LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Starting tirzepatide represents a significant step in managing type 2 diabetes or achieving weight loss goals. This dual GIP/GLP-1 receptor agonist, available as Mounjaro for diabetes and Zepbound for weight management, requires careful initiation with gradual dose escalation. Understanding what to expect when starting tirzepatide—from initial side effects to anticipated metabolic improvements—helps patients prepare for treatment and optimize outcomes. This guide provides comprehensive information on dosing protocols, common experiences during the first weeks, expected clinical benefits, and practical strategies for successful long-term therapy.
Quick Answer: When starting tirzepatide, patients can expect a gradual dose escalation beginning at 2.5 mg weekly, with gastrointestinal side effects like nausea and diarrhea being most common during the first weeks, followed by progressive improvements in blood sugar control and weight reduction over subsequent months.
Tirzepatide is a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide works through a dual mechanism of action that affects glucose metabolism and appetite regulation.
When tirzepatide binds to GLP-1 receptors, it stimulates insulin secretion in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated. This mechanism helps reduce the risk of hypoglycemia compared to some other diabetes medications, though the risk increases when used with insulin or sulfonylureas. GLP-1 receptor activation also suppresses glucagon secretion, slows gastric emptying, and promotes satiety through central nervous system pathways.
The GIP receptor activation component appears to provide complementary metabolic effects. In clinical trials, this dual-receptor approach has shown effective glycemic control and weight reduction. Tirzepatide is administered as a once-weekly subcutaneous injection.
Importantly, tirzepatide is not indicated for patients with type 1 diabetes or diabetic ketoacidosis. It is also not recommended for patients with a personal or family history of medullary thyroid carcinoma or in patients with Multiple Endocrine Neoplasia syndrome type 2, due to thyroid C-cell tumor risk observed in animal studies.
Tirzepatide therapy begins with a low starting dose to minimize gastrointestinal side effects and allow the body to adjust to the medication. The FDA-approved initial dose is 2.5 mg administered subcutaneously once weekly for the first four weeks. This starting dose serves primarily as a tolerability dose rather than a therapeutic dose, helping patients acclimate to the medication's effects on the gastrointestinal system.
After the initial four-week period, the dose is typically increased to 5 mg once weekly. Subsequent dose escalations occur in 2.5 mg increments at four-week intervals, based on individual glycemic response, weight loss goals, and tolerability. The maximum approved dose is 15 mg once weekly for both diabetes and weight management indications. Healthcare providers may maintain patients at lower doses if therapeutic goals are achieved or if higher doses are not well tolerated. The American Diabetes Association guidelines emphasize individualized treatment approaches, recognizing that not all patients require maximum dosing.
Administration technique is straightforward but requires proper instruction. Tirzepatide is injected subcutaneously into the abdomen, thigh, or upper arm using a pre-filled, single-dose pen. Patients should rotate injection sites weekly to prevent lipodystrophy. The injection can be administered at any time of day, with or without meals, but maintaining a consistent day each week optimizes adherence. If a dose is missed, it should be administered within four days; if more than four days have passed, the missed dose should be skipped, and the regular schedule resumed. The weekly injection day can be changed if at least 72 hours have elapsed since the last dose.
Patients should receive comprehensive training on injection technique, pen storage (keep unused pens refrigerated; if needed, they may be kept at room temperature not above 86°F for up to 21 days; discard after use), and proper disposal of sharps. Patients taking oral contraceptives should use non-hormonal or backup contraception for 4 weeks after starting tirzepatide and after each dose increase, as tirzepatide may reduce oral contraceptive effectiveness. Patients taking insulin or sulfonylureas may need dose adjustments of these medications to prevent hypoglycemia.
