LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is an FDA-approved dual GIP/GLP-1 receptor agonist that significantly slows gastric emptying. While there are no absolute dietary restrictions, certain foods commonly worsen gastrointestinal side effects like nausea, bloating, and discomfort. Understanding which foods to avoid or limit on tirzepatide—particularly high-fat, fried, and heavily processed options—can dramatically improve treatment tolerance and adherence. Strategic dietary modifications, especially during dose initiation and escalation, help patients manage side effects while achieving their therapeutic goals for diabetes control or weight management.
Quick Answer: High-fat foods, fried items, spicy dishes, carbonated beverages, and heavily processed carbohydrates should be limited on tirzepatide to reduce gastrointestinal side effects.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). Its mechanism of action directly influences gastrointestinal function, which can alter how patients tolerate certain foods.
The medication works by mimicking incretin hormones that regulate blood glucose and appetite. Tirzepatide slows gastric emptying—the rate at which food moves from the stomach into the small intestine—which prolongs satiety and helps control postprandial glucose excursions. This delayed gastric emptying means food remains in the stomach longer than usual, increasing the likelihood of gastrointestinal discomfort when consuming foods that are difficult to digest or that stimulate excessive gastric acid production.
Gastrointestinal adverse effects are the most commonly reported side effects of tirzepatide. In the SURPASS clinical trials for type 2 diabetes, nausea occurred in 12–22% of patients, diarrhea in 12–16%, and vomiting in 5–9%, with incidence varying by dose. In the SURMOUNT trials for obesity, these rates were even higher, with nausea affecting up to 24–30% of patients. These effects are typically most pronounced during dose initiation and escalation, though some patients experience persistent symptoms throughout treatment. While the gastric emptying effects may attenuate over time with continued use, GI symptoms can still persist.
Importantly, patients should be aware of serious safety concerns related to GI effects. The FDA label includes warnings about pancreatitis, gallbladder disease, and risk of dehydration leading to acute kidney injury. Tirzepatide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis.
