LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Staying properly hydrated while taking GLP-1 medications like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) is essential for managing side effects and optimizing treatment outcomes. These medications slow gastric emptying and reduce appetite, which can inadvertently decrease fluid intake while increasing the risk of dehydration through gastrointestinal symptoms like nausea, vomiting, and diarrhea. Understanding how much water you need daily on GLP-1 therapy helps prevent complications, minimize discomfort, and support your weight management or diabetes goals. This guide provides evidence-based hydration recommendations, practical strategies for meeting fluid needs, and guidance on recognizing when dehydration requires medical attention.
Quick Answer: Patients on GLP-1 medications should aim for approximately 91-125 ounces of total daily fluid intake (2.7-3.7 liters), with adjustments based on individual factors like body weight, activity level, and gastrointestinal symptoms.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—along with tirzepatide (Mounjaro, Zepbound), a dual GIP/GLP-1 receptor agonist, have transformed the management of type 2 diabetes and obesity. These medications work by mimicking natural incretin hormones, which slow gastric emptying, enhance insulin secretion, suppress glucagon release, and reduce appetite through central nervous system pathways. While these mechanisms contribute to improved glycemic control and weight loss, they also create specific hydration challenges that patients and clinicians must address proactively.
The delayed gastric emptying characteristic of these therapies frequently causes gastrointestinal adverse effects, particularly nausea, vomiting, and diarrhea. These symptoms can affect up to 30-45% of patients during dose escalation (varying by medication and dose) and can lead to significant fluid losses if not managed appropriately. Additionally, the appetite suppression that makes these medications effective for weight management may inadvertently reduce overall fluid intake, as patients often consume less food and beverages throughout the day.
Maintaining adequate hydration becomes particularly important because dehydration can exacerbate common side effects, creating a problematic cycle. Insufficient fluid intake may worsen constipation—another frequent adverse effect—and can intensify feelings of nausea and fatigue. For patients with diabetes, dehydration poses additional risks by potentially affecting kidney function and blood glucose stability. In fact, FDA labels for these medications include warnings about acute kidney injury risk, particularly when dehydration occurs from severe gastrointestinal adverse events. Understanding these interconnected factors enables patients to optimize their treatment outcomes while minimizing discomfort.
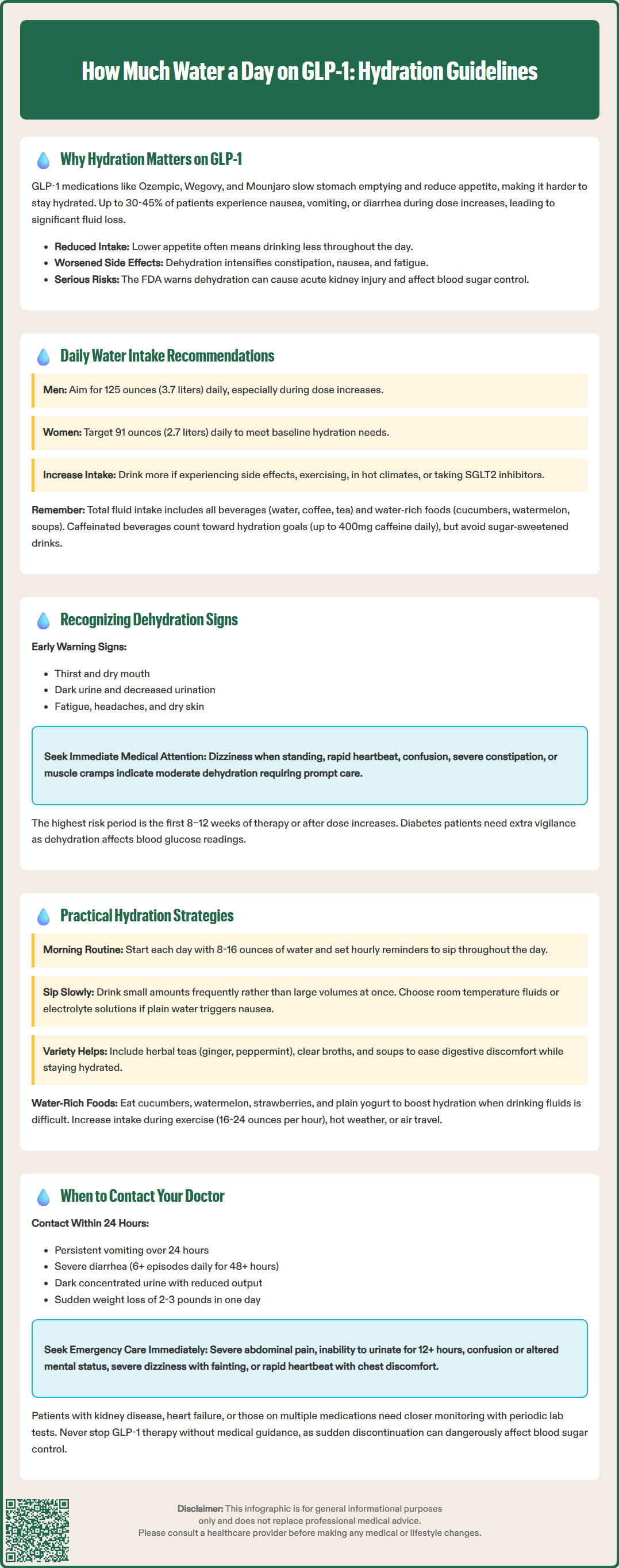
While there is no official FDA-mandated water intake specifically for GLP-1 medications, clinical experience and general hydration guidelines provide a practical framework for patients. The National Academy of Medicine recommends a total water intake (from all beverages and food) of approximately 125 ounces (3.7 liters) daily for men and 91 ounces (2.7 liters) for women under normal conditions. About 80% of this typically comes from beverages, with the remainder from food.
