LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is an FDA-approved GLP-1 receptor agonist used for type 2 diabetes and chronic weight management. While this medication offers significant metabolic and cardiovascular benefits, clinical trials have documented modest increases in resting heart rate among some patients. Understanding why semaglutide increases heart rate, how common this effect is, and when to seek medical attention helps patients and clinicians make informed treatment decisions. This article examines the mechanisms behind heart rate changes, their clinical significance, and practical management strategies for patients taking semaglutide.
Quick Answer: Semaglutide increases heart rate through effects on the autonomic nervous system and GLP-1 receptors in the brain that regulate cardiac function, typically causing modest elevations of 2-4 beats per minute.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under brand names including Ozempic, Wegovy, and Rybelsus, semaglutide works by mimicking the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose metabolism and appetite regulation.
The medication exerts its therapeutic effects through multiple mechanisms. Semaglutide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. These actions collectively improve glycemic control in patients with type 2 diabetes. Additionally, semaglutide acts on appetite centers in the brain, particularly in the hypothalamus, leading to reduced caloric intake and significant weight loss in many patients.
Beyond its primary metabolic effects, semaglutide influences various physiological systems throughout the body. GLP-1 receptors are distributed not only in the pancreas and brain but also in the cardiovascular system, kidneys, and gastrointestinal tract. This widespread receptor distribution explains why semaglutide can produce effects beyond glucose control and weight reduction. Clinical trials have demonstrated cardiovascular benefits in certain patient populations, with Ozempic specifically indicated for reducing the risk of major adverse cardiovascular events in adults with type 2 diabetes and established cardiovascular disease, and Wegovy indicated for cardiovascular risk reduction in adults with established cardiovascular disease who have either obesity or overweight.
Understanding these broad systemic effects is essential when considering potential cardiovascular changes, including alterations in heart rate, that some patients may experience during semaglutide therapy. While the medication offers substantial benefits for metabolic health and cardiovascular risk reduction, awareness of its full range of physiological effects helps clinicians and patients make informed treatment decisions.
Mean increases in resting heart rate have been observed in randomized clinical trials of semaglutide and are documented in FDA prescribing information. While the precise mechanism behind this effect is not fully understood, several physiological pathways have been proposed based on clinical observations and pharmacological understanding of GLP-1 receptor agonists.
One leading hypothesis involves the autonomic nervous system. GLP-1 receptors are present in areas of the brain that regulate autonomic function, including heart rate control. Activation of these receptors may influence the balance between sympathetic (stimulatory) and parasympathetic (inhibitory) nervous system activity. Some research suggests that GLP-1 receptor agonists may increase sympathetic tone or decrease parasympathetic activity, which could lead to a modest elevation in resting heart rate.
Direct effects on the sinoatrial node or cardiac tissue may also play a role, as GLP-1 receptors have been identified in cardiac tissue. However, this mechanism requires further investigation to establish its clinical relevance in humans.
Secondary factors may contribute to heart rate changes in some patients. Semaglutide commonly causes gastrointestinal side effects including nausea, vomiting, and diarrhea, particularly during dose escalation. These symptoms can lead to decreased fluid intake or increased fluid losses, potentially resulting in relative volume depletion. The body may respond to reduced intravascular volume with a compensatory increase in heart rate to maintain adequate cardiac output and tissue perfusion.
It is important to note that clinical trials have reported modest mean increases in heart rate (typically 2-4 beats per minute), and not all patients experience this effect. The FDA prescribing information for Wegovy specifically includes a warning about heart rate increase and recommends monitoring heart rate at regular intervals, while Ozempic's label notes heart rate increases in the adverse reactions section.
