LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
GLP-1 receptor agonists like semaglutide and tirzepatide have gained attention for weight management, prompting questions about their role in lymphedema treatment. Lymphedema, a chronic condition causing progressive limb swelling from impaired lymphatic drainage, affects approximately 1-2 million Americans and remains challenging to manage. While no FDA-approved indication exists for GLP-1 medications in lymphedema, emerging interest focuses on whether weight loss achieved through these agents might benefit obese patients with this condition. This article examines current evidence, potential mechanisms, and the role of GLP-1 therapy within comprehensive lymphedema management.
Quick Answer: GLP-1 receptor agonists are not FDA-approved for lymphedema and lack direct evidence for treating lymphatic dysfunction, though they may indirectly benefit obese patients with lymphedema through significant weight loss.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Lymphedema is a chronic condition characterized by abnormal accumulation of protein-rich fluid in the interstitial tissues, resulting in progressive swelling, typically affecting the extremities. This disorder arises from impaired lymphatic drainage due to either congenital abnormalities (primary lymphedema) or acquired damage to the lymphatic system (secondary lymphedema). In the United States, secondary lymphedema most commonly develops following cancer treatment, particularly after lymph node dissection or radiation therapy for breast cancer, though it can also result from trauma, infection, or venous insufficiency.
The pathophysiology involves mechanical insufficiency of the lymphatic system, leading to fluid stasis, chronic inflammation, adipose tissue deposition, and progressive fibrosis. Patients experience limb heaviness, reduced mobility, recurrent infections (cellulitis), and significant psychosocial burden. The condition affects approximately 1-2 million Americans, with prevalence increasing among cancer survivors as treatment outcomes improve.
Treatment challenges are substantial and multifaceted. Current management relies primarily on conservative measures including complete decongestive therapy (CDT), which combines manual lymphatic drainage, compression bandaging, therapeutic exercise, and skin care. However, CDT requires intensive specialist input from certified lymphedema therapists, patient compliance is often suboptimal due to the demanding regimen, and long-term outcomes remain variable. Surgical options exist for select cases but carry significant risks and costs.
Importantly, sudden onset of unilateral swelling, especially with pain, warmth, or redness, requires urgent medical evaluation to rule out deep vein thrombosis or acute infection. Diuretics are generally ineffective for lymphedema unless another indication exists. The chronic, progressive nature of lymphedema and its resistance to conventional treatment has prompted investigation into novel therapeutic approaches, including metabolic interventions that may address underlying pathophysiological mechanisms.
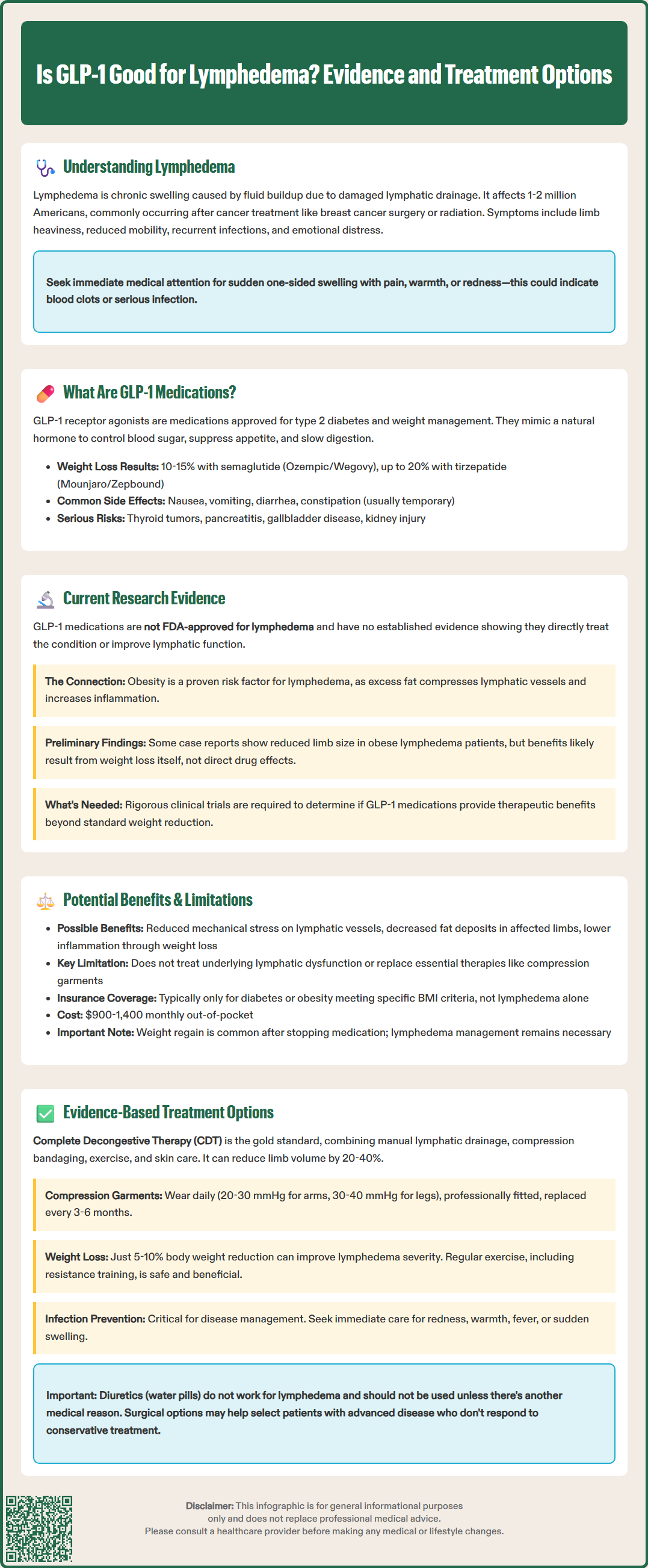
