LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
How many people take GLP-1 medications in the United States? GLP-1 receptor agonists represent one of the fastest-growing pharmaceutical classes, with millions of Americans now using these medications for type 2 diabetes and chronic weight management. Prescription rates have surged following FDA approvals of newer agents like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound). While precise current user numbers vary by data source, IQVIA tracking shows substantial year-over-year growth, though supply constraints and insurance coverage limitations continue to affect access. Understanding utilization patterns helps contextualize this transformative therapeutic class.
Quick Answer: Millions of Americans currently use GLP-1 receptor agonists, with prescription rates showing substantial year-over-year growth as one of the fastest-expanding pharmaceutical classes in the United States.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications that mimic the action of the naturally occurring GLP-1 hormone. These agents work by stimulating insulin secretion in a glucose-dependent manner, suppressing glucagon release, slowing gastric emptying, and promoting satiety through central nervous system pathways. The FDA has approved several GLP-1 medications including liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), semaglutide (Ozempic, Wegovy, Rybelsus), and tirzepatide (Mounjaro, Zepbound)—though tirzepatide is technically a dual GIP/GLP-1 receptor agonist. Exenatide products (Byetta, Bydureon) have been discontinued in the US market.
These medications are primarily prescribed for two distinct clinical indications. The first and original use is for type 2 diabetes management, where GLP-1 agonists help lower hemoglobin A1c levels by 1.0–2.0% on average, with the additional benefit of promoting modest weight loss rather than weight gain seen with some other diabetes medications. The second indication is chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity such as hypertension, dyslipidemia, or obstructive sleep apnea. Some formulations (Wegovy, Saxenda) are also FDA-approved for weight management in adolescents aged 12 years and older.
Certain GLP-1 formulations have demonstrated cardiovascular benefits in clinical trials, leading to specific FDA approvals: Victoza, Ozempic, and Trulicity are approved for reducing major adverse cardiovascular events in patients with type 2 diabetes and established cardiovascular disease, while Wegovy is approved for cardiovascular risk reduction in adults with established cardiovascular disease and either obesity or overweight. The American Diabetes Association (ADA) guidelines recommend GLP-1 receptor agonists as preferred agents for patients with type 2 diabetes and atherosclerotic cardiovascular disease, while SGLT2 inhibitors are preferred for heart failure and chronic kidney disease.