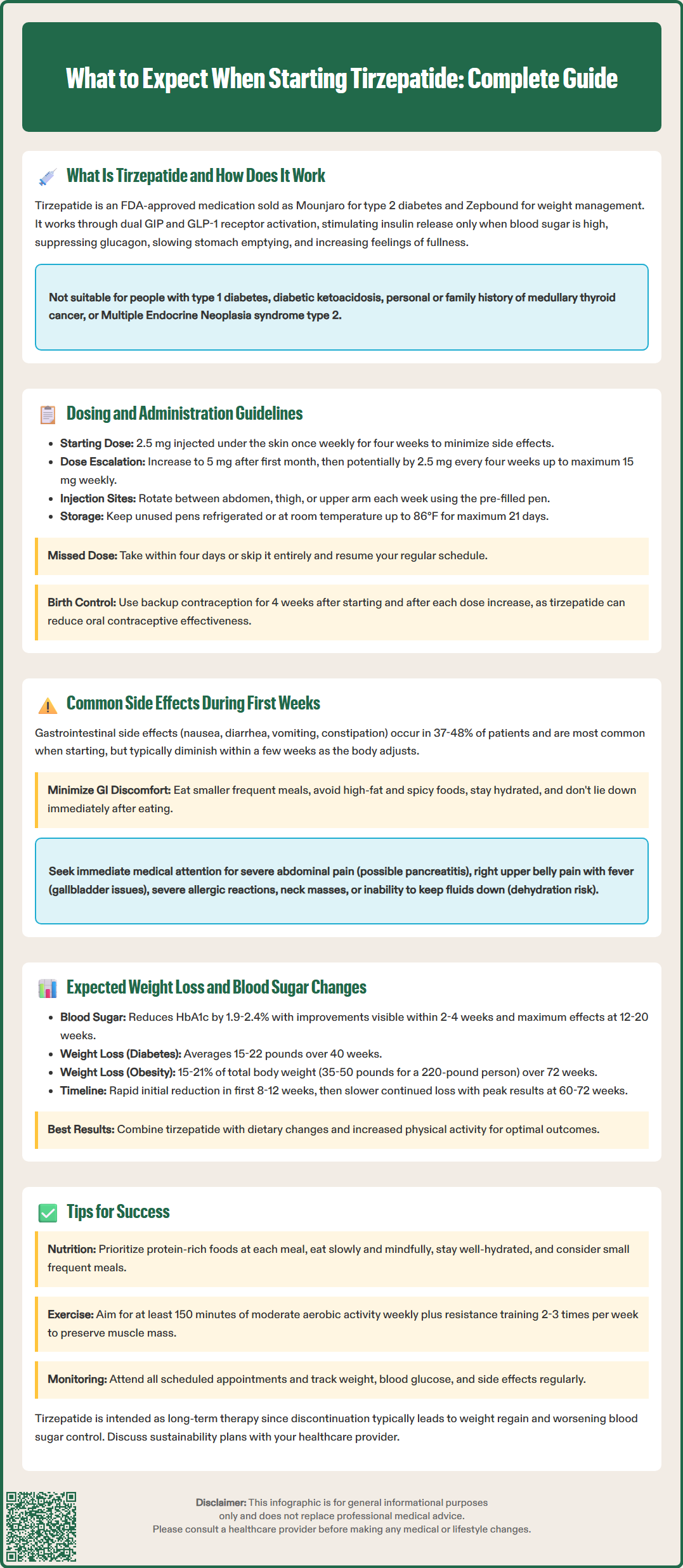
The most frequently reported side effects when starting tirzepatide are gastrointestinal in nature. In clinical trials, gastrointestinal adverse events occurred in 37-48% of patients (depending on dose), with higher rates at higher doses. These effects generally tend to diminish over time as the body adjusts to the medication. The most common adverse effects include nausea (12-24%), diarrhea (12-17%), decreased appetite (10-14%), vomiting (6-12%), constipation (11-17%), dyspepsia, and abdominal pain. Nausea is typically the most prominent symptom, particularly during dose escalation periods.
These gastrointestinal effects result from tirzepatide's mechanism of action, specifically its slowing of gastric emptying and effects on satiety centers in the brain. Most patients experience mild to moderate symptoms that improve within the first few weeks at each dose level. To minimize discomfort, patients should eat smaller, more frequent meals, avoid high-fat and spicy foods, stay well-hydrated, and avoid lying down immediately after eating. Anti-emetic medications may be considered for significant nausea if needed.
Other common side effects during the initial treatment period include fatigue, injection site reactions (redness, itching, or mild discomfort), and headache. These symptoms are generally transient and resolve without intervention. Patients should be counseled that experiencing some gastrointestinal discomfort is normal and does not indicate treatment failure or intolerance, provided symptoms remain manageable.
Serious adverse effects are rare but require immediate medical attention. These include signs of pancreatitis (severe, persistent abdominal pain radiating to the back), symptoms of gallbladder disease (right upper quadrant pain, fever, jaundice), severe allergic reactions, or signs of thyroid tumors (neck mass, difficulty swallowing, persistent hoarseness). Severe gastrointestinal symptoms may lead to dehydration and acute kidney injury; patients should seek medical care if unable to maintain adequate fluid intake. Tirzepatide is not recommended for patients with a history of pancreatitis or severe gastrointestinal disease, including gastroparesis. The medication should not be used during pregnancy or breastfeeding.
Clinical trial data provide robust evidence for tirzepatide's efficacy in both glycemic control and weight reduction. In the SURPASS clinical trial program evaluating patients with type 2 diabetes, tirzepatide demonstrated HbA1c reductions of 1.9-2.4% from baseline, with higher doses producing greater effects. In the SURPASS-1 monotherapy trial, approximately 51-62% of patients achieved an HbA1c below 5.7% (non-diabetic range) at the highest doses. Fasting glucose improvements typically become apparent within the first 2-4 weeks of treatment, with maximal glycemic effects observed after 12-20 weeks at the maintenance dose.
