LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Metformin benefits for skin have gained attention as research explores connections between metabolic health and dermatologic conditions. While metformin is FDA-approved only for type 2 diabetes management, emerging evidence suggests it may improve certain skin conditions—particularly in patients with insulin resistance or polycystic ovary syndrome (PCOS). These potential skin improvements appear to result from metformin's effects on insulin levels, androgen production, and inflammation rather than direct dermatologic mechanisms. Understanding when metformin might benefit skin health requires careful consideration of underlying metabolic factors, appropriate patient selection, and physician supervision.
Quick Answer: Metformin may improve certain skin conditions such as acne, acanthosis nigricans, and hirsutism primarily in patients with insulin resistance or PCOS by lowering insulin levels and reducing hyperandrogenism, though it is not FDA-approved for dermatologic use.
Metformin is an oral antihyperglycemic medication primarily prescribed for the management of type 2 diabetes mellitus. As a biguanide, it reduces hepatic glucose production, decreases intestinal glucose absorption, and enhances peripheral insulin sensitivity in muscle and adipose tissue. The FDA approved metformin in 1994, and it remains a commonly used initial pharmacologic agent for glycemic control in adults with type 2 diabetes, though selection depends on comorbidities, cost, and patient factors.
The drug's mechanism of action involves multiple pathways, including suppression of hepatic gluconeogenesis (partly through mitochondrial complex I inhibition), gut-mediated effects, and activation of AMP-activated protein kinase (AMPK), a cellular energy sensor that regulates metabolic pathways. These metabolic changes occur systemically and may affect tissues beyond those directly involved in glucose homeostasis.
Emerging research suggests metformin may exert anti-inflammatory effects and indirectly improve hyperandrogenism by lowering insulin levels. The drug may also affect insulin-like growth factor-1 (IGF-1) levels, which has been hypothesized to influence skin pathology, though evidence remains preliminary. Additionally, metformin's metabolic effects may influence cellular proliferation and sebaceous gland activity, but these mechanisms require further study. It is important to note that metformin is not FDA-approved for any dermatologic indication, and its use for skin conditions remains investigational. Any potential skin benefits observed in clinical practice likely represent secondary effects of its primary metabolic actions rather than direct dermatologic mechanisms.
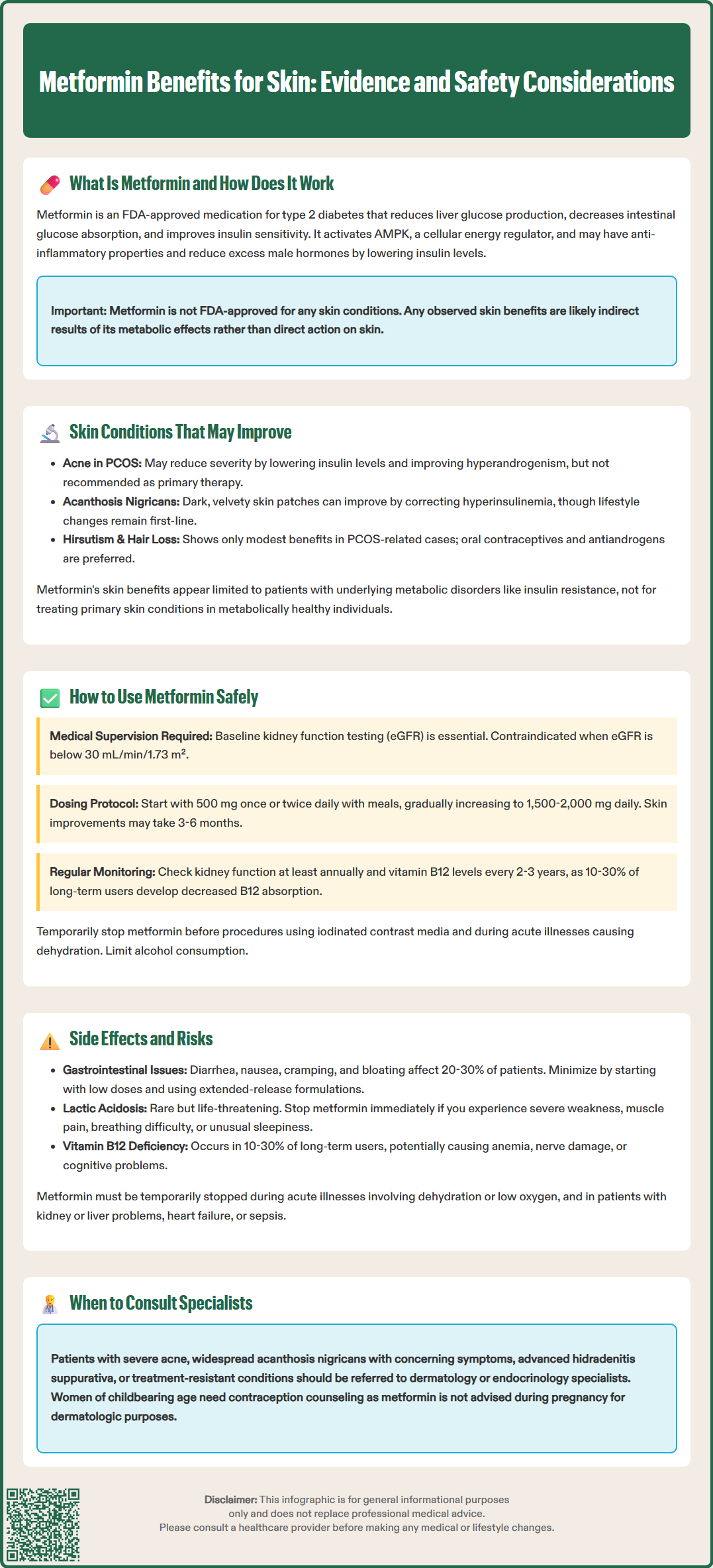