Important safety considerations include a boxed warning for medullary thyroid carcinoma risk, monitoring for pancreatitis (severe abdominal pain), gallbladder disease, and potential hypoglycemia when used with insulin or sulfonylureas. These medications are not recommended during pregnancy or breastfeeding, and caution is needed in patients with a history of pancreatitis.
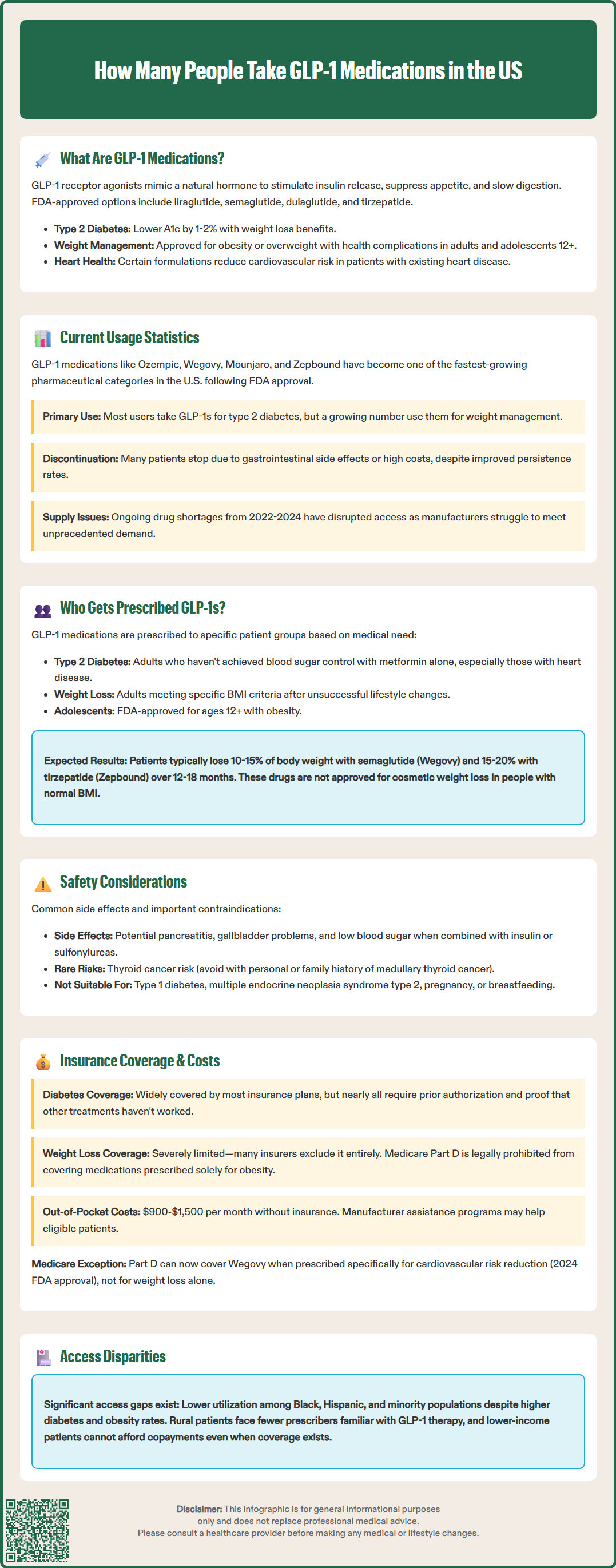
The use of GLP-1 medications has increased significantly in recent years, representing one of the fastest-growing pharmaceutical categories in the United States. According to IQVIA data, GLP-1 receptor agonist prescriptions have shown substantial growth, though precise current user numbers vary by source and definition (new prescriptions vs. continuing users).
Prescription trends show particularly rapid growth for newer agents. Semaglutide (Ozempic and Wegovy) and tirzepatide (Mounjaro and Zepbound) have experienced especially strong uptake following their FDA approvals. The GLP-1 market represents a major therapeutic class by revenue in the United States pharmaceutical landscape, with continued expansion expected.
Demographic data indicates that GLP-1 use spans diverse patient populations, though access remains uneven. The majority of current users have a primary diagnosis of type 2 diabetes, while a growing proportion are using these medications primarily for weight management. Treatment persistence has improved compared to earlier GLP-1 formulations, though discontinuation rates remain significant, often due to gastrointestinal side effects or cost concerns.
Supply constraints have periodically affected availability, with the FDA reporting shortages of several GLP-1 formulations throughout 2022-2024. The FDA Drug Shortages database has listed semaglutide and tirzepatide products at various times, reflecting manufacturing challenges in meeting unprecedented demand. These shortages have complicated access for both new and existing patients, requiring healthcare providers to consider FDA-approved alternatives. Manufacturing capacity is gradually expanding to meet demand, though supply-demand imbalances persist for some formulations.
GLP-1 receptor agonists are most commonly prescribed to adults with type 2 diabetes who have not achieved adequate glycemic control with metformin alone or who have specific comorbidities that make GLP-1 therapy particularly beneficial. According to ADA guidelines, these medications are preferred second-line agents for patients with established atherosclerotic cardiovascular disease. For patients with heart failure or chronic kidney disease, SGLT2 inhibitors are generally preferred first, with GLP-1 agonists considered when SGLT2 inhibitors are contraindicated or not tolerated. Patients with a hemoglobin A1c above target (typically >7.0% for most adults) despite lifestyle modifications and metformin therapy are prime candidates.
