LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Semaglutide for weight loss raises an important question for patients and clinicians: how long can you take semaglutide for weight loss? As a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for chronic weight management, semaglutide (marketed as Wegovy for obesity) represents a long-term treatment approach rather than a short-term solution. Understanding the duration of therapy, safety considerations, and what happens after discontinuation is essential for making informed decisions about this medication. This article examines FDA guidance, clinical trial data, and current medical practice regarding semaglutide treatment duration.
Quick Answer: Semaglutide is FDA-approved for chronic weight management without a specified maximum treatment duration, and patients may continue therapy indefinitely as long as they respond well and tolerate the medication.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist originally developed for type 2 diabetes management and subsequently approved by the FDA for chronic weight management. The medication is available under different brand names: Ozempic (approved for diabetes) and Wegovy (specifically approved for weight loss). Both formulations contain the same active ingredient but differ in dosing protocols and FDA-approved indications.
The mechanism of action involves mimicking the naturally occurring GLP-1 hormone, which plays multiple roles in metabolic regulation. Semaglutide binds to GLP-1 receptors in the brain, particularly in areas that control appetite and food intake, leading to reduced hunger and increased feelings of fullness. Additionally, the medication slows gastric emptying, which prolongs satiety after meals and helps reduce overall caloric intake.
For weight loss purposes, semaglutide is administered as a once-weekly subcutaneous injection. The FDA-approved indication is for adults with obesity (body mass index ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as hypertension, type 2 diabetes, or dyslipidemia. Clinical trials have demonstrated average weight loss of about 15% of initial body weight when combined with lifestyle modifications including reduced-calorie diet and increased physical activity, with some individuals achieving ≥20% weight loss.
In 2024, Wegovy also received FDA approval to reduce the risk of major adverse cardiovascular events in adults with established cardiovascular disease and obesity or overweight.
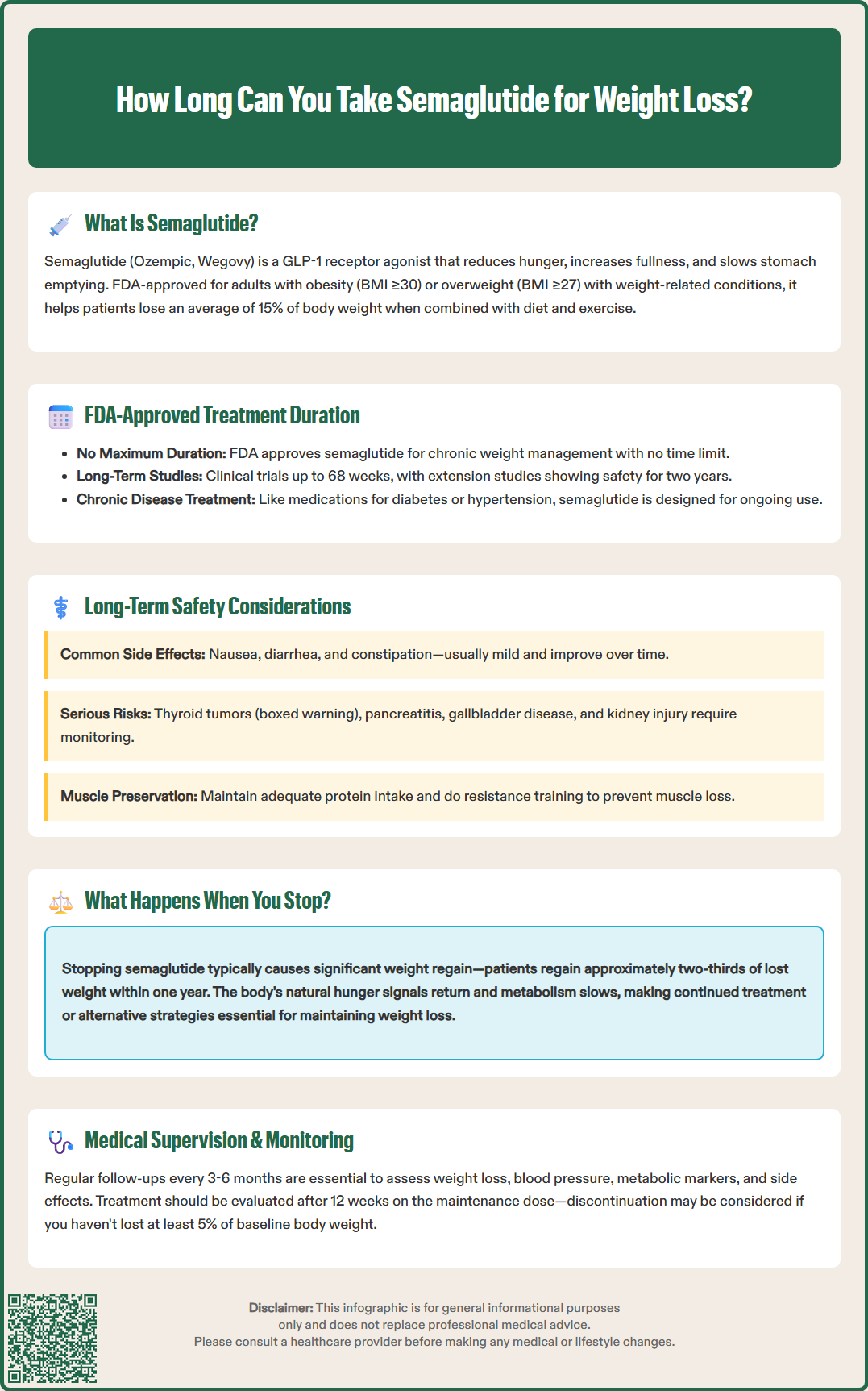
The FDA has approved semaglutide for chronic weight management without specifying a maximum treatment duration. This approval framework reflects the current medical understanding that obesity is a chronic, relapsing disease requiring long-term pharmacological intervention in many patients. The prescribing information for Wegovy does not establish a predetermined endpoint for therapy, instead emphasizing individualized treatment decisions based on clinical response and tolerability.
Clinical trial data supporting FDA approval included studies extending up to 68 weeks (approximately 16 months), with extension studies following participants for up to two years. These trials demonstrated sustained weight loss and metabolic benefits throughout the treatment period. The STEP (Semaglutide Treatment Effect in People with obesity) clinical trial program provided the primary evidence base, showing continued efficacy without significant safety concerns emerging over extended use.
