LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Can you overdose on semaglutide? While semaglutide overdose differs from traditional drug overdoses, taking excessive doses can cause serious complications. Semaglutide, a GLP-1 receptor agonist approved for type 2 diabetes and chronic weight management, does not have an established lethal dose in humans. However, exceeding recommended doses significantly increases the risk of severe gastrointestinal symptoms, dehydration, electrolyte disturbances, and potentially life-threatening complications. Understanding proper dosing, recognizing overdose symptoms, and knowing when to seek medical attention are essential for safe use of this increasingly prescribed medication.
Quick Answer: While there is no established lethal dose of semaglutide in humans, taking excessive amounts can cause serious complications including severe gastrointestinal symptoms, dehydration, electrolyte disturbances, and hypoglycemia.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under the brand name Ozempic), chronic weight management in adults (as Wegovy), and weight management in pediatric patients aged 12 and older with obesity (also as Wegovy). The medication is available in both injectable (Ozempic, Wegovy) and oral (Rybelsus) formulations. Semaglutide works by mimicking the incretin hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways.
Approved dosing schedules differ by indication. For type 2 diabetes, semaglutide is initiated at 0.25 mg subcutaneously once weekly for four weeks, then increased to 0.5 mg weekly. The dose may be further escalated to 1 mg weekly and, if additional glycemic control is needed, to a maximum maintenance dose of 2 mg weekly. For chronic weight management, the titration schedule is more gradual, starting at 0.25 mg weekly and increasing monthly through specific steps (0.25 mg → 0.5 mg → 1.0 mg → 1.7 mg → 2.4 mg) to a target dose of 2.4 mg weekly. This stepwise approach minimizes gastrointestinal adverse effects, which are the most common tolerability issues with semaglutide.
The FDA-approved prescribing information does not specify a defined toxic dose or lethal threshold for semaglutide. However, exceeding recommended therapeutic doses increases the risk of adverse effects, particularly severe nausea, vomiting, and dehydration. Important safety considerations include a boxed warning regarding thyroid C-cell tumors observed in rodents (though the relevance to humans is unknown) and contraindications for patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Understanding the approved dosing parameters is essential for both clinicians and patients to ensure safe and effective use of this medication.
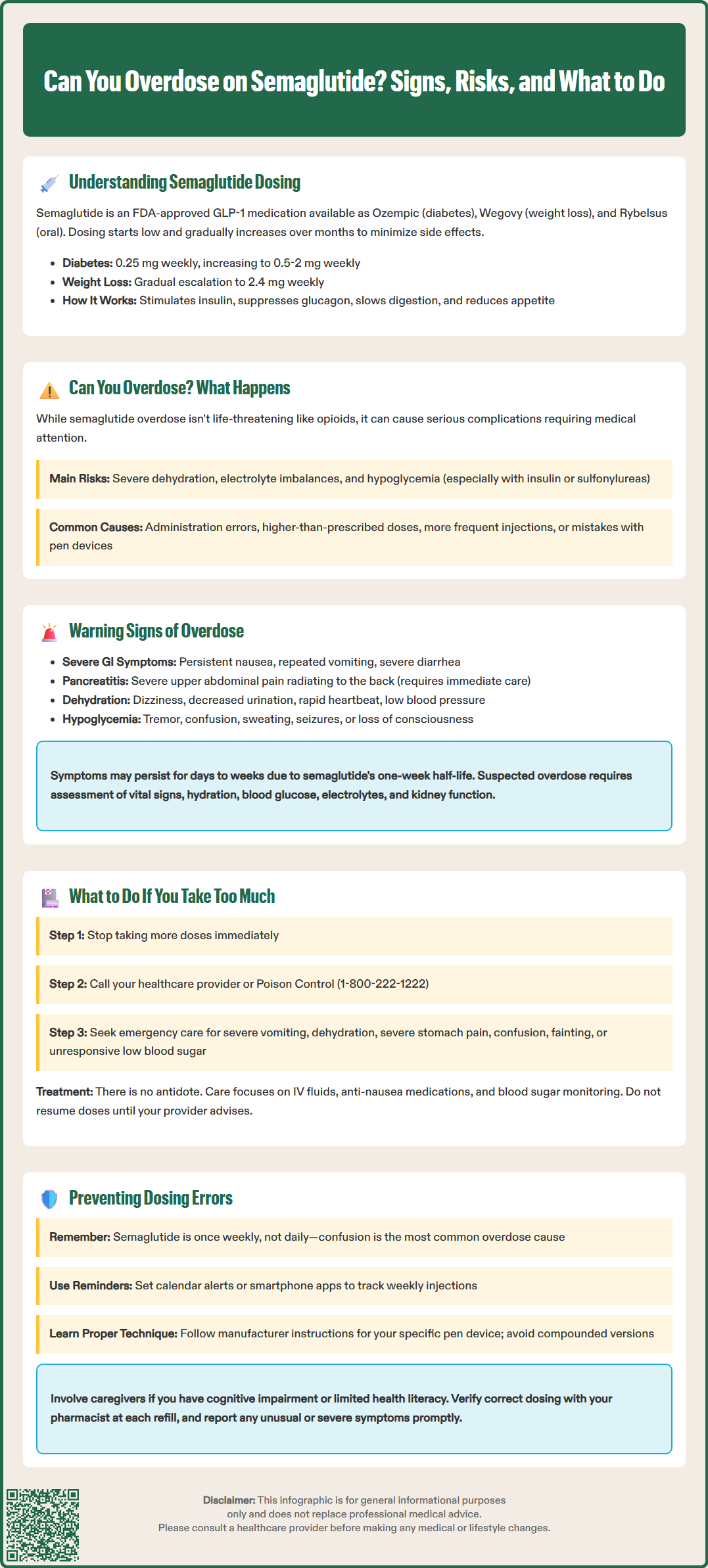
The concept of "overdose" with semaglutide differs from traditional overdose scenarios seen with medications like opioids or sedatives. There is no established lethal dose of semaglutide in humans, and the medication does not typically cause respiratory depression or loss of consciousness. However, severe complications such as profound dehydration, electrolyte disturbances, and hypoglycemia (especially when combined with insulin or sulfonylureas) can potentially become serious or life-threatening if not properly managed. The glucose-dependent mechanism of insulin secretion means that semaglutide carries a lower intrinsic risk of severe hypoglycemia when used as monotherapy, unlike insulin or sulfonylureas.