For weight management indications, GLP-1 medications are prescribed to adults meeting specific BMI criteria who have attempted lifestyle interventions without sufficient success. Clinical trial data from the STEP 1 and SURMOUNT-1 trials show that patients typically achieve 10–15% total body weight loss with semaglutide 2.4 mg weekly (Wegovy) and 15–20% with tirzepatide 10–15 mg weekly (Zepbound) over 12–18 months. These medications are not approved for cosmetic weight loss in individuals with normal BMI. Wegovy and Saxenda are also FDA-approved for adolescents aged 12 years and older with obesity.
Observational studies suggest differences in utilization patterns across demographic groups, though comprehensive national data is limited. The typical age range spans adults from 18-65+ years, with increasing use in younger adults for obesity treatment. Access disparities exist, with studies suggesting lower utilization rates among Black, Hispanic, and other minority populations despite higher rates of diabetes and obesity in these communities.
Certain patient populations require special consideration. GLP-1 medications are generally not recommended for patients with type 1 diabetes, those with a personal or family history of medullary thyroid carcinoma, or individuals with multiple endocrine neoplasia syndrome type 2. Most GLP-1 agonists (semaglutide, liraglutide, dulaglutide, tirzepatide) do not require dose adjustment for mild-to-moderate renal impairment, though caution is warranted in severe renal impairment. Patients with a history of pancreatitis should be monitored closely, and alternative therapies may be considered. These medications are not recommended during pregnancy or breastfeeding.
Insurance coverage for GLP-1 medications varies significantly depending on the indication, specific medication, and insurance plan type. For type 2 diabetes indications, most commercial insurance plans, Medicare Part D, and Medicaid programs provide coverage for GLP-1 receptor agonists, though prior authorization requirements are nearly universal. Insurers typically require documentation of inadequate glycemic control despite metformin therapy, contraindications to other agents, or presence of specific comorbidities that make GLP-1 therapy medically necessary.
Coverage for weight management indications is substantially more limited and represents a major barrier to access. Many commercial insurance plans exclude coverage for weight loss medications entirely, while others cover them only for patients meeting strict criteria. Medicare Part D plans are prohibited by federal law from covering medications prescribed solely for weight loss. However, following Wegovy's 2024 FDA approval for cardiovascular risk reduction, CMS issued guidance allowing Medicare Part D plans to cover Wegovy when prescribed for its cardiovascular indication in eligible patients. Some state Medicaid programs cover weight management medications, but many do not. This coverage gap has created significant out-of-pocket costs for patients seeking these medications for obesity treatment.
Out-of-pocket costs for GLP-1 medications are substantial without insurance coverage. Monthly costs typically range from $900 to $1,500 for brand-name products, making long-term therapy financially prohibitive for many patients. Manufacturer patient assistance programs and copay savings cards can reduce costs for eligible patients, though these programs have specific eligibility criteria and may not be available for government insurance beneficiaries due to federal anti-kickback regulations.
Access disparities extend beyond insurance coverage to include geographic and socioeconomic factors. Patients in rural areas may face limited access to prescribers familiar with GLP-1 therapy, while those in lower-income communities may lack insurance coverage or ability to afford copayments. Healthcare systems and policymakers are increasingly recognizing these access barriers, with ongoing discussions about expanding coverage criteria and addressing supply chain challenges. The evolving landscape of GLP-1 access will likely continue to shift as more long-term outcome data becomes available.
While comprehensive national data is limited, GLP-1 receptor agonists represent a major therapeutic class for type 2 diabetes, with the majority of current users having diabetes as their primary indication. ADA guidelines recommend GLP-1 agonists as preferred second-line agents for patients with established atherosclerotic cardiovascular disease.
The majority of current GLP-1 users have type 2 diabetes as their primary diagnosis, though a growing proportion are using these medications primarily for chronic weight management. Insurance coverage is substantially better for diabetes indications compared to weight management.
GLP-1 prescription growth reflects FDA approvals of newer, more effective agents like semaglutide and tirzepatide, demonstrated cardiovascular benefits in clinical trials, and expanded indications for both type 2 diabetes and chronic weight management. Supply constraints indicate demand has exceeded manufacturing capacity.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.