LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many people searching for natural forms of semaglutide may be surprised to learn that no such product exists. Semaglutide is a synthetic medication engineered in pharmaceutical laboratories to treat type 2 diabetes and obesity. While the body produces a natural hormone called GLP-1 that semaglutide mimics, the medication itself cannot be found in foods, plants, or dietary supplements. Understanding the difference between prescription semaglutide and natural approaches that support metabolic health is essential for making informed treatment decisions. This article examines what semaglutide is, why natural versions don't exist, and evidence-based alternatives that may support your body's natural GLP-1 activity.
Quick Answer: There are no natural forms of semaglutide because it is a synthetic peptide analog engineered in pharmaceutical laboratories with molecular modifications that cannot occur in nature.
Semaglutide is a prescription medication approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management in adults with obesity or overweight with weight-related comorbidities. It is also approved to reduce the risk of major adverse cardiovascular events in adults with type 2 diabetes and established cardiovascular disease (Ozempic), and in adults with established cardiovascular disease and either obesity or overweight (Wegovy). For weight management, Wegovy is also approved for use in adolescents aged 12 years and older with obesity. Semaglutide is not indicated for type 1 diabetes or diabetic ketoacidosis.
Semaglutide belongs to a class of drugs known as glucagon-like peptide-1 receptor agonists (GLP-1 RAs), which mimic the action of the naturally occurring hormone GLP-1 produced in the intestines.
The mechanism of action of semaglutide involves binding to GLP-1 receptors in multiple tissues throughout the body. In the pancreas, this binding stimulates glucose-dependent insulin secretion from beta cells while suppressing inappropriate glucagon release from alpha cells. This dual action helps regulate blood glucose levels without causing hypoglycemia when glucose levels are normal. Additionally, semaglutide slows gastric emptying, which prolongs the sensation of fullness after meals and reduces appetite through effects on appetite centers in the brain.
Semaglutide is administered as a once-weekly subcutaneous injection (marketed as Ozempic for diabetes and Wegovy for weight management) or as a daily oral tablet (Rybelsus). The medication has a long half-life of approximately one week, allowing for convenient once-weekly dosing of the injectable formulations. Clinical trials have demonstrated significant reductions in hemoglobin A1c levels in patients with type 2 diabetes, as well as substantial weight loss in individuals treated for obesity.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which typically diminish over time with continued use. Semaglutide carries a Boxed Warning for risk of thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), and is contraindicated in patients with a personal or family history of MTC or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Other serious but rare risks include pancreatitis and gallbladder disease.
There are no natural forms of semaglutide available. Semaglutide is a synthetic peptide analog that has been specifically engineered in pharmaceutical laboratories to resist degradation and provide prolonged activity compared to native GLP-1. The molecular structure of semaglutide differs significantly from the naturally occurring GLP-1 hormone, with modifications including amino acid substitutions and the addition of a fatty acid side chain that allows binding to albumin, thereby extending its half-life from minutes to approximately one week.
The term "natural semaglutide" is sometimes used in marketing materials for dietary supplements or alternative health products, but this terminology is misleading and scientifically inaccurate. No plant, food, or naturally occurring substance contains semaglutide or any compound with an identical molecular structure. The production of semaglutide requires sophisticated recombinant DNA technology and chemical modification processes that cannot occur in nature or be replicated through dietary means.
Some online retailers and compounding pharmacies have marketed products claiming to offer "natural" or "bioidentical" versions of semaglutide, but these products are not FDA-approved and may pose significant safety risks. The FDA has issued specific warnings about compounded semaglutide products, particularly those using semaglutide sodium salt, which may contain impurities, incorrect dosages, or entirely different substances than labeled. Compounded semaglutide is only permitted under limited conditions and is not FDA-approved. Additionally, there are no FDA-approved generic versions of semaglutide; products claiming to be generic semaglutide may be counterfeit or mislabeled.
While the body does produce natural GLP-1, this endogenous hormone is rapidly broken down by the enzyme dipeptidyl peptidase-4 (DPP-4) within minutes of secretion, making it unsuitable as a therapeutic agent without pharmaceutical modification. Understanding this distinction is essential for patients considering treatment options for diabetes or weight management.
