric delay varies among medications and between individuals. Shorter-acting agents like liraglutide (daily dosing) may have less prolonged effects than longer-acting weekly formulations such as semaglutide or dulaglutide. Importantly, the gastric-slowing effect often diminishes with continued use (tachyphylaxis). Patient-specific factors that may increase risk include recent dose escalation, higher doses, significant gastrointestinal symptoms, diabetes-related gastroparesis, and autonomic neuropathy.
During moderate or deep sedation for colonoscopy, protective airway reflexes are diminished. If regurgitation occurs, the sedated patient cannot effectively clear their airway, allowing gastric contents to enter the lungs. Anesthesia providers assess this risk and may implement protective strategies based on individual patient factors.
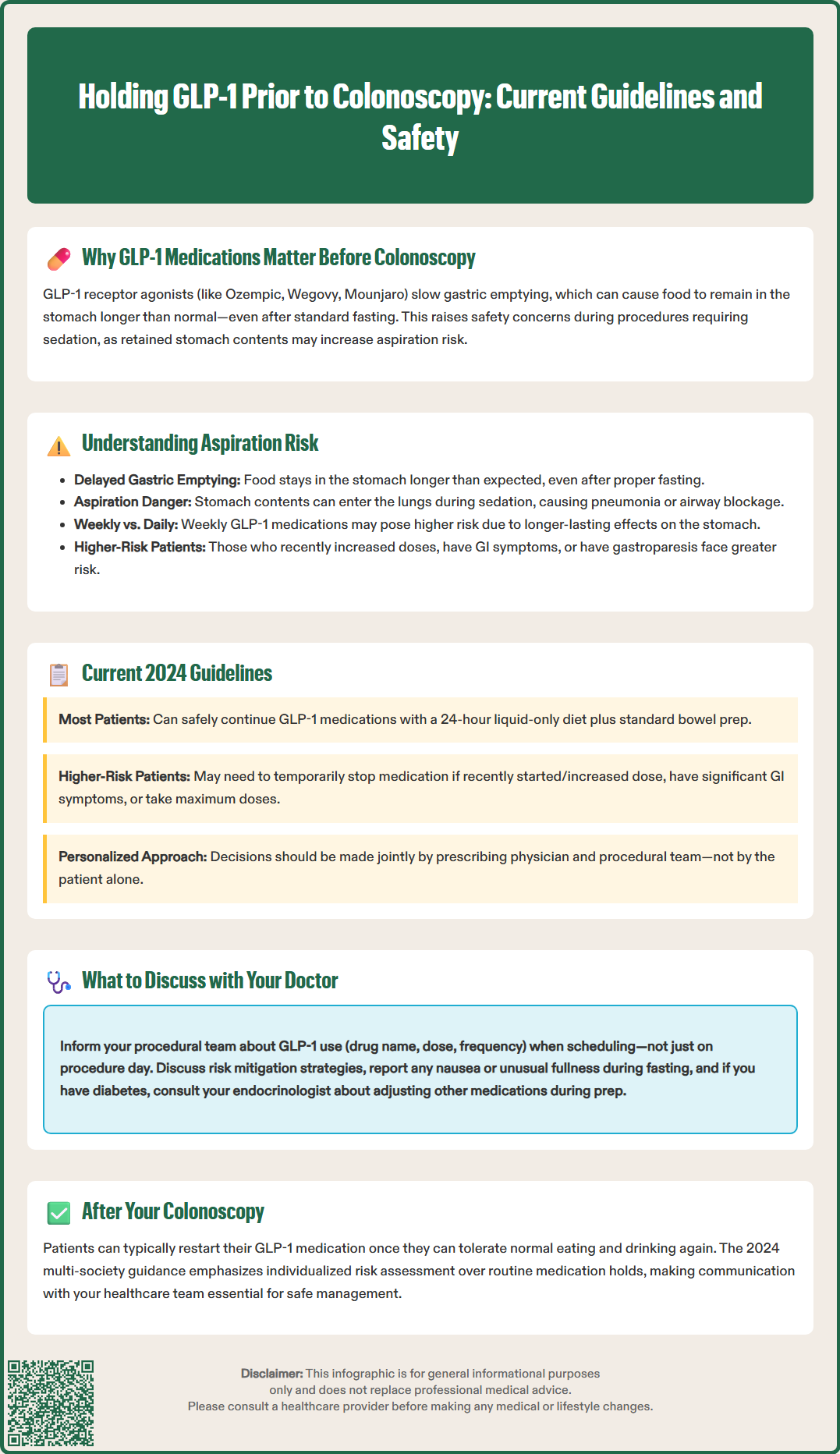
Recommendations for managing GLP-1 medications before colonoscopy have evolved as more clinical experience has accumulated. Current guidance from US medical societies emphasizes a risk-stratified approach rather than universal medication holds.
According to the October 2024 multi-society guidance from the American Society of Anesthesiologists (ASA), American Gastroenterological Association (AGA), American College of Gastroenterology (ACG), American Society for Gastrointestinal Endoscopy (ASGE), and Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), most patients can safely continue their GLP-1 medications before elective procedures with appropriate risk mitigation strategies. These include:
A 24-hour liquid-only diet before the procedure (in addition to the standard colonoscopy preparation)
Consideration of point-of-care gastric ultrasound to assess for residual gastric contents
Anesthesia plan adjustments based on individual risk assessment
However, certain higher-risk patients may benefit from temporarily holding their medication. Risk factors that might warrant consideration of medication adjustment include:
Recent initiation or dose escalation of GLP-1 therapy
Significant gastrointestinal symptoms (nausea, vomiting, early satiety)
Maximum medication doses
Known gastroparesis or other conditions affecting gastric emptying
For patients where holding the medication is deemed appropriate, the duration should be individualized based on the specific medication, patient factors, and clinical judgment. This decision should be made in consultation with both the prescribing physician and the procedural team.
