LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

How long does it take for semaglutide to suppress appetite? Most patients notice appetite reduction within the first one to two weeks of starting treatment, with effects intensifying as the dose increases over subsequent months. Semaglutide, a GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management, works by activating brain receptors that regulate hunger and slowing gastric emptying. Understanding the timeline for appetite suppression helps patients set realistic expectations and optimize their treatment outcomes. This article examines the mechanisms, timeline, and factors influencing semaglutide's appetite-suppressing effects.
Quick Answer: Most patients experience noticeable appetite suppression within one to two weeks of starting semaglutide, with effects intensifying during dose escalation and peak suppression typically occurring at 16-20 weeks.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics the action of naturally occurring GLP-1, a hormone released by the intestines after eating. This medication works through multiple mechanisms to reduce appetite and promote weight loss, making it effective for type 2 diabetes treatment and, specifically in the case of Wegovy (semaglutide 2.4 mg), FDA-approved for chronic weight management.
The primary mechanism involves binding to GLP-1 receptors in specific areas of the brain, particularly the hypothalamus and brainstem regions that regulate hunger and satiety. When semaglutide activates these receptors, it enhances feelings of fullness and reduces hunger signals. Additionally, the medication slows gastric emptying—the rate at which food leaves the stomach—which prolongs the sensation of fullness after meals and helps reduce overall food intake. This gastric emptying effect may attenuate somewhat over time, though appetite suppression continues through multiple pathways.
Research suggests semaglutide may also influence the brain's reward pathways associated with food intake and eating behavior. This may contribute to reduced interest in high-calorie foods, though human clinical evidence in this area continues to evolve. Through these combined mechanisms, semaglutide addresses both physiological hunger and aspects of eating behavior.
The medication's extended half-life of approximately one week allows for once-weekly subcutaneous administration, maintaining steady blood levels that support consistent drug activity. This pharmacokinetic profile distinguishes semaglutide from shorter-acting GLP-1 agonists and contributes to its clinical effectiveness.
Most patients begin experiencing noticeable appetite suppression within the first one to two weeks of starting semaglutide, though the timeline varies considerably among individuals. Many patients report changes in hunger and fullness during these initial weeks, with effects typically becoming more pronounced as treatment continues.
During the dose escalation phase—spanning 16 weeks for Wegovy's weight management formulation—appetite suppression generally intensifies as the dosage increases. The FDA-approved titration schedule starts at a low dose (0.25 mg weekly for Ozempic or Wegovy) to minimize gastrointestinal side effects, gradually increasing every four weeks. Many patients report significant appetite reduction once they reach therapeutic maintenance doses (0.5-2 mg for Ozempic in diabetes management, 2.4 mg for Wegovy in weight management).
Steady-state drug levels are typically achieved approximately 4-5 weeks after any dose change. Peak appetite suppression often coincides with reaching the maintenance dose, usually between weeks 16-20 of treatment for those following the standard titration schedule. Research from the pivotal STEP trials demonstrates that maximal weight loss—which correlates with but is not solely attributable to appetite control—occurs around 60 to 68 weeks of continuous treatment.
It is important to note that appetite suppression may not be uniform throughout treatment. Some patients report variations in hunger levels throughout the week, particularly in the days following their injection versus the days before the next dose. Additionally, the degree of appetite reduction may plateau or diminish slightly over time as physiological adaptation occurs, though clinical efficacy generally persists with continued use.