Several dermatologic conditions have been studied in relation to metformin therapy, though the evidence base varies considerably in quality and consistency. The most extensively researched area involves acne vulgaris, particularly in patients with polycystic ovary syndrome (PCOS) and insulin resistance. Observational studies and small clinical trials suggest that metformin may reduce acne severity in women with PCOS through its insulin-lowering effects, which indirectly improve hyperandrogenism. Hyperinsulinemia can stimulate ovarian androgen production and increase bioavailable testosterone, both of which contribute to sebaceous gland hyperactivity and comedone formation. However, metformin is not recommended by American Academy of Dermatology guidelines as primary therapy for acne.
Acanthosis nigricans, characterized by hyperpigmented, velvety plaques typically affecting intertriginous areas, shows a strong association with insulin resistance. Case reports and small case series have documented improvement or resolution of acanthosis nigricans following metformin treatment in patients with underlying metabolic dysfunction. The improvement likely reflects correction of the underlying hyperinsulinemia rather than a direct effect on melanocytes or keratinocytes. Lifestyle intervention remains first-line therapy for this condition.
Hirsutism and androgenetic alopecia (female pattern hair loss) in women with PCOS represent additional conditions where metformin has been investigated, though evidence remains limited. Some studies report modest improvements in hair growth patterns when metformin is used adjunctively with other therapies. The Endocrine Society and ACOG recommend combined oral contraceptives and/or antiandrogens (e.g., spironolactone) as first-line for cutaneous hyperandrogenism in PCOS.
There is preliminary research exploring metformin's potential role in hidradenitis suppurativa, rosacea, and skin aging, but these areas lack robust clinical evidence and are not supported by current guidelines. Importantly, there is no official link established between metformin and treatment of primary dermatologic conditions in patients without metabolic disorders. Dermatologic improvements appear most consistent when metformin addresses underlying insulin resistance or hyperandrogenism rather than acting as a standalone dermatologic agent.
Patients with severe nodulocystic acne, abrupt widespread acanthosis nigricans (especially with weight loss or GI symptoms), hidradenitis suppurativa Hurley stage II-III, or failure of standard therapies should be referred to a dermatologist or endocrinologist for specialized care.
Metformin should only be initiated under physician supervision following appropriate clinical evaluation and laboratory assessment. The drug is not indicated for cosmetic purposes or primary dermatologic treatment in metabolically healthy individuals. Before prescribing metformin, clinicians should assess renal function through estimated glomerular filtration rate (eGFR), as the medication is contraindicated in patients with eGFR below 30 mL/min/1.73 m². Metformin should not be initiated when eGFR is between 30-45 mL/min/1.73 m²; if continued in patients whose eGFR falls into this range, dose reduction (≤1000 mg/day) and close monitoring are recommended. Baseline assessment should also include hepatic function tests and evaluation for conditions that predispose to lactic acidosis.
