LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Glucagon-like peptide-1 (GLP-1) receptor agonists, FDA-approved medications for type 2 diabetes and obesity, are increasingly recognized for potential anti-inflammatory properties beyond their metabolic effects. Emerging research suggests these agents may reduce inflammatory markers such as C-reactive protein and pro-inflammatory cytokines through mechanisms independent of weight loss or glucose control. While standard therapeutic doses have demonstrated cardiovascular and metabolic benefits in large clinical trials, the concept of using low dose GLP-1 for inflammation remains investigational, with no established FDA indication or standardized dosing protocols. This article examines the scientific evidence, potential mechanisms, clinical applications, and important safety considerations surrounding low-dose GLP-1 therapy for inflammatory conditions.
Quick Answer: Low-dose GLP-1 receptor agonists may exert anti-inflammatory effects by reducing pro-inflammatory cytokines and inflammatory markers, though this application remains investigational without FDA approval or established dosing protocols.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management and subsequently approved for chronic weight management. These agents mimic the action of endogenous GLP-1, an incretin hormone released from intestinal L-cells in response to nutrient intake. The FDA has approved several GLP-1 receptor agonists, including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist, not purely a GLP-1 agent.
The primary mechanism of action involves binding to GLP-1 receptors on pancreatic beta cells, which enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release. This glucose-lowering effect has a low intrinsic risk of hypoglycemia, though the risk increases when combined with insulin or sulfonylureas. GLP-1 receptor agonists also slow gastric emptying, reduce appetite through central nervous system pathways, and promote satiety, leading to reduced caloric intake and weight loss.
GLP-1 receptors are distributed throughout the body beyond pancreatic tissue, including in the cardiovascular system and kidneys. Some preclinical and emerging clinical evidence suggests potential expression on immune cells, though this remains an area of ongoing research. This broad receptor distribution has prompted investigation into potential pleiotropic effects beyond glycemic control, including cardiovascular protection, renal benefits, and anti-inflammatory properties. Standard therapeutic doses for diabetes typically range from 0.5 mg to 2 mg weekly for semaglutide (with Wegovy dosing up to 2.4 mg weekly for obesity), though lower doses are used during initial titration to minimize gastrointestinal side effects.
Importantly, these medications carry a boxed warning for risk of thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), and are contraindicated in patients with personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2.
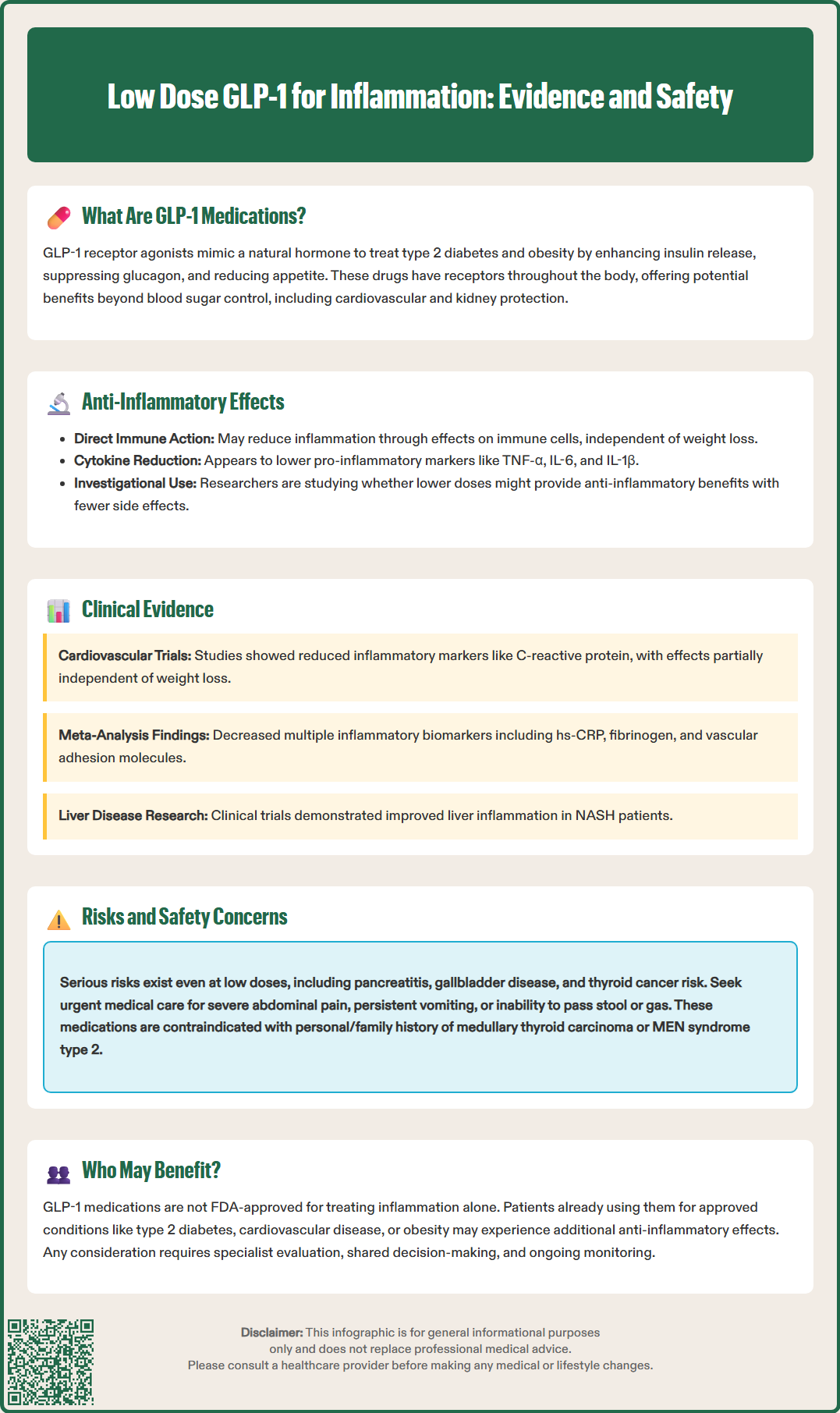
Emerging research suggests that GLP-1 receptor agonists may exert anti-inflammatory effects through multiple pathways, potentially even at doses lower than those typically used for diabetes or weight management. The anti-inflammatory mechanisms appear to be independent of weight loss or glycemic improvement, suggesting direct immunomodulatory properties. Preclinical studies indicate GLP-1 receptors may be expressed on various immune cells, including macrophages, monocytes, and lymphocytes, though human data remains limited.
At the cellular level, GLP-1 receptor activation appears to reduce the production of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-1 beta (IL-1β). These cytokines play central roles in systemic inflammation and are elevated in conditions ranging from metabolic syndrome to cardiovascular disease. Laboratory and animal studies suggest GLP-1 receptor agonists may also inhibit nuclear factor-kappa B (NF-κB) signaling, a key pathway in inflammatory gene expression, and reduce oxidative stress through enhanced antioxidant enzyme activity.
