LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many patients taking tirzepatide for type 2 diabetes or weight management wonder how to get energy while on tirzepatide, especially during the initial treatment phase. Tirzepatide (Mounjaro for diabetes, Zepbound for weight management) is a dual GIP and GLP-1 receptor agonist that can affect energy levels through reduced appetite, slower gastric emptying, and caloric restriction. While mild fatigue may occur as your body adjusts, strategic nutritional planning, proper hydration, adequate sleep, and appropriate physical activity can help maintain energy throughout treatment. Understanding why fatigue occurs and implementing evidence-based strategies enables most patients to manage energy effectively while achieving their therapeutic goals.
Quick Answer: Energy levels on tirzepatide can be maintained through adequate protein intake (1.0-1.6 g/kg daily), proper hydration, consistent sleep schedules, and gradual physical activity while monitoring for symptoms requiring medical evaluation.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). While fatigue is not among the most common adverse effects, some patients report experiencing low energy during treatment, particularly during the initial adjustment period.
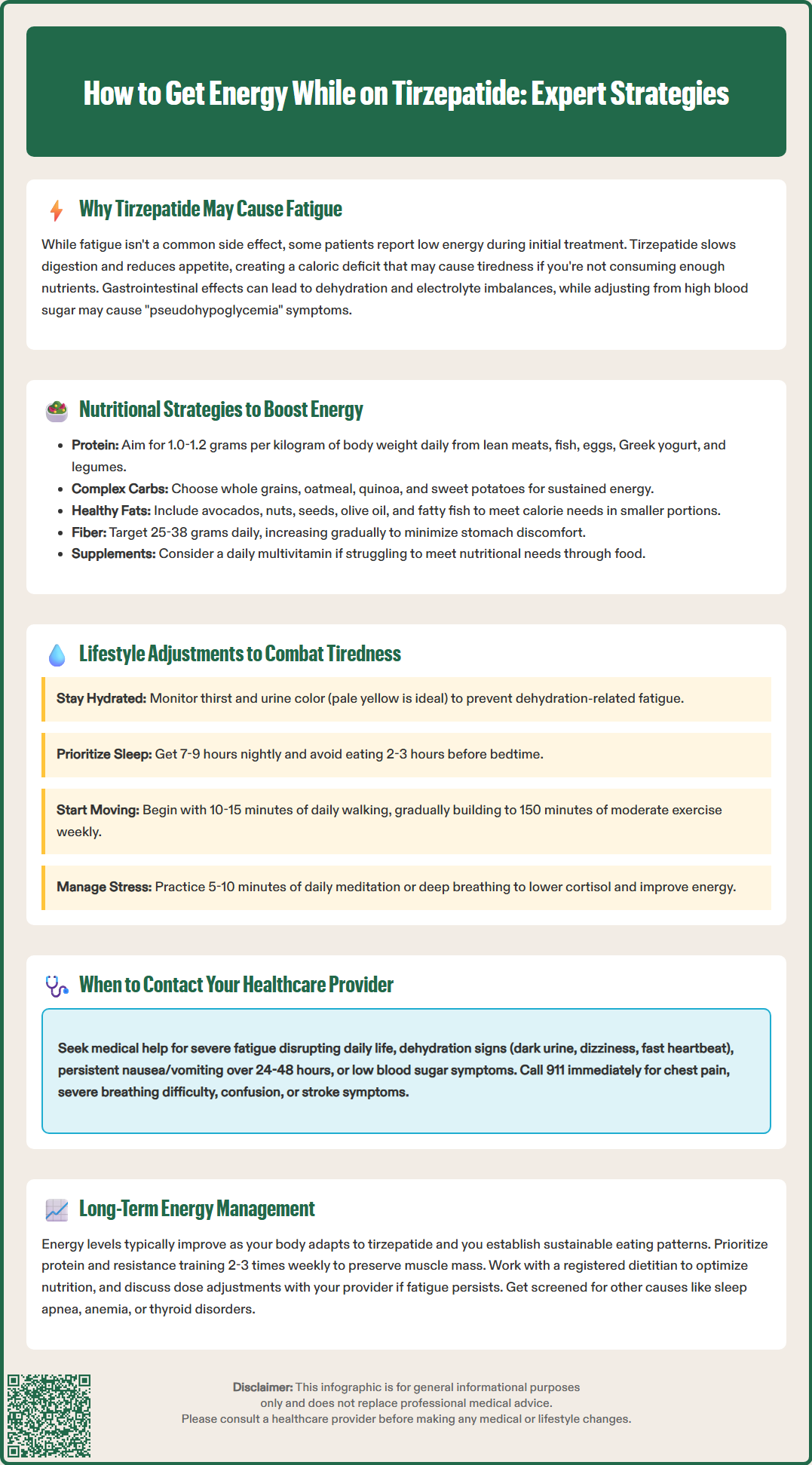
Several mechanisms may potentially contribute to reduced energy levels on tirzepatide. The medication slows gastric emptying, most pronounced after initial doses and diminishing over time, which can lead to decreased caloric intake as patients experience prolonged satiety and reduced appetite. This caloric deficit, while beneficial for weight loss, may result in insufficient energy intake if patients are not consuming adequate nutrients. Additionally, gastrointestinal side effects—including nausea, vomiting, and diarrhea—can lead to dehydration and electrolyte imbalances that may impact energy levels.
