LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Is tirzepatide hard on the liver? This question concerns many patients considering this FDA-approved medication for type 2 diabetes and chronic weight management. Tirzepatide is a dual GIP and GLP-1 receptor agonist that works by enhancing insulin secretion, suppressing glucagon, and reducing appetite. Unlike many medications, tirzepatide is eliminated through protein breakdown rather than extensive liver processing, and no dose adjustment is needed for hepatic impairment. Current evidence suggests tirzepatide is not hepatotoxic and may actually benefit liver health in patients with metabolic dysfunction-associated steatotic liver disease (MASLD). Understanding tirzepatide's liver safety profile helps patients and clinicians make informed treatment decisions.
Quick Answer: Tirzepatide is not hard on the liver and does not cause hepatotoxicity in most patients based on extensive clinical trial data.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. As a once-weekly injectable medication, it works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
The liver plays a central role in glucose and lipid metabolism, making it a key organ of interest when evaluating any diabetes or weight-loss medication. Tirzepatide influences hepatic function indirectly through improved glycemic control, reduced insulin resistance, and weight loss—all factors that can positively impact liver health. The medication is primarily eliminated through proteolytic catabolism rather than hepatic metabolism, which distinguishes it from drugs that undergo extensive liver processing. According to FDA prescribing information, no dose adjustment is recommended for patients with hepatic impairment.
Current evidence does not suggest that tirzepatide is hepatotoxic, though rare idiosyncratic reactions cannot be completely excluded, as with any medication. The FDA prescribing information does not list hepatotoxicity as a known adverse effect, and pre-marketing clinical trials did not identify significant liver-related safety signals. However, tirzepatide does carry a labeled risk of gallbladder disease (cholelithiasis and cholecystitis), which can present with liver function test abnormalities. Understanding tirzepatide's relationship with liver function remains important for clinicians and patients, particularly those with pre-existing liver conditions or metabolic dysfunction-associated steatotic liver disease (MASLD), formerly known as non-alcoholic fatty liver disease (NAFLD).
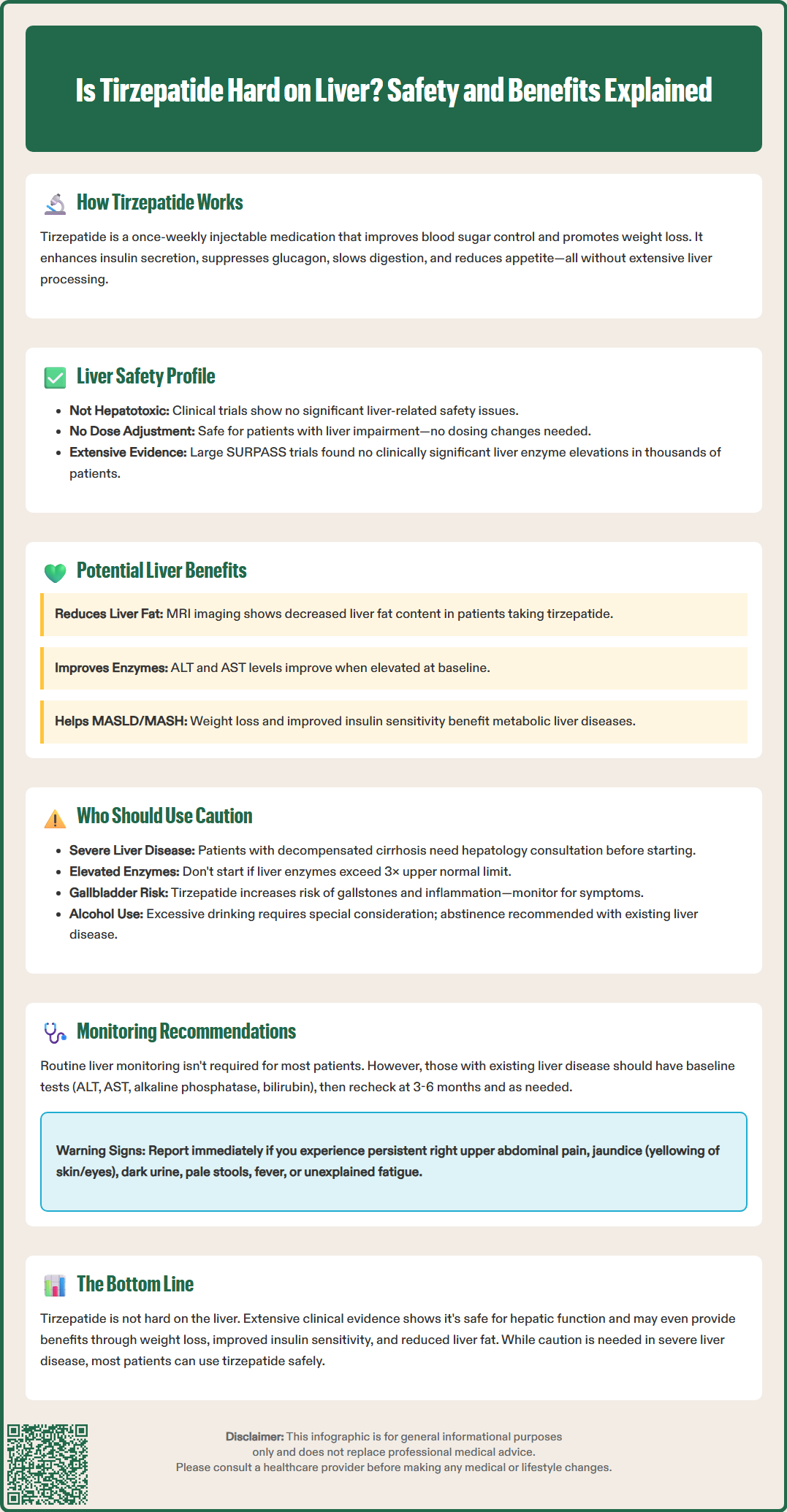
Large-scale clinical trials have provided reassuring data regarding tirzepatide's safety profile concerning liver function. The SURPASS clinical trial program, which enrolled thousands of patients with type 2 diabetes, systematically monitored liver enzymes including alanine aminotransferase (ALT) and aspartate aminotransferase (AST). These studies did not demonstrate clinically significant elevations in liver enzymes attributable to tirzepatide therapy.
In the SURPASS-3 trial comparing tirzepatide to insulin degludec, liver enzyme elevations were infrequent and generally mild when they occurred. Importantly, the incidence of liver enzyme abnormalities was not higher in tirzepatide-treated patients compared to control groups. A substudy of SURPASS-3 using magnetic resonance imaging-proton density fat fraction (MRI-PDFF) demonstrated significant reductions in liver fat content with tirzepatide treatment.