Understanding this pharmacological impact on digestion helps explain why certain dietary modifications can significantly improve tolerability. Patients who adjust their food choices to accommodate slower gastric emptying often report fewer gastrointestinal symptoms and better treatment adherence.
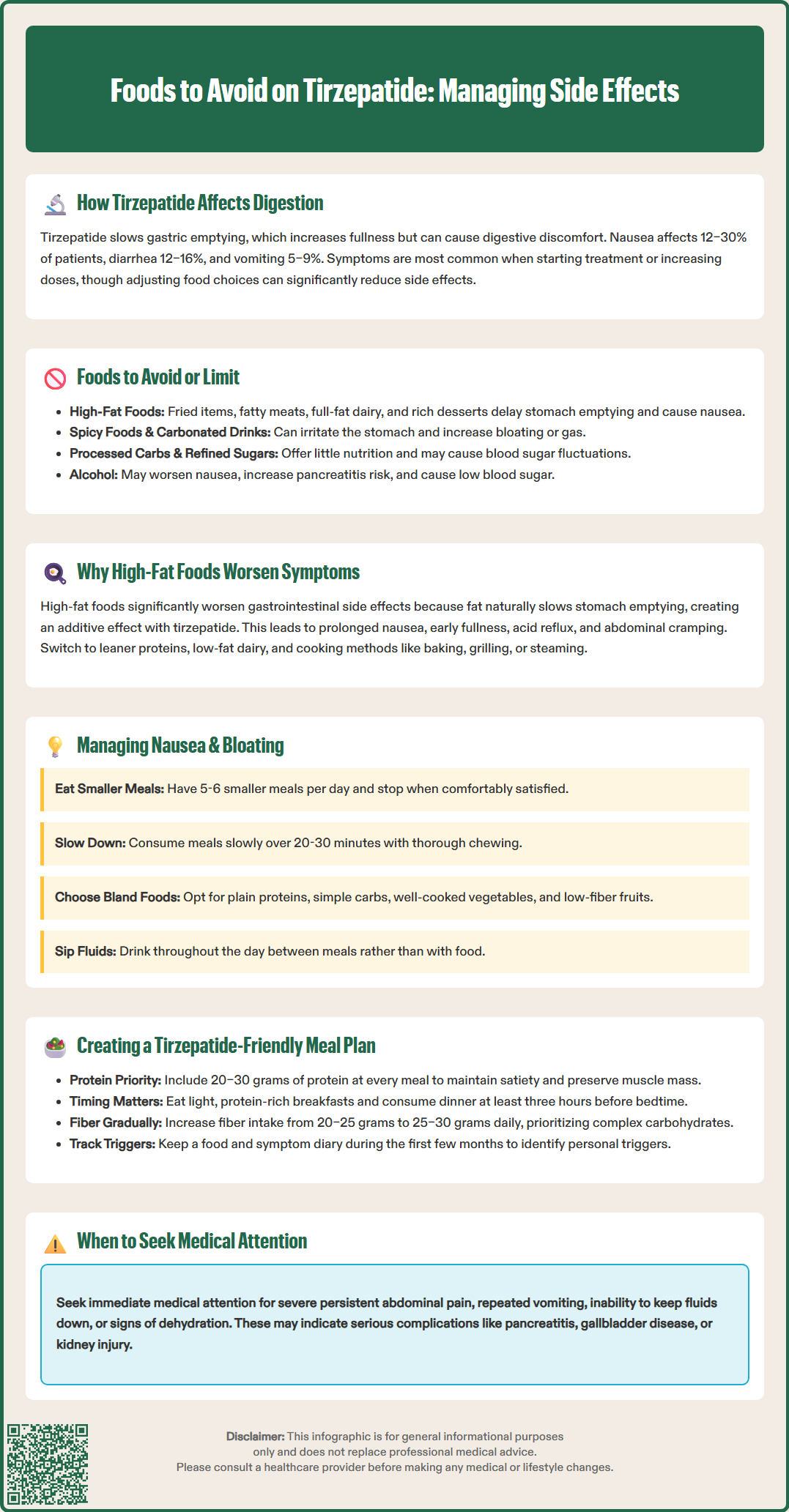
While tirzepatide does not have absolute dietary restrictions, clinical experience and patient reports consistently identify specific food categories that commonly trigger or worsen gastrointestinal side effects. Limiting these foods, particularly during dose initiation and escalation, can improve treatment tolerance.
High-fat foods top the list of problematic items. Foods with significant fat content delay gastric emptying even in individuals not taking tirzepatide. When combined with the medication's effect, this creates a compounding delay that can lead to prolonged fullness, nausea, and discomfort. Examples include:
Fried foods (french fries, fried chicken, donuts)
Fatty cuts of meat (ribeye steak, pork belly, dark meat poultry with skin)
Full-fat dairy products (whole milk, cream, regular cheese)
Processed meats (bacon, sausage, salami)
Rich desserts (ice cream, cheesecake, pastries)
Spicy foods can irritate the gastric lining and exacerbate nausea, particularly when food remains in the stomach for extended periods. Hot peppers, curry dishes, and heavily spiced foods may be poorly tolerated.
Highly processed and refined carbohydrates may cause rapid blood sugar fluctuations. White bread, sugary cereals, candy, and sweetened beverages offer little nutritional value while potentially contributing to discomfort.
Carbonated beverages introduce gas into an already slower-emptying stomach, potentially increasing bloating and fullness. This includes soda, sparkling water, and beer. Individual tolerance varies.
Sugar alcohols (sorbitol, mannitol, xylitol) found in sugar-free gum, mints, and many diet products can cause gas, bloating, and diarrhea in some individuals.
Cruciferous vegetables and legumes, while nutritious, are known gas-producing foods. Broccoli, cabbage, Brussels sprouts, beans, and lentils may worsen bloating in tirzepatide users, though tolerance varies individually.