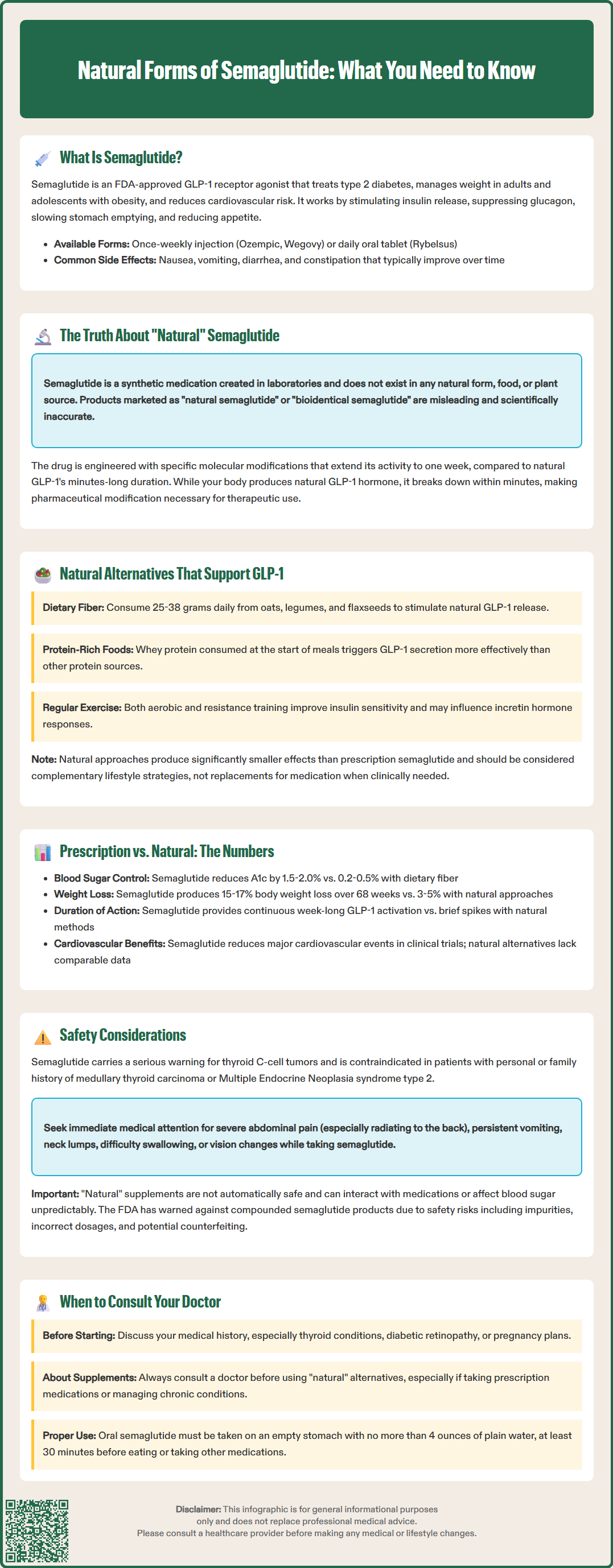
Although there is no natural form of semaglutide, certain dietary approaches, lifestyle modifications, and naturally occurring compounds may support the body's endogenous GLP-1 production or activity. These alternatives work through different mechanisms than prescription semaglutide and typically produce more modest effects on blood glucose control and weight management.
Dietary fiber is one of the most well-studied natural approaches to enhancing GLP-1 secretion. Soluble fiber from sources such as oats, legumes, flaxseeds, and psyllium can stimulate GLP-1 release from intestinal L-cells. The fermentation of fiber by gut bacteria produces short-chain fatty acids, which trigger GLP-1 secretion. Studies suggest that diets high in fiber (25-30 grams daily for women, 30-38 grams for men, per the Institute of Medicine's Dietary Reference Intakes) may modestly increase postprandial GLP-1 levels.