For patients with documented insulin resistance, PCOS, or prediabetes who may experience dermatologic benefits, typical starting doses range from 500 mg once or twice daily with meals. Prediabetes is defined by the American Diabetes Association as A1C 5.7-6.4%, fasting plasma glucose 100-125 mg/dL, or 2-hour OGTT 140-199 mg/dL. The dose is gradually titrated upward over several weeks to minimize gastrointestinal adverse effects, with maintenance doses typically between 1,500-2,000 mg daily in divided doses. Extended-release formulations may improve tolerability and adherence. Patients should be counseled that any potential skin improvements may take 3-6 months to become apparent, as metabolic and hormonal changes occur gradually.
Regular monitoring is essential during metformin therapy. Renal function should be reassessed at least annually, or more frequently in patients with declining kidney function or those taking concurrent nephrotoxic medications. Vitamin B12 levels warrant periodic evaluation (baseline if risk factors exist, then every 2-3 years, or sooner if anemia or neuropathy develops), as long-term metformin use is associated with decreased B12 absorption in approximately 10-30% of patients.
Patients should be educated about temporarily discontinuing metformin before procedures involving iodinated contrast media. For patients with eGFR 30-60 mL/min/1.73 m² or those receiving intra-arterial contrast, metformin should be held at or just before the procedure and renal function reassessed 48 hours afterward before resuming. Metformin should also be temporarily discontinued during acute illnesses causing dehydration or hemodynamic instability. Patients should limit alcohol consumption due to increased risk of lactic acidosis.
Women of childbearing potential should receive contraception counseling, as metformin for off-label dermatologic use is generally not advised during pregnancy. Any dermatologic use of metformin should involve collaboration between the prescribing physician and dermatologist to ensure appropriate patient selection and monitoring.
Gastrointestinal adverse effects represent the most common tolerability issues with metformin, affecting 20-30% of patients. These include diarrhea, nausea, abdominal cramping, bloating, and metallic taste. Symptoms typically emerge during dose initiation or escalation and often improve with continued use. Starting with low doses, using extended-release formulations, and taking medication with meals can minimize these effects. However, approximately 5% of patients discontinue metformin due to persistent gastrointestinal intolerance despite these strategies.
Lactic acidosis, though rare (estimated incidence <10 cases per 100,000 patient-years according to FDA labeling), represents the most serious potential adverse effect of metformin therapy. This life-threatening complication occurs when lactate accumulates due to impaired clearance or increased production. Risk factors include renal insufficiency, hepatic dysfunction, acute heart failure, sepsis, excessive alcohol consumption, and conditions causing tissue hypoxia. Patients should be counseled to stop metformin and seek immediate medical attention if they develop symptoms such as severe weakness, muscle pain, difficulty breathing, unusual sleepiness, or abdominal distress. Metformin must be temporarily withheld during acute illnesses, particularly those involving dehydration, hypoxemia, or hemodynamic compromise.
Long-term metformin use is associated with vitamin B12 malabsorption, potentially leading to deficiency in 10-30% of patients after several years of therapy. Vitamin B12 deficiency can manifest as megaloblastic anemia, peripheral neuropathy, or cognitive changes. Periodic screening of B12 levels is recommended, particularly in patients with risk factors for deficiency or those on long-term therapy. Supplementation should be considered when levels fall below normal ranges.
Additional considerations include potential drug interactions, particularly with cationic drugs that compete for renal tubular secretion (such as cimetidine), and the need for temporary discontinuation before surgical procedures or radiologic studies with contrast. Rarely, metformin may cause cutaneous adverse reactions such as rash or urticaria.
Patients should be advised to avoid excessive alcohol consumption while taking metformin due to increased risk of lactic acidosis. Those considering metformin primarily for potential dermatologic benefits should carefully weigh these risks against uncertain benefits, particularly if they lack established metabolic indications for the medication. The decision to use metformin should always be individualized based on comprehensive risk-benefit assessment and shared decision-making between patient and physician.
Metformin may improve acne in patients with insulin resistance or PCOS by reducing hyperinsulinemia and androgen levels, but it is not recommended as primary acne therapy and should only be used under physician supervision with appropriate metabolic indications.
Potential skin improvements with metformin typically take 3-6 months to become apparent, as metabolic and hormonal changes occur gradually. Results vary depending on the underlying condition and individual patient factors.
Metformin is not FDA-approved for dermatologic conditions and should only be prescribed when patients have documented metabolic indications such as insulin resistance, PCOS, or prediabetes. Use requires physician supervision, renal function monitoring, and careful risk-benefit assessment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.