LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

How fast do GLP-1 injections work? GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) begin affecting appetite and blood sugar within days to weeks, but clinically meaningful outcomes develop more gradually. Appetite suppression often occurs within the first one to two weeks, while measurable weight loss typically starts by week four. For patients with type 2 diabetes, blood glucose improvements become apparent within weeks, with hemoglobin A1c reductions evident after 12 to 16 weeks. Understanding this timeline helps set realistic expectations and supports treatment adherence during the critical early months of therapy.
Quick Answer: GLP-1 injections begin suppressing appetite within one to two weeks, with measurable weight loss starting by week four and hemoglobin A1c reductions evident after 12 to 16 weeks.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are injectable medications that mimic a naturally occurring hormone in the body. These medications include semaglutide (Ozempic, Wegovy) and dulaglutide (Trulicity) for both diabetes and weight management, and liraglutide (Victoza for diabetes, Saxenda for weight management). Tirzepatide (Mounjaro for diabetes, Zepbound for weight management) is a dual GIP/GLP-1 receptor agonist with similar effects. Originally developed for type 2 diabetes management, several of these medications have received FDA approval for chronic weight management in adults with obesity (BMI ≥30) or overweight (BMI ≥27) with weight-related comorbidities.
The mechanism of action involves binding to GLP-1 receptors found throughout the body, particularly in the pancreas, brain, and gastrointestinal tract. In the pancreas, these medications stimulate glucose-dependent insulin secretion, meaning they promote insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycemia compared to some other diabetes medications. Simultaneously, these agents suppress glucagon secretion, a hormone that raises blood sugar levels.
In the brain, GLP-1 receptor activation affects areas that regulate appetite and satiety, leading to reduced hunger and increased feelings of fullness. The medications also slow gastric emptying, which prolongs the sensation of fullness after eating and contributes to reduced caloric intake. This multi-system approach explains why these injections are effective for both glycemic control and weight management.
Most GLP-1 receptor agonists are administered subcutaneously once weekly (semaglutide, dulaglutide, tirzepatide) or once daily (liraglutide), though frequency varies by specific medication. Weekly dosing may improve adherence for some patients compared to daily injectable or oral diabetes medications.
Important safety information: These medications carry a boxed warning for risk of thyroid C-cell tumors and are contraindicated in patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). They are not indicated for type 1 diabetes and are not recommended during pregnancy.
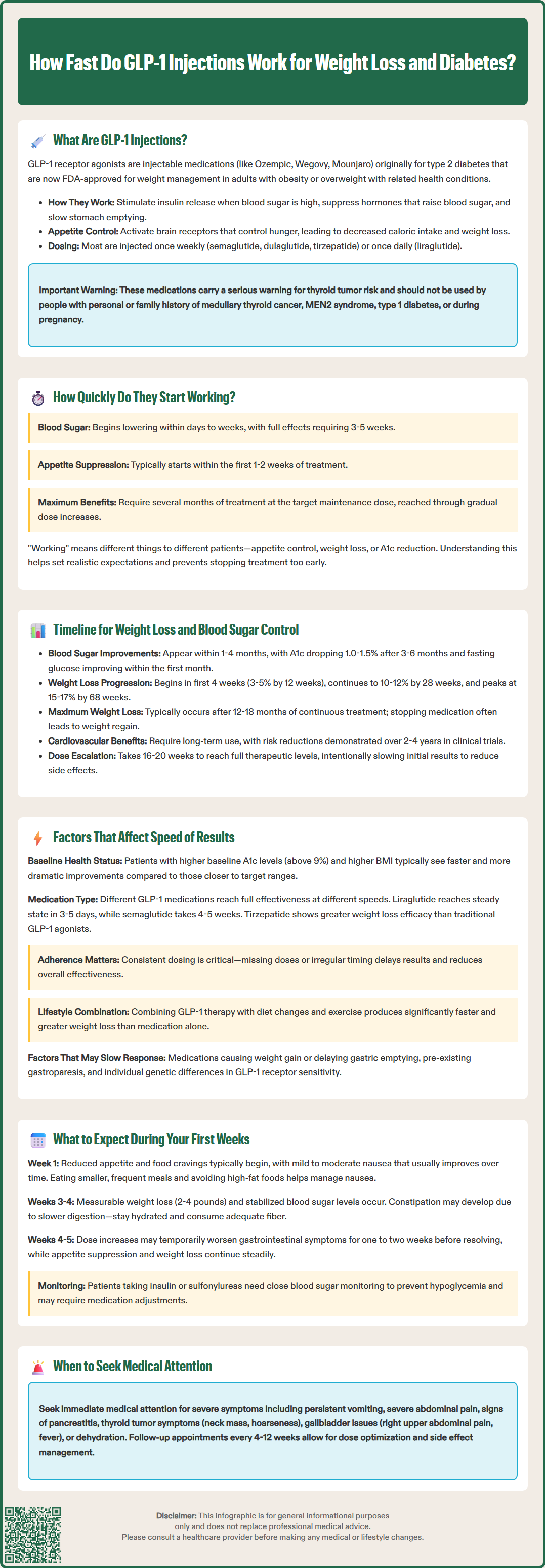
GLP-1 receptor agonists begin exerting physiological effects at different rates depending on the specific medication, though the timeline for clinically meaningful outcomes varies by therapeutic goal. Understanding this distinction helps set appropriate patient expectations and prevents premature discontinuation.