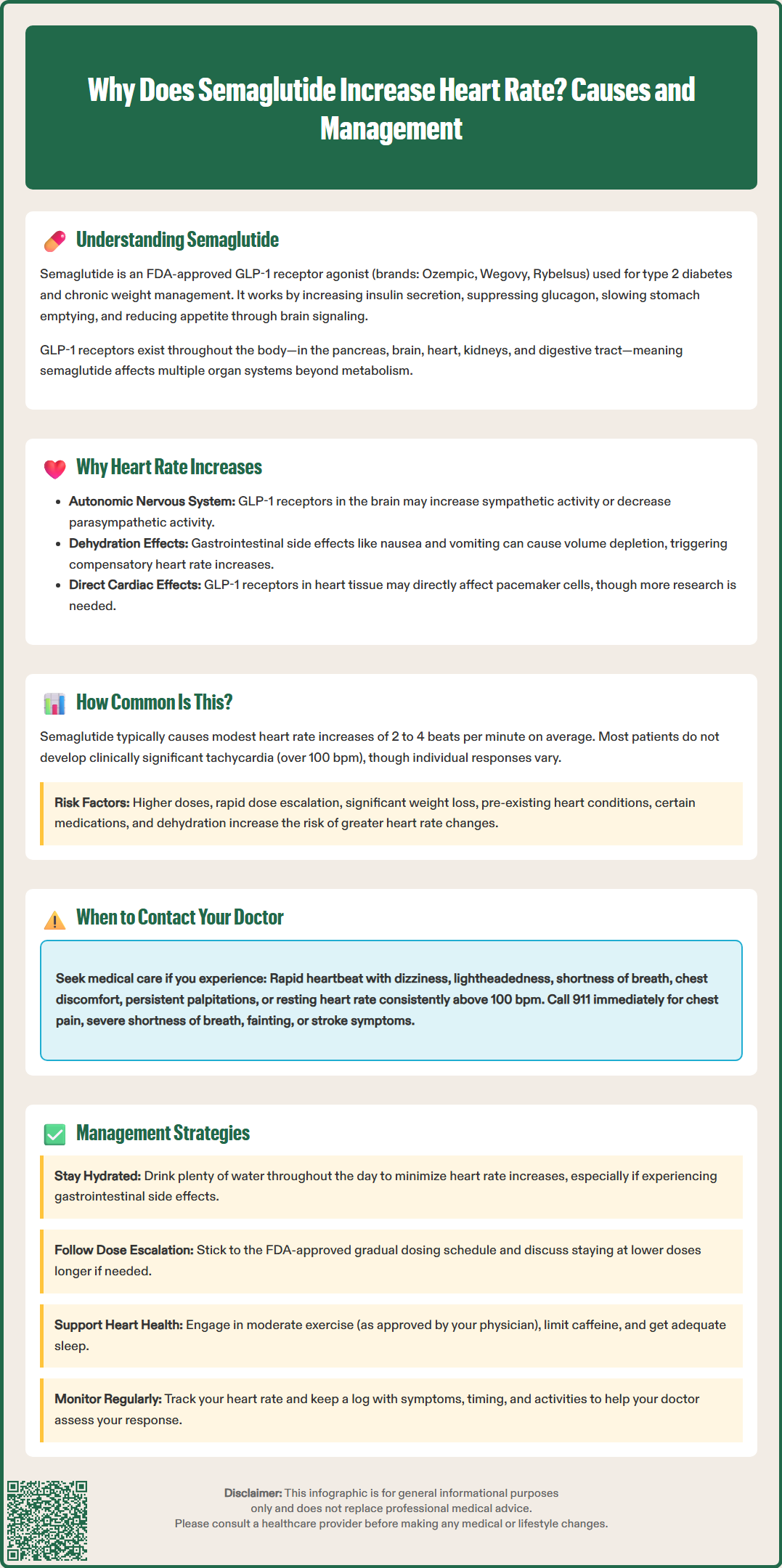
Based on data from major clinical trials and FDA prescribing information, heart rate increases with semaglutide are relatively common but typically modest in magnitude. The SUSTAIN clinical trial program, which evaluated semaglutide for type 2 diabetes, and the STEP trials for weight management provide the most comprehensive safety data available.
In the SUSTAIN trials, patients receiving semaglutide experienced mean increases in resting heart rate of approximately 2 to 4 beats per minute compared to baseline. These increases were generally observed within the first few months of treatment and tended to persist throughout the treatment period. Similar findings emerged from the STEP weight management trials, where heart rate elevations of comparable magnitude were documented. Importantly, these represent average changes across study populations; individual responses varied considerably.
The majority of patients do not experience clinically significant tachycardia (defined as heart rate exceeding 100 beats per minute at rest). However, a subset of individuals may experience more pronounced increases. Factors that may predispose patients to greater heart rate changes include:
Higher doses of semaglutide
Rapid dose escalation
Significant and rapid weight loss
Pre-existing cardiovascular conditions
Concurrent medications affecting heart rate
Dehydration or electrolyte imbalances
According to FDA prescribing information, palpitations have been reported in clinical trials, though precise incidence rates vary by product and study population. The FDA-approved prescribing information for Wegovy specifically includes a warning about heart rate increase and recommends monitoring heart rate at regular intervals, particularly when initiating treatment and increasing the dose.
Clinicians should be aware that heart rate changes may be more noticeable in patients who regularly monitor their cardiovascular parameters, such as those using fitness trackers or home blood pressure monitors with pulse measurement capabilities. However, consumer wearable devices may not provide the same accuracy as medical-grade monitoring equipment.