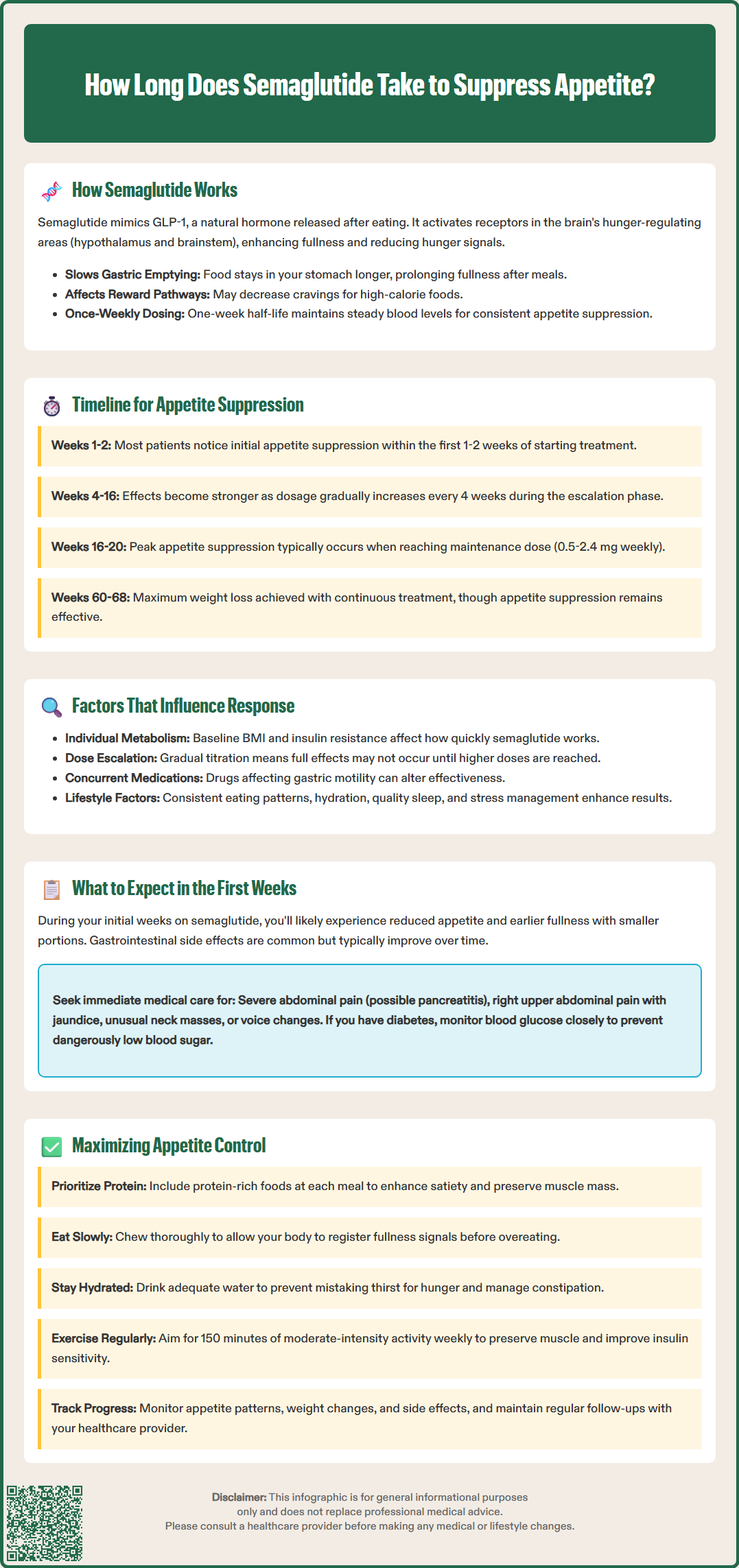
Several patient-specific and treatment-related factors influence the onset and intensity of appetite suppression with semaglutide. Understanding these variables helps set realistic expectations and optimize treatment outcomes.
Individual metabolic factors play a significant role. Patients with higher baseline body mass index (BMI) may experience different response patterns compared to those with lower BMI. Insulin resistance and other metabolic factors may influence how quickly and robustly an individual responds to the medication. Some research suggests potential variations in efficacy across demographic groups, though individual response remains difficult to predict.
Dosage and titration schedule directly impact the timeline for appetite effects. The gradual dose escalation recommended by the FDA balances efficacy with tolerability, but it means that full appetite suppression may not occur until higher doses are reached. Patients who require slower titration due to gastrointestinal side effects may experience a delayed onset of maximal appetite control.
Concurrent medications and medical conditions can modify semaglutide's effects. Medications that affect gastric motility, such as opioids or anticholinergics, may alter the drug's impact on satiety. Severe gastrointestinal disorders may influence tolerability and effectiveness. Semaglutide can also delay the absorption of some oral medications due to its effect on gastric emptying, which may require monitoring for drugs with a narrow therapeutic index.
Safety considerations include important FDA warnings. Semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Caution is advised in patients with a history of pancreatitis, and monitoring for gallbladder disease is recommended. For patients with diabetes, the risk of diabetic retinopathy complications and hypoglycemia (when used with insulin or sulfonylureas) should be discussed with healthcare providers.
Lifestyle factors including diet composition, meal timing, sleep quality, and stress levels interact with semaglutide's pharmacological effects. Patients who maintain consistent eating patterns and adequate hydration often report more predictable appetite control. Psychological factors, including eating behaviors and food relationships, also influence the subjective experience of appetite suppression and treatment satisfaction.
The initial weeks of semaglutide treatment represent an adjustment period during which patients experience both therapeutic effects and potential side effects. Understanding what to expect helps patients navigate this phase successfully and maintain treatment adherence.