For blood glucose control, the onset of action varies by medication. Daily liraglutide may begin lowering blood sugar within days, while weekly formulations like semaglutide may show initial effects within 1-2 weeks. The full glycemic effect typically develops over several weeks as the medication reaches steady-state concentrations in the bloodstream. For weekly semaglutide, steady state is generally achieved after 4 to 5 weeks of consistent dosing, while liraglutide reaches steady state within 3 to 5 days due to its shorter half-life (approximately 13 hours).
Appetite suppression often occurs more rapidly than weight loss itself. Many patients report decreased hunger and earlier satiety within the first week or two of treatment. This early effect on appetite is mediated by the medication's action on brain receptors that regulate hunger signals. However, the intensity of appetite suppression may vary considerably between individuals.
Gastrointestinal effects, including nausea and delayed gastric emptying, typically manifest within the first few days to weeks of treatment. While these effects contribute to reduced food intake, they are not the primary mechanism of weight loss. According to the American Diabetes Association Standards of Care, GLP-1 receptor agonists produce weight loss through multiple mechanisms including central appetite regulation and delayed gastric emptying, beyond gastrointestinal side effects alone.
It is important to note that "working" means different things for different patients. Some may prioritize rapid appetite control, while others focus on measurable weight loss or hemoglobin A1c reduction. Clinical trials demonstrate that maximal therapeutic effects generally require several months of treatment at the target maintenance dose, which is typically reached through a gradual dose escalation process.
The timeline for achieving therapeutic goals with GLP-1 injections follows a predictable pattern, though individual responses vary. For patients with type 2 diabetes, hemoglobin A1c reductions become apparent within 12 to 16 weeks of initiating therapy. Clinical trials of semaglutide and dulaglutide have demonstrated A1c reductions of 1.0% to 1.5% or more from baseline after three to six months of treatment. Fasting plasma glucose typically improves earlier, with noticeable reductions within the first month.
Weight loss follows a more gradual trajectory. Most patients begin losing weight within the first four weeks of treatment, with the rate of loss varying during the dose escalation phase. According to the STEP 1 trial published in the New England Journal of Medicine, patients taking semaglutide 2.4 mg (Wegovy) achieved approximately:
3% to 5% body weight loss by week 12
10% to 12% body weight loss by week 28
15% to 17% body weight loss by week 68 (maximum effect)
These figures represent average outcomes in clinical trials; individual results vary significantly. The SURMOUNT-1 trial showed that tirzepatide produced even greater weight loss in many patients. Weight loss typically continues for 12 to 18 months before plateauing. The American College of Physicians guidelines note that continued treatment is necessary to maintain weight loss, as discontinuation often leads to weight regain.
For cardiovascular benefits, the timeline extends further. The LEADER trial (liraglutide) and SUSTAIN-6 trial (semaglutide) demonstrated cardiovascular risk reduction over multi-year follow-up periods (approximately 3.8 years and 2.1 years, respectively). More recently, the SELECT trial showed that semaglutide 2.4 mg reduced major adverse cardiovascular events in adults with overweight or obesity without diabetes. These findings underscore that GLP-1 therapy is a long-term intervention rather than a short-term solution.
Patients should understand that dose escalation protocols intentionally slow the initial response. Most GLP-1 medications start at a low dose and gradually increase every four weeks to minimize gastrointestinal side effects. The full therapeutic dose may not be reached until 16 to 20 weeks after initiation, which delays maximal efficacy but improves tolerability and treatment adherence.
Multiple patient-specific and medication-related factors influence the speed and magnitude of response to GLP-1 receptor agonists. Recognizing these variables helps clinicians and patients set realistic expectations and optimize treatment outcomes.
Baseline metabolic status significantly affects response time. Patients with higher baseline hemoglobin A1c levels (above 9%) typically experience more rapid and pronounced glucose reductions compared to those with A1c levels closer to target. Similarly, individuals with higher body mass index may experience greater absolute weight loss, though percentage body weight reduction remains relatively consistent across BMI categories.
Medication-specific pharmacokinetics play a crucial role. Semaglutide has a half-life of approximately one week, while liraglutide has a half-life of 13 hours. This means liraglutide reaches steady-state concentrations within 3 to 5 days, whereas semaglutide requires 4 to 5 weeks. Tirzepatide, a dual GIP/GLP-1 receptor agonist, has demonstrated greater efficacy in clinical trials, including the head-to-head SURMOUNT-5 trial comparing it to semaglutide 2.4 mg, potentially producing more substantial weight loss than traditional GLP-1 agonists alone.