Alcohol should be consumed in moderation, if at all. Heavy alcohol use may worsen nausea and increase pancreatitis risk. For patients also taking insulin or sulfonylureas, alcohol may increase hypoglycemia risk.
Patients should note that food tolerance is highly individual. Some people tolerate foods that others cannot, and tolerance often improves after the initial adjustment period. Consider testing your tolerance to these foods gradually as your body adjusts to treatment.
The relationship between high-fat foods and increased gastrointestinal side effects in tirzepatide users has a clear physiological basis. Understanding this mechanism helps patients make informed dietary choices and anticipate potential reactions.
Dietary fat is the macronutrient that most significantly delays gastric emptying under normal circumstances. When fat enters the duodenum (the first part of the small intestine), it triggers the release of cholecystokinin (CCK) and other hormones that signal the stomach to slow its emptying rate. This physiological response allows adequate time for fat digestion and absorption. However, when a patient is taking tirzepatide—which already substantially delays gastric emptying through GLP-1 receptor activation—adding high-fat foods creates an additive effect that can result in uncomfortable digestive symptoms.
Fried foods present additional challenges beyond their fat content. The combination of high fat content and often significant portion sizes makes fried foods particularly problematic for patients on tirzepatide.
Clinical observations suggest that consuming high-fat meals while on tirzepatide can trigger:
Prolonged nausea lasting several hours after eating
Early satiety that prevents adequate nutritional intake
Gastroesophageal reflux symptoms
Abdominal cramping, bloating, or diarrhea in some individuals
The fat content threshold that triggers symptoms varies among individuals. Many patients find that gradually reducing fat intake and choosing leaner proteins, low-fat dairy options, and cooking methods like baking, grilling, or steaming rather than frying can improve tolerance. Patients who previously consumed high-fat diets may need to make substantial adjustments, but these modifications typically become easier as new eating patterns are established and weight loss progresses.
The American Diabetes Association's nutrition guidance suggests that total fat intake typically ranges from 20-35% of total calories, though individual needs vary. Working with a registered dietitian can help develop personalized strategies for managing fat intake while ensuring nutritional adequacy.
Nausea and bloating are the most frequently reported gastrointestinal side effects of tirzepatide, but strategic dietary modifications can significantly reduce their severity and frequency. These approaches, based on clinical practice and principles used for delayed gastric emptying, focus on both food selection and eating patterns.
Portion control is fundamental. Smaller, more frequent meals accommodate the reduced gastric capacity created by delayed emptying. Rather than three large meals, patients often tolerate five to six smaller meals better. A practical guideline is to eat until comfortably satisfied—not full—and to stop immediately if fullness or nausea begins.
Eating pace matters considerably. Consuming meals slowly, with thorough chewing, reduces the volume of food entering an already slow-emptying stomach at any given time. Patients should aim for 20–30 minutes per meal, putting utensils down between bites.
Bland, easily digestible foods form the foundation of a nausea-reducing diet:
Plain proteins: skinless chicken breast, white fish, eggs, tofu
Simple carbohydrates: white rice, plain pasta, crackers, toast
Cooked vegetables: carrots, zucchini, green beans (well-cooked, not raw)
Bananas, applesauce, and other low-fiber fruits
Ginger may have anti-nausea properties for some patients. Ginger tea, ginger candies, or fresh ginger added to meals may provide relief. Peppermint tea can also soothe digestive discomfort, though patients with gastroesophageal reflux should use it cautiously as it may relax the lower esophageal sphincter.
Hydration strategy requires attention. While adequate fluid intake is essential, drinking large volumes with meals can worsen fullness and nausea. Patients should sip fluids throughout the day between meals rather than consuming large amounts at mealtimes. Target fluid intake should be individualized based on your needs and medical conditions; discuss specific targets with your healthcare provider.
Timing considerations include avoiding lying down within two to three hours after eating, which can worsen reflux and nausea. Some patients find that their worst nausea occurs at specific times relative to their weekly injection; adjusting meal timing or composition around these patterns can help.