According to the FDA prescribing information, treatment response should be evaluated after 12 weeks on the maintenance dose (2.4 mg). If a patient has not lost at least 5% of baseline body weight at this point, discontinuation should be considered. This assessment timing is important, as it occurs after completing the dose escalation phase and allowing sufficient time on the therapeutic dose.
Current clinical practice guidelines from organizations such as the American Association of Clinical Endocrinology (AACE), the Endocrine Society, and the American Diabetes Association (ADA) support long-term use of anti-obesity medications when clinically indicated. Healthcare providers typically reassess treatment continuation at regular intervals, generally every 3-6 months. If adverse effects outweigh benefits, discontinuation should be considered. Conversely, patients who respond well may continue treatment indefinitely as part of comprehensive weight management, similar to the approach used for other chronic conditions such as hypertension or diabetes.
Long-term safety data for semaglutide continues to accumulate, with current evidence extending beyond two years of continuous use. The most commonly reported adverse effects are gastrointestinal in nature, including nausea, diarrhea, vomiting, constipation, and abdominal pain. These symptoms typically occur during dose escalation and often diminish over time as patients develop tolerance. Most gastrointestinal effects are mild to moderate in severity and can be managed through slower dose titration and dietary modifications.
More serious but less common adverse effects require ongoing monitoring. Semaglutide carries a boxed warning regarding the risk of thyroid C-cell tumors, based on rodent studies showing increased incidence of medullary thyroid carcinoma. While this risk has not been established in humans, semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Routine screening with calcitonin or thyroid ultrasound is not recommended by the FDA.
Other important risks include acute pancreatitis, gallbladder disease (including cholelithiasis and cholecystitis), acute kidney injury (particularly in patients experiencing severe gastrointestinal symptoms), hypoglycemia when used with insulin or insulin secretagogues, increased heart rate, diabetic retinopathy complications in patients with diabetes, and suicidal behavior or ideation. Semaglutide is contraindicated during pregnancy and should be discontinued at least 2 months before a planned pregnancy due to its long half-life.
Recent post-marketing surveillance has identified additional considerations. Some patients report persistent gastrointestinal symptoms that may affect quality of life and nutritional status. There have been reports of gastroparesis (delayed gastric emptying) in some individuals, and semaglutide is not recommended in patients with severe gastroparesis. Patients should be counseled about adequate protein intake and nutritional monitoring during treatment, with consideration of dietitian consultation and resistance training to help preserve muscle mass.
Regarding effectiveness, clinical data demonstrates that weight loss plateaus typically occur around 60-68 weeks of treatment, after which weight tends to stabilize rather than continue declining. Maintenance of weight loss requires continued medication use along with sustained lifestyle modifications. Studies show that metabolic benefits—including improvements in blood pressure, lipid profiles, glycemic control, and markers of cardiovascular risk—are maintained as long as treatment continues and weight loss is sustained.