The concept of "low dose" GLP-1 therapy for inflammation remains investigational and lacks standardized definition. Some researchers have explored doses at the initial titration level (for example, 0.25 mg weekly of semaglutide, which is the standard starting dose for Ozempic but subtherapeutic for glycemic control), hypothesizing that anti-inflammatory benefits might be achieved with reduced gastrointestinal side effects. However, there is currently no FDA-approved indication for GLP-1 receptor agonists specifically for inflammation, and the optimal dosing strategy for anti-inflammatory effects has not been established through rigorous clinical trials. Any off-label use should be approached cautiously, ideally within clinical trials, and discussed thoroughly with healthcare providers.
Clinical evidence supporting the anti-inflammatory effects of GLP-1 receptor agonists comes primarily from cardiovascular outcome trials and mechanistic studies, though most research has examined standard therapeutic doses rather than specifically low-dose regimens. The LEADER trial with liraglutide and the SUSTAIN-6 trial with semaglutide demonstrated cardiovascular benefits that may be partially mediated through anti-inflammatory mechanisms. Some analyses from these trials showed modest reductions in inflammatory biomarkers, including high-sensitivity C-reactive protein (hs-CRP).
A systematic review and meta-analysis published in Diabetes, Obesity and Metabolism examined inflammatory markers across multiple GLP-1 receptor agonist trials and found reductions in hs-CRP levels, though the magnitude and clinical significance of these changes varied across studies. These reductions appeared partially independent of weight loss, suggesting potential direct anti-inflammatory effects. Studies have also demonstrated changes in other inflammatory markers, including fibrinogen, plasminogen activator inhibitor-1 (PAI-1), and various adhesion molecules involved in vascular inflammation.
Smaller mechanistic studies have explored GLP-1 effects in specific inflammatory conditions. The LEAN trial with liraglutide and a phase 2 trial of semaglutide in patients with non-alcoholic steatohepatitis (NASH) showed improvements in liver histology and reductions in hepatic inflammation markers. Limited pilot studies in patients with psoriasis have reported improvements in disease severity scores alongside metabolic benefits, though these findings require confirmation in larger trials. The recent SELECT trial examined semaglutide 2.4 mg in people without diabetes but with cardiovascular disease and included biomarker analyses that may provide additional insights.
However, most of these studies used standard doses approved for diabetes or obesity, and dedicated trials examining low-dose GLP-1 specifically for inflammatory conditions are lacking. The American Diabetes Association (ADA) recognizes the cardiovascular benefits of GLP-1 receptor agonists in their Standards of Care but does not currently recommend these agents solely for inflammation management outside established indications for diabetes, obesity, or cardiovascular risk reduction.
The theoretical benefits of low-dose GLP-1 therapy for inflammation include the potential for anti-inflammatory effects with a reduced side effect burden compared to standard doses. The most common adverse effects of GLP-1 receptor agonists are gastrointestinal, including nausea, vomiting, diarrhea, and constipation, which are typically dose-dependent. Lower doses might provide immunomodulatory benefits while minimizing these troublesome symptoms, potentially improving treatment adherence. Additionally, cardiovascular and metabolic benefits observed at therapeutic doses might be partially retained at lower doses, though this remains speculative without dedicated dose-finding studies.