When to seek medical attention: Contact your healthcare provider immediately if you experience severe, persistent abdominal pain (with or without vomiting), right upper quadrant pain with fever or jaundice, repeated vomiting, inability to keep fluids down, or signs of dehydration. These may indicate serious conditions requiring prompt medical attention. Your provider may also consider slowing dose escalation, temporarily reducing your dose, or prescribing antiemetic medications if symptoms significantly impact your quality of life or nutritional intake.
A well-structured meal plan that accommodates tirzepatide's effects on digestion while meeting nutritional needs supports both medication tolerance and therapeutic goals. The following framework provides practical guidance for daily eating patterns.
Breakfast options should be light yet protein-containing:
Scrambled egg whites with whole grain toast
Plain Greek yogurt (low-fat) with berries
Oatmeal made with water or low-fat milk, topped with sliced banana
Protein smoothie with whey or plant-based protein, spinach, and frozen fruit
Mid-morning snack (if needed):
Small apple with one tablespoon almond butter
Rice cakes with low-fat cottage cheese
Handful of unsalted almonds (approximately 10–12 nuts)
Lunch emphasizes lean protein and vegetables:
Grilled chicken breast (3–4 ounces) with steamed vegetables and quinoa
Turkey and avocado wrap using a whole wheat tortilla (half portion)
Vegetable soup with white beans (as tolerated) and a small side salad
Baked cod with roasted sweet potato and green beans
Afternoon snack:
Carrot and cucumber sticks with hummus
Low-fat string cheese with whole grain crackers
Small pear or peach
Dinner should be consumed at least three hours before bedtime to reduce reflux risk:
Baked salmon (3 ounces) with asparagus and wild rice
Lean ground turkey stir-fry with mixed vegetables over brown rice
Grilled shrimp with zucchini noodles and marinara sauce
Chicken breast with roasted Brussels sprouts (as tolerated) and small baked potato
Key principles for meal planning:
Protein at every meal: 20–30 grams per meal supports satiety and preserves lean muscle during weight loss (adjust as needed for kidney disease or other conditions)
Fiber gradually increased: Start with 20–25 grams daily, slowly increasing to 25–30 grams as tolerated
Complex carbohydrates prioritized: Whole grains, legumes (as tolerated), and starchy vegetables over refined options
Healthy fats in moderation: Focus on sources like avocado, nuts, seeds, and olive oil, but keep portions small
For gas-producing foods like legumes and cruciferous vegetables, try these strategies: rinse canned beans thoroughly, start with small portions, cook thoroughly, and gradually increase as tolerated.
Meal preparation strategies include batch cooking lean proteins, pre-portioning meals, and keeping emergency bland foods available for high-nausea days. Patients should maintain a food and symptom diary during the first few months to identify personal triggers and optimal eating patterns.
If constipation or diarrhea occurs, adjust fiber types and hydration accordingly, and discuss over-the-counter remedies with your healthcare provider.
Individual nutritional needs vary based on age, sex, activity level, and comorbidities. Patients with diabetes should coordinate meal planning with blood glucose monitoring. Consultation with a registered dietitian familiar with GLP-1/GIP receptor agonist therapy can provide personalized guidance and ensure nutritional adequacy while managing side effects.
High-fat foods should be limited on tirzepatide as they compound the medication's gastric emptying delay, commonly causing prolonged nausea, bloating, and discomfort. Choosing leaner proteins and low-fat cooking methods like baking or grilling typically improves tolerance.
Eating smaller, more frequent meals with bland, easily digestible foods, consuming meals slowly over 20–30 minutes, staying hydrated between meals, and avoiding lying down within two to three hours after eating can significantly reduce nausea severity.
Tirzepatide has no absolute dietary restrictions, but high-fat, fried, spicy, and heavily processed foods commonly worsen gastrointestinal side effects. Individual tolerance varies, and many patients find they can gradually reintroduce foods as their body adjusts to treatment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.