Protein-rich foods also stimulate GLP-1 release, particularly when consumed at the beginning of a meal. Research indicates that whey protein, in particular, may enhance GLP-1 secretion more effectively than other protein sources. The American Diabetes Association recommends individualized macronutrient distribution based on patient preferences and metabolic goals, rather than any specific protein percentage, as part of medical nutrition therapy for diabetes.
Specific nutrients and compounds that have been studied for potential metabolic effects include:
Omega-3 fatty acids from fish oil, which may have metabolic benefits, though evidence specifically for GLP-1 enhancement is limited
Berberine, a plant alkaloid that has shown modest glucose-lowering effects in some small studies, though it may interact with certain medications through CYP enzymes and P-glycoprotein and should be avoided during pregnancy and lactation
Curcumin from turmeric, which has been studied for various metabolic effects, though it may interact with anticoagulants and has limited bioavailability
Green tea catechins, particularly epigallocatechin gallate (EGCG), though concentrated extracts have been associated with rare cases of liver injury
It is important to note that the American Diabetes Association and American College of Physicians do not recommend routine use of dietary supplements for glycemic control due to limited evidence and potential safety concerns.
Physical activity represents another evidence-based approach to supporting metabolic health. Both aerobic exercise and resistance training have been shown to improve insulin sensitivity and may influence incretin hormone responses, though effects on GLP-1 levels specifically are variable across studies.
These natural approaches may provide metabolic benefits, but their effects are generally much smaller in magnitude compared to prescription GLP-1 receptor agonists like semaglutide. They should be viewed as complementary lifestyle strategies rather than direct substitutes for pharmacotherapy when medication is clinically indicated.
The efficacy and clinical outcomes of prescription semaglutide differ substantially from natural alternatives that support GLP-1 activity. Understanding these differences is essential for patients and healthcare providers when making informed treatment decisions.
Efficacy for glycemic control: Clinical trials of semaglutide (SUSTAIN program) have demonstrated hemoglobin A1c reductions of 1.5-2.0% in patients with type 2 diabetes, with many patients achieving A1c levels below 7%. In contrast, dietary fiber supplementation typically produces A1c reductions of 0.2-0.5% in systematic reviews, while berberine studies have shown variable reductions of approximately 0.5-1.0%, though many studies have methodological limitations. The magnitude of glucose-lowering effect with prescription semaglutide is consistently greater and more predictable than with natural alternatives.
Weight loss outcomes: Semaglutide at the doses used for weight management (Wegovy, 2.4 mg weekly) has produced average weight loss of 15-17% of body weight over 68 weeks in clinical trials (STEP program). Natural approaches such as increased dietary fiber, protein optimization, and exercise typically result in weight loss of 3-5% when implemented without additional interventions. While this modest weight loss can provide health benefits, it is substantially less than what is achieved with prescription semaglutide.
Cardiovascular outcomes: Semaglutide has demonstrated significant cardiovascular benefits in large randomized controlled trials. The SUSTAIN-6 trial showed reduced risk of major adverse cardiovascular events in adults with type 2 diabetes and established cardiovascular disease. The SELECT trial demonstrated that semaglutide 2.4 mg weekly reduced cardiovascular events in adults with established cardiovascular disease and either overweight or obesity. Natural alternatives lack comparable cardiovascular outcome data.
Mechanism and duration of action: Prescription semaglutide provides continuous GLP-1 receptor activation throughout the week due to its extended half-life and high receptor binding affinity. Natural approaches that stimulate endogenous GLP-1 release produce transient elevations in GLP-1 levels that are quickly degraded by DPP-4 enzymes. This fundamental difference in pharmacokinetics explains the superior clinical outcomes with prescription medication.
Cost and accessibility: Prescription semaglutide can cost approximately $900-$1,300 per month without insurance coverage, though many insurance plans cover it for FDA-approved indications, and manufacturer assistance programs may be available for eligible patients. Natural alternatives such as dietary modifications and fiber supplements are generally much less expensive but require sustained behavioral changes and may be challenging to maintain long-term.