Post-marketing surveillance has not identified a consistent hepatotoxicity signal, though the FDA Adverse Event Reporting System (FAERS) contains some reports of hepatobiliary adverse events where causality has not been established. Spontaneous reporting systems have inherent limitations in determining true incidence or causation.
The SURMOUNT trials, evaluating tirzepatide for chronic weight management in adults without diabetes, further support its hepatic safety profile. These studies included participants with obesity-related comorbidities and showed that substantial weight loss achieved with tirzepatide was not associated with deterioration in liver function markers.
While tirzepatide does not appear to cause liver damage in most patients, individual responses can vary. Rare idiosyncratic reactions are theoretically possible with any medication. The absence of a clear hepatotoxicity signal across extensive clinical trial data provides reassurance that tirzepatide is generally not harmful to the liver for most patients.
Emerging evidence suggests that tirzepatide may benefit liver health, particularly in patients with metabolic dysfunction-associated steatotic liver disease (MASLD) and metabolic dysfunction-associated steatohepatitis (MASH), previously termed non-alcoholic steatohepatitis (NASH). These conditions, characterized by excessive fat accumulation and inflammation in the liver, are closely linked to obesity, insulin resistance, and type 2 diabetes—conditions that tirzepatide effectively addresses.
The SURPASS-3 MRI substudy demonstrated that tirzepatide treatment led to significant reductions in hepatic fat content, as measured by MRI-PDFF. In patients with type 2 diabetes and presumed MASLD, tirzepatide therapy resulted in meaningful decreases in liver fat percentage. More recently, the SYNERGY-NASH trial (published in NEJM 2024) specifically evaluated tirzepatide in patients with MASH, showing improvements in histologic endpoints. However, it's important to note that tirzepatide is not FDA-approved for the treatment of MASLD or MASH, and any such use would be considered off-label.
The mechanisms underlying these hepatic benefits are multifactorial. Tirzepatide's effects on weight reduction directly decrease hepatic lipid accumulation. Improved insulin sensitivity reduces hepatic glucose production and lipogenesis. Additionally, GLP-1 receptor activation may influence hepatic metabolism, though the precise mechanisms remain under investigation.
Biomarker improvements further suggest tirzepatide's positive liver effects. Patients treated with tirzepatide have shown reductions in ALT and AST levels when these were elevated at baseline. Improvements in non-invasive fibrosis markers, such as the Fibrosis-4 (FIB-4) index and NAFLD fibrosis score, have also been observed, though these are surrogate markers and do not definitively confirm histologic fibrosis regression. Longer-term studies are needed to determine if these changes translate to improved clinical outcomes in patients with liver disease.