The pharmacological action of tirzepatide on glucose regulation may also play a role. By enhancing insulin secretion in a glucose-dependent manner and suppressing glucagon release, the medication helps normalize blood glucose levels. Patients transitioning from chronically elevated glucose levels may experience symptoms similar to hypoglycemia (pseudohypoglycemia) as their bodies adjust to lower glucose ranges, which can manifest as fatigue, even when glucose levels remain within normal limits.
It's important to note that there is no established direct link between tirzepatide and chronic fatigue syndrome or persistent energy depletion. Many patients find that energy levels improve as their bodies adapt to the medication, though the timeline varies between individuals.
Maintaining adequate nutrition while on tirzepatide requires deliberate planning, as the medication's appetite-suppressing effects can make it challenging to consume sufficient calories and nutrients. Prioritizing nutrient-dense foods is essential to maximize energy intake within a reduced appetite window.
Protein intake should be a primary focus, with a target of 1.0-1.2 grams per kilogram of body weight daily for most adults, and potentially higher (1.2-1.6 g/kg) for older adults or those engaging in regular physical activity. High-quality protein sources—including lean poultry, fish, eggs, Greek yogurt, and legumes—help preserve lean muscle mass during weight loss and provide sustained energy. Distributing protein across meals rather than concentrating it in one sitting may improve satiety and support muscle protein synthesis.
Carbohydrate intake should be individualized based on blood glucose goals and monitoring results. Complex carbohydrates such as whole grains, oatmeal, quinoa, sweet potatoes, and brown rice offer sustained energy release. Patients with diabetes should work with their healthcare providers to determine appropriate carbohydrate targets and distribution throughout the day.
Healthy fats are calorie-dense and can help patients meet energy needs in smaller volumes. Avocados, nuts, seeds, olive oil, and fatty fish provide essential fatty acids and fat-soluble vitamins while supporting satiety. Including small amounts of healthy fats with meals can improve nutrient absorption and provide concentrated energy.
Fiber intake of 25-38 grams daily supports digestive health and helps regulate glucose absorption. Gradually increasing fiber intake can minimize GI discomfort.
Micronutrient considerations are equally important. B vitamins, iron, magnesium, and vitamin D all play crucial roles in energy metabolism. A daily multivitamin may be reasonable for patients consistently unable to meet nutritional needs through food alone, though megadoses should be avoided. Patients taking metformin should be particularly mindful of vitamin B12 status.
Smaller, more frequent meals may help some patients consume adequate nutrition despite reduced appetite. A registered dietitian can provide personalized nutrition guidance based on individual health status, medications, and goals.
Beyond nutrition, several lifestyle modifications can significantly improve energy levels while taking tirzepatide. Hydration is important, as the medication's gastrointestinal effects can lead to fluid losses. Most adults should aim for adequate fluid intake based on thirst, urine color (pale yellow indicates good hydration), and activity level. Patients with heart failure, kidney disease, or those on fluid restrictions should follow their healthcare provider's specific recommendations regarding fluid intake. Dehydration can cause fatigue, headaches, and difficulty concentrating.
Sleep hygiene deserves careful attention during tirzepatide treatment. Establishing a consistent sleep schedule with 7-9 hours of quality sleep per night supports metabolic health and energy regulation. Patients should avoid eating within 2-3 hours of bedtime, as tirzepatide's effect on gastric emptying may cause discomfort when lying down. Creating a cool, dark sleeping environment and limiting screen time before bed can improve sleep quality.
Physical activity, while challenging when energy is low, paradoxically helps improve overall energy levels. The U.S. Physical Activity Guidelines recommend at least 150 minutes of moderate-intensity activity weekly plus muscle-strengthening activities twice weekly. However, starting with just 10-15 minutes of walking daily and gradually increasing duration and intensity is appropriate when adapting to tirzepatide. Patients should schedule exercise during their highest-energy periods of the day and avoid overexertion.
Stress management techniques including meditation, deep breathing exercises, or gentle yoga can reduce cortisol levels and improve energy perception. Chronic stress depletes energy reserves and may worsen gastrointestinal symptoms. Even 5-10 minutes of daily mindfulness practice can provide measurable benefits.
Medication administration should occur once weekly on the same day as prescribed. Tirzepatide can be taken at any time of day, with consistency being more important than specific timing. Patients should follow their healthcare provider's instructions regarding administration and maintain a regular schedule to support medication effectiveness.