Evidence base: Semaglutide has been studied in large, randomized controlled trials involving tens of thousands of patients, with well-established safety and efficacy profiles. Many natural alternatives have limited high-quality clinical trial data, particularly regarding long-term outcomes and cardiovascular effects.
Both prescription semaglutide and natural alternatives that affect GLP-1 activity require careful consideration of safety, contraindications, and appropriate medical supervision. Patients should never attempt to self-treat diabetes or obesity without professional guidance.
Contraindications to semaglutide include personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, and previous serious hypersensitivity to semaglutide or any formulation components. The FDA Boxed Warning for thyroid C-cell tumors advises patients to seek immediate medical attention if they experience symptoms such as a lump or swelling in the neck, difficulty swallowing, persistent hoarseness, or shortness of breath. Routine calcitonin monitoring or thyroid ultrasound is not recommended unless clinically indicated.
Caution is advised in patients with a history of pancreatitis, severe gastroparesis, or diabetic retinopathy. Patients with diabetic retinopathy should have appropriate eye evaluations when initiating or intensifying semaglutide therapy, as rapid improvement in glucose control may temporarily worsen retinopathy. Semaglutide is not recommended during pregnancy, and women of childbearing potential should discontinue the medication at least two months before planned conception. The safety of semaglutide during breastfeeding has not been established.
Monitoring requirements: Patients taking prescription semaglutide should monitor blood glucose levels as directed. Renal function should be monitored in patients with renal impairment or when experiencing severe gastrointestinal adverse effects that could lead to dehydration and acute kidney injury. Patients should be monitored for signs of pancreatitis or gallbladder disease.
Administration considerations: Oral semaglutide (Rybelsus) must be taken on an empty stomach with no more than 4 ounces of plain water, at least 30 minutes before the first food, beverage, or other oral medications of the day. Semaglutide should not be used concurrently with other GLP-1 receptor agonists or tirzepatide.
Drug interactions: Semaglutide's effect on gastric emptying may alter the absorption of oral medications, particularly those with narrow therapeutic indices. Dose adjustments of insulin or insulin secretagogues are often necessary to prevent hypoglycemia when initiating semaglutide therapy.
When to consult your doctor:
Before starting any treatment for diabetes or weight management
If experiencing persistent severe nausea, vomiting, or abdominal pain (especially if radiating to the back, which may indicate pancreatitis)
If considering natural supplements, especially if taking prescription medications
Before making significant dietary changes if you have diabetes or other chronic conditions
If natural approaches have not produced adequate glycemic control (A1c >9% or not meeting individualized targets) or weight loss after 3-6 months
If you experience symptoms of hypoglycemia, dehydration, or acute illness
If you develop signs of allergic reaction, including difficulty breathing, rash, or swelling
If you notice changes in vision or have existing diabetic retinopathy
Patients should be aware that "natural" does not automatically mean safe. Some herbal supplements and natural products can interact with medications, affect blood glucose levels unpredictably, or contain contaminants. The American College of Physicians and American Diabetes Association emphasize that treatment decisions should be individualized based on patient preferences, comorbidities, and clinical circumstances, with shared decision-making between patients and healthcare providers. Self-treatment with unregulated products marketed as natural alternatives to prescription medications may delay appropriate medical care and potentially cause harm.
No, semaglutide cannot be obtained from foods or supplements because it is a synthetic medication created through pharmaceutical engineering. While your body produces natural GLP-1 hormone, this is chemically different from semaglutide and breaks down within minutes.
Dietary fiber from sources like oats and legumes, protein-rich foods, and regular physical activity may support your body's natural GLP-1 production. However, these approaches produce much smaller metabolic effects compared to prescription semaglutide and should not be considered direct substitutes when medication is clinically indicated.
There are no FDA-approved generic versions of semaglutide, and the FDA has issued warnings about compounded semaglutide products that may contain impurities, incorrect dosages, or different substances than labeled. Only FDA-approved semaglutide products (Ozempic, Wegovy, Rybelsus) have established safety and efficacy profiles.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.