While tirzepatide is not considered hepatotoxic, certain patient populations warrant careful consideration and monitoring. Patients with pre-existing severe liver disease, including decompensated cirrhosis, were generally excluded from pivotal clinical trials, meaning safety data in this population are limited. For patients with advanced liver disease, the decision to initiate tirzepatide should involve careful risk-benefit assessment and consultation with hepatology specialists when appropriate.
Patients with a history of drug-induced liver injury from other medications should be monitored closely, though no specific link exists with tirzepatide. Baseline liver function testing is prudent in these individuals to establish a reference point. Additionally, patients with acute hepatitis or significantly elevated baseline liver enzymes (ALT or AST greater than three times the upper limit of normal) should have their liver condition evaluated and stabilized before initiating tirzepatide.
Tirzepatide carries a labeled risk of gallbladder disease, including cholelithiasis and cholecystitis. Patients with a history of gallbladder disease or risk factors should be informed about this risk and advised to report symptoms such as right upper quadrant pain, fever, or jaundice promptly.
Individuals with excessive alcohol consumption require special consideration, as alcohol itself is hepatotoxic. The American Association for the Study of Liver Diseases (AASLD) recommends addressing alcohol use as a primary intervention for liver health. US guidelines suggest limiting alcohol to ≤2 drinks/day for men and ≤1 drink/day for women, with abstinence advised for those with liver disease.
Women using oral contraceptives should be aware that tirzepatide may reduce the effectiveness of these medications due to delayed gastric emptying. The FDA label recommends using non-oral contraceptives or adding a backup method for 4 weeks after tirzepatide initiation or dose increases. Healthcare providers should conduct a thorough medication review before prescribing tirzepatide, focusing particularly on medications with narrow therapeutic indices that might be affected by delayed gastric emptying.
Routine liver function monitoring is not specifically required for patients taking tirzepatide according to FDA prescribing information, as hepatotoxicity is not an established adverse effect. However, clinical judgment should guide individualized monitoring strategies based on patient-specific risk factors and baseline liver health status.
For patients with known liver disease or elevated baseline liver enzymes, periodic monitoring of hepatic function tests is reasonable. A practical approach includes checking ALT, AST, alkaline phosphatase, and total bilirubin at baseline before initiating tirzepatide, then reassessing at 3 to 6 months after starting therapy, and subsequently as clinically indicated. Consider holding tirzepatide if ALT/AST exceed 3 times the upper limit of normal with symptoms, or if bilirubin exceeds 2 times the upper limit of normal, pending evaluation.
Patients with MASLD or MASH may benefit from more structured monitoring, including non-invasive assessments of liver fibrosis such as FIB-4 index calculation or vibration-controlled transient elastography (FibroScan) when available. According to AASLD guidance, FIB-4 scores <1.3 indicate low risk, while scores >2.67 (or >2.0 for patients over age 65) suggest higher risk and warrant hepatology referral or additional testing.
If patients develop right upper quadrant pain, especially with fever or jaundice, prompt evaluation including abdominal ultrasound is recommended to assess for gallbladder disease, a known risk with tirzepatide therapy.
Patients should be educated about symptoms that might indicate liver problems. Warning signs include persistent right upper quadrant abdominal pain, jaundice (yellowing of skin or eyes), dark urine, pale stools, or unexplained fatigue. Any such symptoms warrant prompt medical evaluation and liver function testing. The most common side effects of tirzepatide are gastrointestinal, including nausea, diarrhea, vomiting, and constipation, which are unrelated to liver function. These typically improve over time and can be managed through dose titration and dietary modifications. Regular follow-up visits provide opportunities to assess overall treatment response, adjust therapy as needed, and ensure comprehensive metabolic and hepatic health monitoring.
Current evidence from large clinical trials does not suggest that tirzepatide causes liver damage. The FDA prescribing information does not list hepatotoxicity as a known adverse effect, and extensive clinical trial data have not identified significant liver-related safety signals.
Routine liver function monitoring is not specifically required for tirzepatide according to FDA prescribing information. However, patients with known liver disease or elevated baseline liver enzymes may benefit from periodic monitoring based on individual clinical judgment.
Emerging evidence suggests tirzepatide may benefit patients with metabolic dysfunction-associated steatotic liver disease (MASLD) by reducing hepatic fat content and improving liver enzyme levels. However, tirzepatide is not FDA-approved for treating MASLD, and any such use would be considered off-label.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.