Potential systemic anti-inflammatory effects could theoretically benefit multiple conditions characterized by chronic low-grade inflammation, including metabolic syndrome, cardiovascular disease, and certain autoimmune conditions. The reduction in inflammatory markers such as hs-CRP and IL-6 may contribute to improved endothelial function, reduced atherosclerotic progression, and better overall cardiometabolic health. Some researchers hypothesize that anti-inflammatory effects might also benefit neurodegenerative conditions, though this remains highly investigational.
However, significant risks and uncertainties accompany off-label low-dose use. The safety profile of GLP-1 receptor agonists at doses below those studied in clinical trials is not well characterized. Even at low doses, these medications carry risks including pancreatitis (requiring discontinuation if suspected), gallbladder disease, and rare but serious adverse events such as medullary thyroid carcinoma (boxed warning; contraindicated in patients with personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2). Gastrointestinal side effects may still occur even at reduced doses.
Additional risks include diabetic retinopathy complications (particularly with semaglutide in patients with pre-existing retinopathy), acute kidney injury (especially with volume depletion from gastrointestinal effects), and rare cases of intestinal obstruction or ileus. Patients should seek urgent medical attention for severe abdominal pain, persistent vomiting, or inability to pass stool or gas.
Crucially, there is no established evidence base for efficacy at low doses specifically for inflammation, and the dose-response relationship for anti-inflammatory effects is unknown. Insurance coverage for off-label use is unlikely, making treatment potentially cost-prohibitive. Patients considering low-dose GLP-1 therapy should undergo thorough evaluation, including assessment of contraindications, baseline inflammatory markers if appropriate, and regular monitoring for adverse effects. This approach should only be undertaken under close medical supervision as part of a comprehensive treatment plan.
Given the investigational nature of low-dose GLP-1 therapy for inflammation, identifying appropriate candidates requires careful clinical judgment and shared decision-making. Currently, there is no official FDA indication for GLP-1 receptor agonists specifically targeting inflammation, and clinical guidelines do not recommend this approach outside established indications. However, certain patient populations might theoretically benefit from the anti-inflammatory properties of these agents when used for approved indications.
Patients with type 2 diabetes and elevated inflammatory markers, particularly those with established cardiovascular disease or high cardiovascular risk, represent a group where GLP-1 receptor agonists are already recommended by the ADA and American College of Physicians (ACP). In these individuals, the anti-inflammatory effects may provide additional benefit beyond glycemic control. Similarly, patients with obesity and metabolic syndrome often exhibit chronic low-grade inflammation, and GLP-1 receptor agonists approved for weight management may address both adiposity and inflammatory burden simultaneously.
Patients with non-alcoholic steatohepatitis (NASH) or non-alcoholic fatty liver disease (NAFLD) with concurrent diabetes or obesity might benefit from the hepatic anti-inflammatory effects observed in clinical studies, though GLP-1 receptor agonists are not yet FDA-approved specifically for liver disease. Individuals with inflammatory conditions such as psoriasis who also have metabolic comorbidities might experience dual benefits, though dedicated trials in these populations are lacking.
Conversely, low-dose GLP-1 therapy is not appropriate for patients without established indications, particularly those seeking anti-inflammatory effects alone without diabetes or obesity. Contraindications include personal or family history of medullary thyroid carcinoma, Multiple Endocrine Neoplasia syndrome type 2, and severe gastroparesis. Caution is advised in patients with a history of pancreatitis, and these medications should be avoided during pregnancy or discontinued well before planned conception (e.g., 2 months before planned pregnancy for semaglutide based on its half-life).
Patients should be counseled that evidence for low-dose regimens specifically for inflammation is limited, and alternative evidence-based anti-inflammatory strategies (lifestyle modification, statins, specific anti-inflammatory medications for diagnosed conditions) should be prioritized. Any consideration of GLP-1 therapy should involve comprehensive evaluation by an endocrinologist or appropriate specialist, with clear discussion of the investigational nature of this approach, potential risks, costs, and the importance of ongoing monitoring.
Emerging research suggests GLP-1 receptor agonists may reduce inflammatory markers such as C-reactive protein and pro-inflammatory cytokines, though dedicated clinical trials examining low-dose regimens specifically for inflammation are lacking. Most evidence comes from standard therapeutic doses used for diabetes or obesity management.
Risks include gastrointestinal side effects, pancreatitis, gallbladder disease, and a boxed warning for thyroid C-cell tumors. The safety profile at doses below those studied in clinical trials is not well characterized, and there is no FDA approval for this indication.
Currently, GLP-1 receptor agonists should only be used for FDA-approved indications such as type 2 diabetes or obesity. Patients with these conditions who also have elevated inflammatory markers may experience additional anti-inflammatory benefits, but use solely for inflammation outside established indications is not recommended.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.