Week 1-2: Most patients notice subtle changes in appetite and fullness during the first week. You may find that smaller portions satisfy you, or that you think about food less frequently between meals. Some individuals experience mild nausea, which paradoxically may contribute to reduced appetite. It is important to distinguish between therapeutic appetite reduction and nausea-induced food aversion—the former is desirable, while the latter may require dose adjustment or supportive management.
Gastrointestinal adaptation is common during the first month. Nausea, occasional vomiting, diarrhea, or constipation are frequently reported side effects, typically peaking during the first few weeks and improving with continued use. These effects result from slowed gastric emptying and altered gut motility. Eating smaller, more frequent meals and avoiding high-fat foods can minimize discomfort. If gastrointestinal symptoms are severe or persistent, consult your healthcare provider before the next scheduled dose increase.
Safety monitoring is essential. Seek immediate medical attention for severe or persistent abdominal pain (with or without vomiting), which could indicate pancreatitis; right upper abdominal pain, jaundice or dark urine, which may suggest gallbladder problems; or any unusual neck mass or voice changes. If you have diabetes, monitor blood glucose levels closely, especially if taking insulin or sulfonylureas, as dose adjustments may be needed to prevent hypoglycemia. Report any vision changes promptly, particularly if you have diabetic retinopathy.
Behavioral adjustments become necessary as appetite changes. Many patients report feeling satisfied with significantly less food than previously required, which may feel unusual initially. Some describe a reduced interest in snacking or decreased cravings for specific foods. Learning to recognize and respond to new satiety signals is an important part of early treatment.
Important note: Semaglutide should not be used during pregnancy or by women planning pregnancy. Discuss effective contraception with your healthcare provider if you are of childbearing potential.
While semaglutide provides pharmacological appetite suppression, combining medication with evidence-based lifestyle strategies optimizes outcomes and supports sustainable weight management.
Nutritional strategies enhance semaglutide's effects. Focus on protein-rich foods at each meal, as protein promotes satiety and helps preserve lean muscle mass during weight loss. The American Diabetes Association recommends individualized nutrition plans, but generally suggests emphasizing vegetables, lean proteins, whole grains, and healthy fats while limiting ultra-processed foods. Because semaglutide slows gastric emptying, eating slowly and chewing thoroughly improves comfort and allows satiety signals to register before overeating occurs.
Hydration and meal timing may impact appetite control. Adequate fluid intake helps prevent dehydration, which can be mistaken for hunger, and helps manage constipation—a common side effect. Hydration needs should be individualized, with caution in those with heart or kidney disease. Establishing regular meal times helps create predictable eating patterns. Some patients report that eating their largest meal earlier in the day works better for them, though this is based on individual preference rather than clinical evidence.
Physical activity complements semaglutide's metabolic effects. While the medication reduces appetite, exercise helps maintain muscle mass, improves insulin sensitivity, and supports cardiovascular health. The U.S. Department of Health and Human Services and American Diabetes Association recommend at least 150 minutes of moderate-intensity activity weekly for adults, adjusted based on individual capabilities and medical conditions.
Additional considerations for optimizing treatment include moderating alcohol consumption due to pancreatitis risk and managing constipation through adequate fiber, fluids, and physical activity. For patients experiencing significant gastrointestinal side effects, working with a registered dietitian can help develop strategies to maintain adequate nutrition while minimizing discomfort.
Monitoring and adjustment ensure optimal outcomes. Track your response to treatment, including appetite patterns, food intake, weight changes, and any side effects. Regular follow-up with your healthcare provider allows for dose optimization and addresses any concerns. If appetite suppression diminishes over time or plateaus occur, your provider may adjust the dose (within FDA-approved ranges) or recommend additional interventions. Remember that semaglutide is most effective as part of a comprehensive weight management program that includes behavioral support, nutritional counseling, and ongoing medical supervision.
Most patients begin experiencing noticeable appetite suppression within the first one to two weeks of starting semaglutide. Effects typically become more pronounced as the dose increases during the 16-week titration period, with peak appetite control often occurring around weeks 16-20 of treatment.
Semaglutide has a one-week half-life allowing once-weekly dosing, but some patients report variations in hunger levels throughout the week. Appetite suppression may be strongest in the days following injection and slightly less pronounced before the next dose, though individual experiences vary.
If appetite suppression diminishes or plateaus, consult your healthcare provider who may adjust your dose within FDA-approved ranges or recommend additional interventions. Combining medication with consistent nutrition strategies, physical activity, and behavioral support helps maintain long-term effectiveness.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.