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management, with select agents subsequently approved for chronic weight management. These medications include semaglutide (Ozempic for diabetes, Wegovy for obesity), liraglutide (Victoza for diabetes, Saxenda for obesity), dulaglutide (Trulicity, approved only for diabetes), and tirzepatide (Mounjaro for diabetes, Zepbound for obesity), which is a dual GLP-1/GIP receptor agonist. The FDA has approved specific formulations for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with weight-related comorbidities.
The mechanism of action centers on mimicking endogenous GLP-1, an incretin hormone secreted by intestinal L-cells in response to nutrient intake. GLP-1 receptor agonists bind to GLP-1 receptors expressed throughout the body, including pancreatic beta cells, the central nervous system, cardiovascular tissue, and adipose tissue. Their primary effects include:
Glucose-dependent insulin secretion from pancreatic beta cells
Suppression of glucagon release from alpha cells
Delayed gastric emptying, promoting satiety
Central appetite suppression via hypothalamic pathways
Reduced energy intake through decreased appetite and earlier satiety
These medications produce substantial weight loss—typically 10-15% of body weight with semaglutide and up to 20% with tirzepatide—primarily through reduced caloric intake. Common adverse effects include gastrointestinal symptoms (nausea, vomiting, diarrhea, constipation), which are usually transient and dose-dependent.
There is currently no established evidence base demonstrating that GLP-1 receptor agonists directly treat lymphedema or improve lymphatic function. No randomized controlled trials have specifically evaluated GLP-1 medications as a primary intervention for lymphedema management, and these agents are not approved by the FDA for lymphedema treatment. The scientific literature lacks direct mechanistic studies examining GLP-1 effects on lymphatic vessel function, lymphangiogenesis, or lymphatic pumping capacity.
However, emerging research has identified potential indirect connections worth noting. Obesity is a well-established risk factor for lymphedema development and progression, particularly in cancer survivors, as documented in NCCN Survivorship Guidelines and National Lymphedema Network position papers. Excess adipose tissue mechanically compresses lymphatic vessels, promotes chronic low-grade inflammation, and impairs lymphatic transport capacity. Observational studies have suggested that weight reduction can improve lymphedema symptoms and reduce limb volume in obese patients with the condition, though the quality of evidence remains limited.
Preliminary observational data and case reports have suggested that some patients with both obesity and lymphedema experience symptomatic improvement when treated with GLP-1 agonists for weight management. These reports describe reduced limb circumference, decreased heaviness, and improved mobility. However, such observations cannot establish causation and likely reflect the natural benefits of weight loss through any means rather than a specific drug effect. Additionally, GLP-1 receptors have been identified in various tissues involved in inflammation and immune regulation, raising questions about potential anti-inflammatory effects that could theoretically benefit the chronic inflammatory component of lymphedema. Rigorous clinical trials are needed to determine whether any observed benefits represent genuine therapeutic effects beyond weight reduction alone.