Post-marketing surveillance has documented cases of inadvertent overdosing, typically involving administration errors where patients received higher-than-prescribed doses or more frequent injections than intended. In these cases, the most commonly reported effects were gastrointestinal symptoms—primarily severe nausea, vomiting, and diarrhea—which can lead to dehydration and electrolyte disturbances if not managed appropriately. The FDA prescribing information for both Ozempic and Wegovy specifically notes these manifestations in the overdosage section.
The FDA has issued safety communications regarding compounded semaglutide products, which have been associated with adverse events including overdose due to improper compounding practices and dosing errors. Additionally, the Institute for Safe Medication Practices (ISMP) has reported on pen device-related dosing errors that can lead to unintended overdoses.
Animal toxicology studies have shown that semaglutide can cause thyroid C-cell tumors in rodents in a dose- and duration-dependent manner. The clinical relevance of these findings to humans remains unknown, and there is no evidence that acute overdose in humans increases thyroid cancer risk. The American Diabetes Association guidelines emphasize that while semaglutide has a favorable safety profile, appropriate dosing and patient education remain critical to minimize adverse events and optimize therapeutic outcomes.
Recognition of potential semaglutide overdose relies primarily on identifying an exaggerated pharmacological response rather than unique toxicological symptoms. The most prominent manifestations involve the gastrointestinal system, reflecting the medication's mechanism of delayed gastric emptying and effects on the gastrointestinal tract. Patients who have taken excessive doses typically experience severe and persistent nausea, often accompanied by repeated vomiting that may lead to inability to maintain oral hydration or nutrition.
Gastrointestinal symptoms may include severe abdominal pain or discomfort, which could indicate pancreatitis—a known adverse effect of GLP-1 receptor agonists that requires immediate medical attention. Patients should be evaluated for signs of acute pancreatitis, including persistent severe epigastric pain radiating to the back, elevated serum lipase or amylase levels (typically >3 times upper limit of normal), and characteristic imaging findings. Semaglutide should be discontinued if pancreatitis is suspected and should not be restarted if pancreatitis is confirmed.
Dehydration secondary to prolonged vomiting and diarrhea represents a significant clinical concern, potentially manifesting as dizziness, decreased urine output, dry mucous membranes, tachycardia, and orthostatic hypotension. Severe dehydration can lead to acute kidney injury, with signs including oliguria and rising serum creatinine. Severe constipation or ileus has also been reported with GLP-1 receptor agonists and may present with abdominal distension and absence of bowel movements.
Hypoglycemia, while uncommon with semaglutide monotherapy, becomes more likely in overdose situations, particularly in patients concurrently using insulin or sulfonylureas. Symptoms of hypoglycemia include tremor, palpitations, sweating, confusion, and in severe cases, loss of consciousness or seizures. Additional symptoms that may occur include headache, fatigue, and general malaise. It is important to note that the long half-life of semaglutide (approximately one week) means that symptoms may persist for several days to weeks following an overdose. Any patient presenting with suspected semaglutide overdose should undergo clinical assessment including vital signs, hydration status, blood glucose monitoring, and consideration of serum electrolytes and renal function.