For patients on GLP-1 or GIP/GLP-1 therapy, many endocrinologists and diabetes educators suggest targeting these recommended adequate intake levels, with particular attention to consistent hydration during dose escalation periods when gastrointestinal symptoms are most pronounced.
A practical approach involves monitoring your fluid intake to ensure you're meeting these guidelines, with adjustments based on individual factors. Patients experiencing active nausea, vomiting, or diarrhea should increase intake to compensate for fluid losses. Those engaging in physical activity, living in hot climates, or experiencing increased urination (common with hyperglycemia or SGLT2 inhibitor medications) require additional hydration beyond baseline recommendations. Body weight influences needs—larger individuals generally require more fluid, though personalized targets should be developed with healthcare providers.
It's important to recognize that total fluid intake includes water from all sources: plain water, coffee, tea, other beverages, and water-rich foods like cucumbers, watermelon, and soups. Contrary to common belief, caffeinated beverages do generally count toward hydration goals, though moderation is advised (FDA considers up to 400mg caffeine daily generally safe for most adults). However, sugar-sweetened beverages should be limited due to their glycemic impact. Patients should work with their healthcare team to establish individualized hydration targets, particularly those with heart failure, kidney disease, or other conditions requiring fluid restriction. Regular monitoring and adjustment based on symptoms, urine color, and clinical parameters ensure optimal hydration throughout treatment.
Recognizing dehydration early allows for prompt intervention and prevents progression to more serious complications. Patients on GLP-1 medications should monitor for both mild and moderate dehydration symptoms, as the gradual onset may be subtle, particularly when appetite suppression affects overall fluid consumption.
Early signs of mild dehydration include:
Thirst and dry mouth
Dark yellow or amber-colored urine—healthy hydration typically produces pale yellow urine
Decreased urination frequency or volume
Fatigue and reduced energy levels—often attributed to medication but may reflect dehydration
Headaches—particularly if new or worsening since starting therapy
Dry skin and lips
More concerning signs of moderate dehydration warrant prompt medical attention:
Dizziness or lightheadedness, especially when standing (orthostatic symptoms)
Rapid heartbeat or palpitations
Confusion or difficulty concentrating
Dry mucous membranes (mouth, eyes)
Severe constipation unresponsive to usual measures
Muscle cramps or weakness
Patients with diabetes should be particularly vigilant, as dehydration can affect blood glucose readings and may contribute to hyperglycemic hyperosmolar state (HHS) in type 2 diabetes. Those taking SGLT2 inhibitors alongside GLP-1/GIP medications face additional risks, including increased urination and potential for euglycemic diabetic ketoacidosis if severely dehydrated.
Individuals taking diuretics, ACE inhibitors, or other medications affecting fluid balance face increased dehydration risk. The combination of reduced oral intake from appetite suppression and fluid losses from gastrointestinal symptoms creates a vulnerable period, especially during the first 8–12 weeks of therapy or following dose increases. Keeping a simple hydration log or using smartphone reminders can help patients track intake and identify patterns before dehydration becomes clinically significant.
Maintaining adequate hydration while managing GLP-1 side effects requires strategic planning and practical techniques that accommodate reduced appetite and potential nausea. The following evidence-informed strategies can help patients meet their fluid goals consistently.