The potential benefits of GLP-1 receptor agonists for lymphedema patients are primarily indirect and related to weight management rather than direct lymphatic effects. For obese individuals with lymphedema, significant weight loss achieved through GLP-1 therapy may offer several advantages:
Reduced mechanical load on compromised lymphatic vessels
Decreased adipose tissue deposition in affected limbs
Improved mobility and exercise tolerance, facilitating physical therapy
Reduced systemic inflammation associated with obesity
Enhanced quality of life through combined weight loss and symptom improvement
Clinical guidelines from organizations such as the National Lymphedema Network and NCCN Survivorship Guidelines emphasize weight management as an important component of comprehensive lymphedema care for overweight patients. In this context, GLP-1 agonists represent a potentially valuable tool within a multimodal treatment approach, particularly for patients who have not achieved adequate weight loss through lifestyle modification alone.
However, significant limitations must be acknowledged. There is no evidence that GLP-1 medications address the fundamental lymphatic dysfunction underlying lymphedema or promote lymphatic regeneration. These agents cannot replace established therapies such as compression therapy and manual lymphatic drainage. The medications carry risks including gastrointestinal side effects that may limit tolerability, potential pancreatitis, and substantial cost (often $900-1,400 monthly without insurance coverage). Insurance authorization for GLP-1 agonists typically requires meeting specific criteria for diabetes or obesity (BMI thresholds and comorbidities), not lymphedema diagnosis alone.
Furthermore, weight loss alone does not cure lymphedema, and patients require continued conservative management regardless of weight reduction. Clinical trial data (STEP-4, SURMOUNT) demonstrate that treatment discontinuation typically results in substantial weight regain. Patients with normal BMI and lymphedema would not be appropriate candidates for these medications, as the risk-benefit profile would be unfavorable without obesity-related indications.
Current evidence-based management of lymphedema centers on conservative therapies with proven efficacy. The gold standard remains complete decongestive therapy (CDT), a comprehensive approach consisting of two phases. The intensive phase involves daily manual lymphatic drainage performed by certified lymphedema therapists (CLT), multilayer compression bandaging, remedial exercises, and meticulous skin care. The maintenance phase transitions to self-management with compression garments, continued exercise, and ongoing skin protection. Systematic reviews demonstrate that CDT typically reduces limb volume by 20-40%, with results varying by disease stage and affected limb.
Compression therapy is the cornerstone of long-term management. Graduated compression garments (20-30 mmHg for upper extremities or 30-40 mmHg for lower extremities) maintain volume reduction achieved through CDT and prevent progression. Garments should be professionally fitted, replaced every 3-6 months, and worn daily. Pneumatic compression devices provide adjunctive home-based treatment, though they should complement rather than replace manual techniques and compression garments.
Weight management represents an evidence-based intervention for overweight patients. Studies demonstrate that even modest weight loss (5-10% of body weight) can reduce lymphedema severity and improve symptoms. Dietary counseling and structured exercise programs should be incorporated into comprehensive care plans. The American Cancer Society and National Lymphedema Network recommend regular physical activity, including resistance training, which was previously discouraged but is now recognized as safe and beneficial.
Surgical interventions may be considered for select patients with advanced disease unresponsive to conservative management. Options include lymphovenous anastomosis, vascularized lymph node transfer, and suction-assisted protein lipectomy. These procedures require specialized expertise and careful patient selection.
Infection prevention is critical, as cellulitis occurs frequently in lymphedematous limbs and accelerates disease progression. Patients should receive education on:
Meticulous skin hygiene and moisturization
Prompt treatment of minor wounds
Recognition of early infection signs (erythema, warmth, fever)
Immediate medical attention for suspected cellulitis
Some patients with recurrent cellulitis (typically ≥3-4 episodes annually) may benefit from prophylactic antibiotics according to Infectious Diseases Society of America guidelines. Patients should seek urgent medical care for sudden onset of swelling, pain, or redness to rule out deep vein thrombosis or acute infection. Referral to certified lymphedema therapists (CLT-LANA) and specialized lymphedema clinics is appropriate for complex cases, inadequate response to initial therapy, or when surgical evaluation is warranted.
No, GLP-1 receptor agonists are not FDA-approved for lymphedema and have no established evidence demonstrating direct treatment of lymphatic dysfunction. Any potential benefits appear indirect, primarily through weight loss in obese patients.
Complete decongestive therapy (CDT) remains the evidence-based gold standard, combining manual lymphatic drainage by certified therapists, compression bandaging, therapeutic exercise, and meticulous skin care. Compression garments are essential for long-term maintenance.
GLP-1 medications may be appropriate if you meet FDA criteria for obesity treatment (BMI ≥30 or ≥27 with comorbidities), as weight loss can reduce mechanical stress on lymphatic vessels. However, these medications should complement, not replace, established lymphedema therapies like compression and manual drainage.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.