While mild fatigue during the initial weeks of tirzepatide treatment is relatively common, certain symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience severe or worsening fatigue that interferes with daily activities or persists despite adequate nutrition, hydration, and rest.
Signs of dehydration requiring medical attention include dark-colored urine, dizziness upon standing, rapid heartbeat, confusion, or decreased urination. These symptoms may indicate significant fluid and electrolyte imbalances that require evaluation and possible intervention.
Persistent nausea or vomiting lasting more than 24-48 hours can lead to dangerous dehydration and nutritional deficiencies and should be reported promptly.
Symptoms of pancreatitis, including severe abdominal pain that may radiate to the back, with or without vomiting, require immediate medical attention. Similarly, signs of gallbladder disease such as pain in the right upper abdomen, fever, or yellowing of the skin or eyes should prompt urgent evaluation.
Symptoms suggestive of hypoglycemia—including shakiness, sweating, confusion, irritability, or rapid heartbeat—require immediate attention, particularly in patients taking tirzepatide alongside insulin or sulfonylureas. If hypoglycemia is suspected, patients should check their blood glucose if possible and consume 15 grams of fast-acting carbohydrate (such as glucose tablets or 4 oz of juice) if levels are below 70 mg/dL, then recheck after 15 minutes.
Unexplained weight loss that is rapid or associated with inability to maintain adequate nutrition should prompt evaluation for medication dose adjustment or nutritional intervention.
Patients should also report new or worsening depression, anxiety, or mood changes, as these can manifest as fatigue and may require separate evaluation and management.
Call 911 or seek emergency care immediately for chest pain, severe shortness of breath, confusion, or focal neurological symptoms such as one-sided weakness or difficulty speaking.
Before any scheduled appointment, patients should document their symptoms, including timing, severity, and any associated factors. Keeping a food and symptom diary can help healthcare providers identify patterns and develop targeted interventions.
Successful long-term energy management on tirzepatide requires ongoing attention and periodic reassessment as treatment progresses. Most patients experience adaptation over time, with energy levels typically improving as the body adjusts to the medication's effects and patients develop sustainable eating patterns.
Regular monitoring should include assessment of nutritional status, particularly during dose escalation phases. Laboratory testing may be appropriate based on individual risk factors and symptoms, rather than on a fixed schedule. Patients who have undergone significant weight loss may require adjustment of other medications, including thyroid hormone replacement or blood pressure medications, which can impact energy levels.
Protein preservation becomes increasingly important with sustained weight loss. Resistance training exercises 2-3 times weekly help maintain muscle mass, which supports metabolic rate and functional energy. Working with a physical therapist or certified trainer can ensure proper technique and appropriate progression, reducing injury risk.
Dietary evolution should occur as patients progress through treatment. Initial strategies focused on managing nausea and maintaining basic nutrition may need refinement as tolerance improves. Consulting with a registered dietitian experienced in weight management medications can provide personalized guidance for optimizing energy while continuing to achieve weight loss or glycemic goals.
Dose optimization may be necessary for some patients. For weight management, tirzepatide (Zepbound) starts at 2.5 mg weekly and can be titrated at 4-week intervals to maintenance doses of 5 mg, 10 mg, or 15 mg weekly based on response and tolerability. Some individuals may find better energy levels at lower maintenance doses. This decision should be made collaboratively with healthcare providers, considering both efficacy and quality of life.
Screening for other causes of persistent fatigue is important. Conditions such as obstructive sleep apnea, anemia, thyroid disorders, and depression can contribute to low energy and may require specific treatment.
Realistic expectations are essential for long-term success. Some degree of reduced energy may persist as the body adapts to a lower body weight and reduced caloric intake. However, many patients report that improved metabolic health, better sleep quality, and enhanced physical function ultimately result in net energy improvements compared to pre-treatment baseline.
Tirzepatide may cause fatigue through several mechanisms including reduced caloric intake from decreased appetite, slower gastric emptying, gastrointestinal side effects leading to dehydration, and the body's adjustment to normalized blood glucose levels. Most patients find energy levels improve as their bodies adapt to the medication.
Adults on tirzepatide should aim for 1.0-1.2 grams of protein per kilogram of body weight daily, with higher amounts (1.2-1.6 g/kg) recommended for older adults or those engaging in regular physical activity. Distributing protein across meals helps preserve muscle mass and provides sustained energy during weight loss.
Contact your healthcare provider if you experience severe or worsening fatigue interfering with daily activities, signs of dehydration (dark urine, dizziness, confusion), persistent vomiting lasting more than 24-48 hours, severe abdominal pain, or symptoms of hypoglycemia. Seek emergency care immediately for chest pain, severe shortness of breath, or neurological symptoms.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.