Weight loss with tirzepatide is substantial and progressive. In diabetes trials, patients lost an average of 15-22 pounds (7-10 kg) over 40 weeks, depending on the dose. The SURMOUNT-1 trial, which evaluated tirzepatide specifically for weight management in patients with obesity, demonstrated even more impressive results: average weight reductions of 15% (10 mg dose) to 20.9% (15 mg dose) of initial body weight over 72 weeks. This translates to approximately 35-50 pounds for a 220-pound individual.
Weight loss typically follows a predictable pattern. Patients may notice initial rapid weight reduction during the first 8-12 weeks, followed by continued but slower weight loss over subsequent months. Peak weight loss generally occurs between 60-72 weeks of treatment. Individual responses vary considerably based on baseline weight, adherence to lifestyle modifications, dose achieved, and metabolic factors. Patients should understand that tirzepatide is most effective when combined with dietary changes and increased physical activity.
It is important to set realistic expectations. Not all patients will achieve the average weight loss seen in clinical trials, and some individuals may be "non-responders" or experience more modest results. According to the FDA label for Zepbound, treatment response should be evaluated after 12 weeks on a maintenance dose; if patients have not achieved at least 5% weight loss, discontinuation should be considered. For diabetes management, regular monitoring of HbA1c (every 3 months initially) and body weight helps assess treatment efficacy and guide dose adjustments.
Successful tirzepatide therapy requires active patient engagement and lifestyle optimization. While the medication provides powerful metabolic effects, combining it with evidence-based lifestyle modifications significantly enhances outcomes and promotes long-term success. Patients should work with their healthcare team to develop a comprehensive treatment plan that addresses diet, physical activity, and behavioral factors.
Dietary strategies are crucial for maximizing benefits and minimizing side effects. Focus on protein-rich foods at each meal to promote satiety and preserve lean muscle mass during weight loss. Consider working with a registered dietitian to develop an individualized meal plan. Emphasize whole foods, vegetables, fruits, and whole grains while limiting processed foods, added sugars, and excessive fats. Eat slowly and mindfully, stopping when comfortably satisfied rather than overly full. Stay well-hydrated throughout the day, as dehydration can worsen gastrointestinal side effects and fatigue. Small, frequent meals often work better than large meals, particularly during the initial treatment weeks.
Physical activity enhances weight loss, improves insulin sensitivity, and helps maintain muscle mass. The American Diabetes Association recommends at least 150 minutes of moderate-intensity aerobic activity weekly, plus resistance training 2-3 times per week. Start gradually if currently sedentary, and increase activity progressively as tolerance improves. Even modest increases in daily movement—such as taking stairs, parking farther away, or short walking breaks—contribute to overall success.
Monitoring and follow-up are essential components of safe, effective treatment. Attend all scheduled appointments for dose adjustments, side effect assessment, and metabolic monitoring. Track your weight, blood glucose levels (if diabetic), and any side effects in a journal or smartphone app. Contact your healthcare provider promptly for concerning symptoms, including severe or persistent abdominal pain, signs of dehydration (extreme thirst, dizziness, dark urine), jaundice, or unexplained symptoms. Seek immediate medical attention for severe abdominal pain with vomiting, signs of allergic reaction, or symptoms of hypoglycemia if taking insulin or sulfonylureas. Regular laboratory monitoring typically includes HbA1c every 3 months, lipid panels, kidney function tests, and liver enzymes as clinically indicated.
If you're planning surgery or a procedure requiring anesthesia, inform your surgical team about your tirzepatide use, as they may provide specific instructions about timing your dose. Women of childbearing potential should use effective contraception while on tirzepatide, with non-hormonal or backup methods recommended during the first 4 weeks of treatment and after each dose increase.
Finally, understand that tirzepatide is generally intended as a long-term therapy. Discontinuation often results in weight regain and worsening glycemic control. Discuss treatment duration, cost considerations, and long-term plans with your healthcare provider to ensure sustainable management of your metabolic health.
Blood sugar improvements typically become apparent within 2-4 weeks of starting tirzepatide, with maximal glycemic effects observed after 12-20 weeks at the maintenance dose. Weight loss begins early but progresses gradually, with peak effects generally occurring between 60-72 weeks of treatment.
The most common side effects are gastrointestinal, including nausea (12-24% of patients), diarrhea (12-17%), decreased appetite (10-14%), vomiting (6-12%), and constipation (11-17%). These effects are typically mild to moderate and improve within the first few weeks at each dose level.
Tirzepatide is generally intended as long-term therapy, as discontinuation often results in weight regain and worsening glycemic control in diabetes patients. Treatment duration and long-term management plans should be discussed with your healthcare provider to ensure sustainable metabolic health outcomes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.