Establish a structured hydration routine:
Start each day with 8–16 ounces of water upon waking, before breakfast or morning medications
Set hourly reminders on your phone or smartwatch to take several sips throughout the day
Use a marked water bottle (with time-based goals) to visualize progress toward daily targets
Drink water before, during, and after meals—even if eating less, maintain the hydration habit
Adapt fluid intake to minimize nausea:
Sip slowly and frequently rather than consuming large volumes at once, which may trigger nausea
Choose room temperature or slightly cool water—very cold beverages may worsen gastric discomfort
Try electrolyte solutions (sugar-free options) if plain water feels unappealing or causes nausea
Incorporate herbal teas (ginger, peppermint) that provide hydration while potentially easing digestive symptoms
Consume clear broths or soups, which offer both hydration and electrolytes with minimal nausea risk
Increase water-rich food consumption:
Cucumbers, celery, lettuce, zucchini (>95% water content)
Watermelon, strawberries, cantaloupe, oranges (85–92% water)
Plain yogurt, cottage cheese (provides protein plus hydration)
Sugar-free gelatin or popsicles for those struggling with nausea
Monitor and adjust based on activity and environment:
During exercise, drink according to thirst and conditions—approximately 16-24 ounces per hour of moderate activity in temperate conditions, adjusting for heat and intensity
Increase intake during hot weather or in heated indoor environments
Compensate for air travel, which can accelerate dehydration
Caffeinated beverages can contribute to your fluid intake, though moderation is advised (limit to 400mg caffeine daily, roughly 3-5 cups of coffee). Minimize alcohol consumption, as it can contribute to dehydration. Avoid or limit sugar-sweetened beverages, particularly if you have diabetes. Working with a registered dietitian familiar with GLP-1 therapy can provide personalized strategies that align with individual tolerance, preferences, and medical conditions.
While most hydration challenges on GLP-1 therapy can be managed with increased fluid intake and dietary modifications, certain situations require prompt medical evaluation to prevent serious complications or identify underlying issues requiring treatment adjustment.
Contact your healthcare provider within 24 hours if you experience:
Persistent vomiting (more than 24 hours) preventing adequate fluid intake
Severe diarrhea (more than 6 episodes daily) lasting beyond 48 hours
Inability to keep down fluids despite anti-nausea measures
Weight loss exceeding 2–3 pounds in 24 hours (likely fluid loss)
Markedly reduced urine output with dark, concentrated urine
New or worsening dizziness affecting daily activities or causing falls
Blood glucose readings consistently above target despite usual management
Seek immediate medical attention (emergency department or call 911) for:
Severe, persistent abdominal pain (may indicate pancreatitis or gallbladder disease, which are labeled risks of GLP-1 medications requiring immediate evaluation and drug discontinuation)
Severe dizziness or fainting episodes
Rapid or irregular heartbeat with chest discomfort
Confusion, disorientation, or altered mental status
Inability to urinate for 12+ hours
Signs of acute kidney injury (decreased urine output, swelling, severe fatigue)
Symptoms of hyperglycemic emergencies in diabetes patients (excessive thirst, frequent urination, fatigue, fruity breath)
Patients with pre-existing kidney disease, heart failure, or those taking multiple medications affecting fluid balance should maintain closer communication with their healthcare team. These individuals may require more frequent monitoring, including periodic laboratory assessment of kidney function (serum creatinine, estimated glomerular filtration rate) and electrolytes, particularly during dose escalation.
If gastrointestinal symptoms persist despite adequate hydration and supportive measures, your provider may consider dose reduction, temporary treatment interruption, or prescribing anti-emetic medications such as ondansetron or metoclopramide. In some cases, switching to a different medication with a different pharmacokinetic profile may improve tolerability. Never discontinue therapy without medical guidance, as abrupt cessation can affect glycemic control in diabetes patients. Open communication with your healthcare team ensures safe, effective treatment while maintaining optimal hydration status throughout your therapeutic journey.
Yes, caffeinated beverages like coffee and tea count toward your daily fluid intake and are generally safe in moderation (up to 400mg caffeine daily). However, avoid adding excessive sugar, and monitor how caffeine affects any nausea or gastrointestinal symptoms you may experience.
Try sipping small amounts frequently rather than drinking large volumes at once, choose room temperature fluids instead of very cold water, and consider electrolyte solutions, herbal teas (ginger or peppermint), clear broths, or water-rich foods like watermelon. If nausea persists despite these strategies, contact your healthcare provider about anti-nausea medications.
Yes, SGLT2 inhibitors increase urination and fluid loss, so you'll likely need additional hydration beyond standard recommendations when combining these medications with GLP-1 therapy. Discuss individualized fluid targets with your healthcare provider, especially during hot weather or physical activity.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.