Adherence to dosing schedules directly impacts effectiveness. Missing doses or inconsistent injection timing can delay therapeutic effects and reduce overall efficacy. Weekly formulations may improve adherence compared to daily injections for some patients.
Lifestyle modifications substantially influence outcomes. Patients who combine GLP-1 therapy with dietary changes and increased physical activity typically experience faster and more significant weight loss than those relying on medication alone. The FDA labels for weight management formulations explicitly recommend comprehensive lifestyle intervention as part of treatment.
Concomitant medications may affect response. Medications that delay gastric emptying may alter the speed and magnitude of GLP-1 effects. Additionally, patients taking medications that cause weight gain (certain antipsychotics, antidepressants, or corticosteroids) may experience slower weight loss. Notably, tirzepatide may reduce the effectiveness of oral contraceptives during dose escalation due to delayed gastric emptying; backup contraception may be advised during this period.
Pre-existing gastrointestinal conditions can impact response. Patients with severe gastroparesis may experience altered drug absorption and increased side effects, potentially affecting the speed of therapeutic response.
Genetic and metabolic factors contribute to individual variability. Some patients are naturally more sensitive to GLP-1 receptor activation, while others require higher doses to achieve comparable effects. There is no reliable way to predict individual response before initiating treatment, making therapeutic trials necessary.
The initial weeks of GLP-1 therapy represent a critical adjustment period during which patients experience both therapeutic effects and potential side effects. Setting appropriate expectations improves treatment adherence and patient satisfaction.
Week 1 to 2: Most patients begin noticing reduced appetite and earlier satiety within the first week. Some describe feeling "less food-focused" or experiencing decreased cravings, particularly for high-calorie foods. Gastrointestinal side effects, primarily nausea, may emerge during this period. Nausea is typically mild to moderate and often improves with continued use. Patients should be advised to eat smaller, more frequent meals and avoid high-fat foods, which can exacerbate nausea.
Week 3 to 4: Blood glucose levels begin stabilizing for patients with diabetes. Home glucose monitoring may show reduced fasting and postprandial readings. Weight loss becomes measurable, though typically modest (2 to 4 pounds). Some patients experience constipation during this phase due to slowed gastrointestinal motility. Adequate hydration and dietary fiber intake help manage this side effect.
Week 5 to 8: For weekly formulations, steady-state drug concentrations are achieved, and the first dose escalation typically occurs around week 4 or 5. Patients may experience a temporary increase in gastrointestinal symptoms with each dose increase, though these usually resolve within one to two weeks. Weight loss continues at a steady pace, and appetite suppression becomes more consistent.
Important safety considerations during the initial treatment period include:
Monitoring for severe gastrointestinal symptoms: Persistent vomiting, severe abdominal pain, or signs of pancreatitis (severe upper abdominal pain radiating to the back) require immediate medical evaluation.
Thyroid monitoring: Patients should report any symptoms of thyroid tumors including neck mass, hoarseness, difficulty swallowing, or shortness of breath (boxed warning).
Gallbladder issues: Right upper quadrant pain, fever, or jaundice may indicate gallbladder disease, which has been associated with these medications.
Hypoglycemia risk: Patients taking GLP-1 agonists with insulin or sulfonylureas need close glucose monitoring, as dose adjustments of these medications may be necessary.
Hydration status: Nausea and reduced oral intake can lead to dehydration, potentially causing acute kidney injury, particularly in older adults.
Vision changes: Rapid improvement in blood glucose can temporarily worsen diabetic retinopathy; patients with pre-existing retinopathy should have ophthalmology follow-up.
Injection site reactions: Mild redness or itching at injection sites is common but should resolve quickly.
Patients should contact their healthcare provider if they experience severe or persistent side effects, are unable to tolerate the medication, or have concerns about their response to treatment. Regular follow-up appointments, typically scheduled every 4 to 12 weeks during the initial treatment phase, allow for dose adjustments, side effect management, and monitoring of therapeutic outcomes. The American Diabetes Association recommends assessing hemoglobin A1c every three months until glycemic targets are achieved, then at least twice yearly thereafter. For weight management, inadequate response (less than 5% weight loss after several months at maintenance dose) may warrant reassessment of the treatment approach.
Most patients report decreased hunger and earlier satiety within the first one to two weeks of starting GLP-1 therapy. The intensity of appetite suppression varies between individuals and typically becomes more consistent as the medication reaches steady-state concentrations.
Blood glucose levels begin improving within one to two weeks for most patients with type 2 diabetes, with fasting plasma glucose showing noticeable reductions within the first month. Hemoglobin A1c reductions become apparent after 12 to 16 weeks of consistent treatment.
GLP-1 medications use gradual dose escalation protocols, increasing every four weeks to minimize side effects, which means the full therapeutic dose may not be reached until 16 to 20 weeks. Weight loss continues progressively for 12 to 18 months before plateauing, with maximal effects requiring sustained treatment at maintenance doses.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.