While modest heart rate increases are generally well-tolerated, certain symptoms and circumstances warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience any of the following:
Symptomatic tachycardia represents the most important indication for medical assessment. Contact your doctor if you experience a rapid or racing heartbeat accompanied by dizziness, lightheadedness, shortness of breath, chest discomfort, or near-syncope (feeling like you might faint). These symptoms may indicate that your heart rate elevation is clinically significant and requires evaluation.
Persistent palpitations that are bothersome or interfere with daily activities should be reported, even if not accompanied by other symptoms. While occasional awareness of your heartbeat is common and usually benign, persistent or frequent palpitations may warrant further investigation, including electrocardiography (ECG) to assess for arrhythmias.
Resting heart rate consistently exceeding 100 beats per minute should prompt medical consultation. If you regularly monitor your heart rate and notice sustained elevations above this threshold, particularly if this represents a significant change from your baseline, discuss this with your healthcare provider. They may recommend dose adjustment, additional cardiac evaluation, or assessment for contributing factors such as dehydration or medication interactions.
Patients with pre-existing cardiovascular conditions should maintain heightened awareness. If you have a history of arrhythmias, heart failure, coronary artery disease, or other cardiac conditions, report any new or worsening cardiovascular symptoms promptly. Your cardiologist and prescribing physician should coordinate care to ensure semaglutide remains appropriate for your situation.
Call 911 immediately for chest pain, severe shortness of breath, fainting (syncope), symptoms suggestive of stroke (such as sudden weakness, numbness, difficulty speaking, or vision changes), or sustained very rapid heart rate with symptoms. These require emergency medical attention regardless of their presumed cause. Do not attribute serious symptoms solely to medication without proper medical assessment.
For patients experiencing heart rate increases on semaglutide, several management strategies can help minimize symptoms and ensure safe continuation of therapy when clinically appropriate.
Adequate hydration represents an important intervention. Ensure consistent fluid intake throughout the day, particularly if experiencing gastrointestinal side effects. Hydration needs vary by individual, activity level, climate, and medical conditions. Patients with heart failure, kidney disease, or other conditions requiring fluid restrictions should follow their healthcare provider's specific guidance rather than general hydration recommendations. If nausea limits fluid intake, try small, frequent sips or electrolyte-containing beverages as tolerated.
Gradual dose escalation according to the FDA-approved titration schedule for your specific semaglutide product helps minimize side effects, including cardiovascular changes. Do not advance to higher doses more rapidly than recommended. If heart rate increases are problematic at a particular dose level, discuss with your physician whether maintaining that dose longer before escalation, or potentially remaining at a lower maintenance dose, might be appropriate. The goal is to balance therapeutic benefit with tolerability.
Lifestyle modifications can support cardiovascular health during treatment. Regular moderate-intensity exercise, as tolerated and approved by your physician, helps improve cardiovascular fitness and may help regulate heart rate over time. Avoid excessive caffeine intake, as this can independently increase heart rate and may compound any medication effects. Ensure adequate sleep, as sleep deprivation can affect autonomic nervous system function and heart rate regulation.
Medication review with your healthcare provider is essential. Certain medications can interact with semaglutide or independently affect heart rate. Your doctor should review all prescription medications, over-the-counter drugs, and supplements to identify potential contributors to tachycardia. In some cases, adjusting timing or dosing of other medications may help.
Regular monitoring provides reassurance and helps detect significant changes early. If you have concerns about heart rate, consider periodic monitoring using a reliable device. Keep a log of readings along with associated symptoms, timing relative to semaglutide doses, and any relevant activities or dietary factors. This information can help your healthcare provider assess patterns and determine whether intervention is needed. For accurate measurements, consider having your heart rate checked at medical facilities if you're concerned about the reliability of home devices.
If heart rate increases remain problematic despite these measures, your physician may consider additional evaluation (such as ECG, electrolyte testing, or thyroid function tests), dose reduction, temporary treatment interruption, or discontinuation if clinically indicated. The decision should weigh the cardiovascular concerns against the metabolic benefits of continued therapy, taking into account your individual risk profile and treatment goals.
Clinical trials show semaglutide causes mean increases in resting heart rate of approximately 2-4 beats per minute compared to baseline. Individual responses vary, and most patients do not experience clinically significant tachycardia.
Do not stop semaglutide without consulting your healthcare provider. Modest heart rate increases are generally well-tolerated, but contact your doctor if you experience symptomatic tachycardia, persistent palpitations, or resting heart rate consistently exceeding 100 beats per minute.
Heart rate increases typically occur within the first few months of treatment and tend to persist throughout therapy. However, individual responses vary, and management strategies including adequate hydration and gradual dose escalation may help minimize this effect.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.