Discontinuation of semaglutide typically results in weight regain, a phenomenon well-documented in clinical trials and real-world observations. The STEP 1 trial extension study demonstrated that participants who stopped semaglutide after 68 weeks regained approximately two-thirds of their lost weight within one year of discontinuation. This pattern of weight regain reflects the underlying pathophysiology of obesity as a chronic disease characterized by biological adaptations that defend against weight loss.
The physiological mechanisms driving weight regain after semaglutide cessation are multifactorial. When the medication is withdrawn, the appetite-suppressing effects diminish, leading to increased hunger and food intake. Additionally, metabolic adaptations that occur during weight loss—including reduced energy expenditure and hormonal changes that promote weight regain—are no longer counteracted by the medication's effects. These biological factors often override behavioral interventions, making weight maintenance challenging without pharmacological support.
Patients should be counseled that stopping semaglutide does not pose immediate medical dangers in most cases, but the decision should be made collaboratively with healthcare providers. Abrupt discontinuation is generally safe from a pharmacological standpoint, as semaglutide does not cause physical dependence or withdrawal symptoms. However, the medication should be stopped immediately if serious adverse effects occur, such as signs of pancreatitis (severe abdominal pain), symptoms of thyroid tumors (neck mass, difficulty swallowing), or severe allergic reactions. Semaglutide must be discontinued if pregnancy occurs or at least 2 months before a planned pregnancy.
For patients who need to discontinue semaglutide due to side effects, cost, or personal preference, transitioning to alternative weight management strategies is essential. This may include switching to other FDA-approved anti-obesity medications with different mechanisms of action, intensifying behavioral interventions, or considering bariatric surgery for eligible candidates. Any trial off therapy should be clinician-guided with alternative supports in place, as medication pauses typically lead to weight regain without a comprehensive plan.
Comprehensive medical supervision is essential throughout semaglutide treatment, beginning with thorough baseline assessment and continuing with regular monitoring intervals. Initial evaluation should include measurement of body weight, BMI, waist circumference, blood pressure, and relevant laboratory tests. Baseline laboratory work typically includes fasting glucose or hemoglobin A1c, lipid panel, liver function tests, and renal function (serum creatinine and estimated glomerular filtration rate). Pregnancy testing should be performed when applicable, and patients who could become pregnant should be counseled on contraception during treatment.
During the dose escalation phase, patients should be monitored closely for tolerability and adverse effects. The standard titration schedule for Wegovy involves gradual dose increases over 16-20 weeks to reach the maintenance dose of 2.4 mg weekly. More frequent contact during this period—whether through office visits, telehealth appointments, or structured check-ins—helps identify and manage gastrointestinal symptoms early, potentially improving treatment adherence. Patients should be educated about warning signs requiring immediate medical attention, including severe abdominal pain (possible pancreatitis), persistent vomiting leading to dehydration, visual changes, or symptoms of allergic reactions.
Once patients reach the maintenance dose, ongoing monitoring should occur at least every 3-6 months. These visits should assess weight trajectory, blood pressure, and metabolic parameters. Healthcare providers should evaluate for adverse effects, review medication adherence, and reinforce lifestyle modifications including nutrition and physical activity. Specific monitoring considerations include heart rate, renal function if severe gastrointestinal symptoms occur, hypoglycemia risk if used with insulin or sulfonylureas, and diabetic retinopathy in patients with diabetes. Patients should be monitored for depression, suicidal thoughts, or unusual mood changes.
Long-term treatment decisions should be individualized based on response and risk-benefit assessment. Per the FDA label, if a patient has not lost at least 5% of baseline body weight after 12 weeks on the maintenance dose (2.4 mg), discontinuation should be considered. Semaglutide should not be coadministered with other GLP-1 receptor agonists or other semaglutide-containing products. Shared decision-making is crucial, incorporating discussion of treatment goals, potential risks, expected benefits, cost considerations, and alternative options. Documentation of these discussions and the rationale for continuing or discontinuing treatment supports high-quality, patient-centered care.
No, the FDA has not established a maximum treatment duration for semaglutide. It is approved for chronic weight management, and patients who respond well and tolerate the medication may continue treatment indefinitely under medical supervision.
Yes, most patients experience weight regain after discontinuing semaglutide. Clinical trials show that participants regained approximately two-thirds of their lost weight within one year of stopping the medication, reflecting obesity's chronic nature and biological adaptations that promote weight regain.
Patients should be monitored closely during the initial dose escalation phase, then at least every 3-6 months once on the maintenance dose. Monitoring includes weight assessment, blood pressure, metabolic parameters, adverse effects evaluation, and individualized treatment continuation decisions.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.