It is essential to emphasize that these are general guidelines, and individual circumstances may warrant different approaches. Patients should never adjust their medication schedule without explicit instruction from their healthcare providers. The timing of medication resumption after colonoscopy should also be discussed, typically allowing restart once normal oral intake is tolerated.
Recognition of gastric emptying effects with GLP-1 medications has prompted guidance from regulatory agencies and professional medical societies to inform clinical practice.
The FDA prescribing information for GLP-1 receptor agonists and tirzepatide notes that these medications cause a delay in gastric emptying, which may impact the absorption of concomitantly administered oral medications. The labels acknowledge this pharmacologic effect but do not provide specific procedural holding periods or pre-procedure recommendations, leaving clinical decisions to healthcare providers based on individual patient assessment.
The 2024 multi-society clinical practice guidance (ASA/AGA/ACG/ASGE/SAGES) represents the most current US consensus on managing these medications before procedures requiring sedation or anesthesia. This guidance recommends that most patients can continue their GLP-1 medications before elective procedures with appropriate risk mitigation strategies, including a 24-hour liquid-only diet before the procedure. The guidance suggests that medication holds or procedure delays should be considered primarily for patients with significant risk factors or symptoms suggesting delayed gastric emptying.
This 2024 guidance updates earlier interim recommendations from the American Society of Anesthesiologists (ASA) issued in 2023, which had suggested more routine holding of these medications (daily formulations on the day of procedure, weekly formulations for one week prior). The evolution of guidance reflects growing clinical experience and recognition of the importance of individualized risk assessment.
The American Diabetes Association (ADA) Standards of Care emphasizes the importance of multidisciplinary communication when temporarily interrupting diabetes medications for procedures. The ADA notes that medication adjustments should be individualized based on the patient's glycemic control, with appropriate glucose monitoring during any interruption period.
It is important to note that guidance continues to evolve as more data emerge. Healthcare facilities may have institution-specific protocols that reflect local expertise and patient populations. The urgency of the procedure must also be weighed against potential risks, with different approaches for elective versus urgent or emergent procedures.
Patients taking GLP-1 medications who are scheduled for colonoscopy should proactively communicate with both their prescribing physician and the gastroenterology team to ensure safe procedural planning. Several key topics warrant discussion well in advance of the scheduled procedure date.
Medication disclosure is the critical first step. Patients should inform the scheduling coordinator and procedural team about all medications, including GLP-1 receptor agonists or dual GIP/GLP-1 receptor agonists, with specific drug name, dose, and frequency. This information should be provided when the colonoscopy is scheduled, not just on the day of the procedure. Many patients use these drugs for weight management rather than diabetes, and these medications may not be captured in routine medication reconciliation if patients do not volunteer the information.
Risk assessment and mitigation strategies should be discussed. Patients should ask about the recommended approach for their specific situation, which may include:
Following a liquid-only diet for 24 hours before the procedure (in addition to the standard bowel preparation)
Whether any medication adjustment is recommended based on individual risk factors
What additional precautions the anesthesia team might take
Diabetes management considerations are important for patients using GLP-1 agonists for glycemic control. If any medication adjustment is recommended, patients should discuss with their endocrinologist or primary care physician:
Whether temporary adjustments to other diabetes medications are needed
How frequently to monitor blood glucose during this period
What glucose levels should prompt contact with the medical team
Bowel preparation instructions should be reviewed carefully. Standard colonoscopy preparation involves consuming large volumes of liquid laxative solutions. Patients should confirm whether any modifications to the standard preparation are recommended based on their medication status.
Signs warranting medical attention should be reviewed. Patients should be instructed to report any symptoms of significant nausea, vomiting, or feeling unusually full during the fasting period before colonoscopy, as these may indicate issues that could affect the procedure.
Finally, patients should understand that if urgent or emergent colonoscopy is required, the procedure may need to proceed regardless of medication status, with the anesthesia team taking appropriate precautions based on individual risk assessment. For elective procedures, a shared decision-making approach between the patient and healthcare team will determine the optimal management strategy.
Most patients can safely continue GLP-1 medications before colonoscopy with appropriate precautions, including a 24-hour liquid-only diet before the procedure. However, patients with certain risk factors such as recent dose increases, significant gastrointestinal symptoms, or known gastroparesis may benefit from temporarily holding their medication based on individualized assessment by their healthcare team.
GLP-1 medications slow gastric emptying, meaning food and liquids remain in the stomach longer than normal. This can potentially increase the risk of pulmonary aspiration during sedation if gastric contents are retained despite standard fasting periods, though this risk varies significantly among individuals.
If your healthcare team determines a medication hold is appropriate, the duration should be individualized based on your specific medication, dosing frequency, and clinical factors. This decision should be made in consultation with both your prescribing physician and procedural team, and patients should never adjust medications without explicit medical instruction.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.