If a patient realizes they have administered more semaglutide than prescribed, they should not take any additional doses and should contact their healthcare provider or poison control center (1-800-222-1222 in the United States) immediately for guidance. Patients experiencing severe or persistent vomiting, signs of dehydration, severe abdominal pain, confusion, fainting, or symptoms of hypoglycemia (blood glucose <70 mg/dL not responsive to oral carbohydrates) should seek immediate medical evaluation, either through their healthcare provider or an emergency department.
There is no specific antidote for semaglutide overdose. Semaglutide is highly protein-bound and not expected to be dialyzable. Management is entirely supportive and symptomatic, focusing on maintaining hydration, correcting electrolyte imbalances, and monitoring for complications. In the emergency department or clinical setting, treatment typically includes intravenous fluid resuscitation for dehydration, antiemetic medications to control nausea and vomiting (with careful consideration of electrolyte status when using medications like ondansetron, which may prolong QT interval in patients with hypokalemia or hypomagnesemia), and monitoring of vital signs and metabolic parameters. Blood glucose should be checked regularly, particularly in patients on concurrent diabetes medications, with appropriate treatment of hypoglycemia using oral glucose or intravenous dextrose as clinically indicated.
If pancreatitis is suspected, semaglutide should be discontinued immediately and appropriate diagnostic workup initiated. If pancreatitis is confirmed, semaglutide should not be restarted. For oral semaglutide (Rybelsus) overdose, management is similarly supportive, with consideration of the timing since ingestion.
Given semaglutide's long half-life, symptoms may persist for several days to weeks, and patients may require ongoing supportive care and monitoring during this period. Subsequent doses should be held until the patient has consulted with their healthcare provider, who will determine the appropriate timing for resuming the regular dosing schedule based on symptom resolution and clinical status. All overdose events should be reported to the patient's prescribing physician, and consideration should be given to reviewing injection technique, dosing instructions, and implementing strategies to prevent future errors.
Prevention of semaglutide overdose centers on comprehensive patient education, clear prescribing practices, and systematic approaches to medication administration. At the time of prescribing, clinicians should provide detailed verbal and written instructions regarding the correct dose, injection technique, and titration schedule. Patients should understand that semaglutide is administered once weekly, not daily, as confusion between daily and weekly dosing represents one of the most common errors leading to inadvertent overdose. Demonstrating proper use of the pre-filled pen device and having patients perform return demonstrations can identify potential technique issues before they result in dosing errors.
It's important to recognize that Ozempic and Wegovy use different pen devices—Ozempic utilizes multi-dose pens while Wegovy comes in single-dose pens—which can contribute to dosing errors. Patients should be trained using the manufacturer's Instructions for Use specific to their prescribed product. The FDA has issued safety communications regarding compounded semaglutide products, warning about adverse events related to improper compounding and dosing errors. Patients should be encouraged to use FDA-approved products rather than compounded alternatives.
Pharmacists play a critical role in overdose prevention through medication counseling and verification of appropriate dosing at each prescription fill. They should confirm that patients understand the difference between the various semaglutide formulations and strengths, as Ozempic, Wegovy, and Rybelsus have different dosing schedules and maximum doses. Implementing calendar-based reminders or smartphone applications can help patients track their weekly injections and avoid duplicate dosing.
Healthcare systems can implement additional safeguards, including electronic prescribing systems with built-in dose range checking, patient education materials in multiple formats (written, video, pictorial), and follow-up contact after initiation or dose escalation to assess tolerance and adherence. The Joint Commission's National Patient Safety Goals (NPSG.03.06.01) emphasize the importance of medication reconciliation at all transitions of care, which provides opportunities to identify and correct dosing errors before they result in adverse outcomes. For patients with cognitive impairment, visual deficits, or limited health literacy, involving caregivers in medication administration and education is essential. Finally, clinicians should maintain a low threshold for evaluating patients who report unusual or severe gastrointestinal symptoms, as these may indicate inadvertent overdosing or other complications requiring intervention. Clear communication channels between patients and healthcare providers facilitate early identification and management of dosing concerns, ultimately enhancing the safety profile of semaglutide therapy.
Taking a double dose typically causes severe gastrointestinal symptoms including nausea, vomiting, and diarrhea that may lead to dehydration. Contact your healthcare provider or poison control immediately, do not take your next scheduled dose, and seek emergency care if you experience persistent vomiting, severe abdominal pain, or signs of dehydration.
Due to semaglutide's one-week half-life, overdose symptoms may persist for several days to weeks. Patients may require ongoing supportive care and monitoring during this extended period until the medication is cleared from the body.
No, there is no specific antidote for semaglutide overdose. Treatment is entirely supportive and focuses on managing symptoms through intravenous hydration, antiemetic medications, electrolyte correction, and monitoring for complications such as pancreatitis or hypoglycemia.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.