LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide after gastric sleeve surgery represents an emerging approach for patients experiencing inadequate weight loss or weight regain following bariatric surgery. While gastric sleeve surgery removes approximately 80% of the stomach to restrict food intake and alter gut hormones, some patients may benefit from additional medical therapy. Semaglutide, a GLP-1 receptor agonist approved by the FDA for type 2 diabetes (Ozempic) and chronic weight management (Wegovy), works through mechanisms that overlap with the physiological changes produced by sleeve gastrectomy. This off-label combination requires careful clinical evaluation, individualized timing, and close monitoring to optimize metabolic outcomes while managing potential risks in patients with altered gastrointestinal anatomy.
Quick Answer: Semaglutide may be used off-label after gastric sleeve surgery to address inadequate weight loss or weight regain, though this requires careful clinical evaluation and monitoring.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Ozempic) and chronic weight management (Wegovy) in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with weight-related comorbidities. Wegovy is also approved for weight management in adolescents ≥12 years with obesity. Gastric sleeve surgery, or sleeve gastrectomy, is a bariatric procedure that removes approximately 80% of the stomach, creating a tubular gastric pouch that restricts food intake and alters gut hormone secretion.
The intersection of pharmacotherapy and bariatric surgery represents an evolving area in obesity medicine. Some patients who undergo gastric sleeve surgery may experience inadequate weight loss (defined as less than 50% excess weight loss), weight regain after initial success, or persistent metabolic conditions such as type 2 diabetes. In these scenarios, clinicians may consider adjunctive medical therapy with agents like semaglutide to optimize metabolic outcomes.
Both gastric sleeve surgery and semaglutide influence similar physiological pathways, including GLP-1 signaling, gastric emptying, and appetite regulation. The gastric sleeve procedure naturally increases endogenous GLP-1 levels by accelerating nutrient delivery to the distal small intestine. Semaglutide mimics and potentially amplifies this effect through exogenous GLP-1 receptor activation, though the precise interaction between these mechanisms in post-bariatric patients requires further study.
Importantly, there is no FDA indication specifically for semaglutide use after bariatric surgery, making this an off-label application. The different semaglutide formulations (Wegovy, Ozempic, Rybelsus) are not interchangeable, with Wegovy specifically indicated and dosed for chronic weight management. Clinical practice in this area is guided by emerging evidence, expert consensus, and individualized patient assessment. Clinicians must carefully evaluate the appropriateness of semaglutide therapy in the post-bariatric population, considering both potential benefits and safety considerations unique to patients with altered gastrointestinal anatomy.
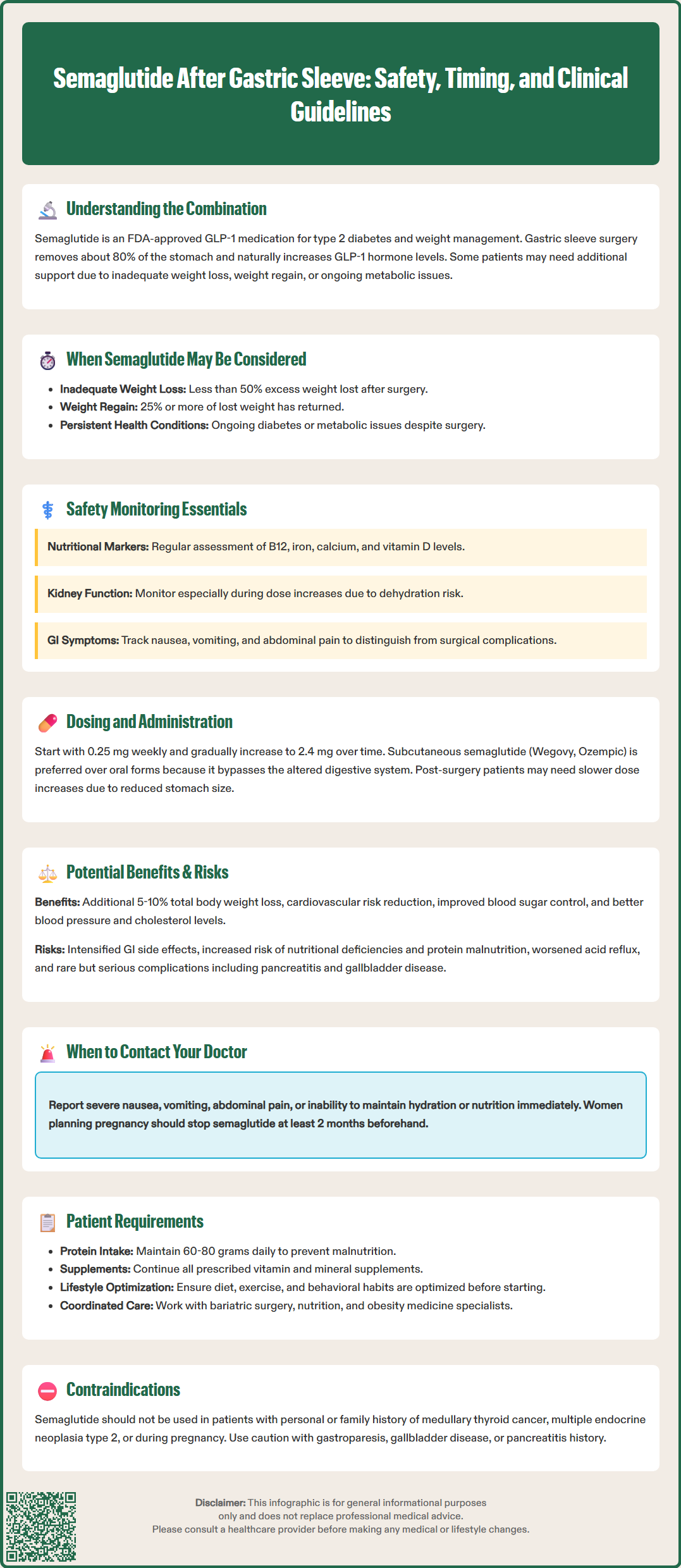
The timing of semaglutide initiation after gastric sleeve surgery requires careful clinical judgment. While no definitive guidelines specify an optimal timeframe, many clinicians consider initiating pharmacotherapy when patients experience weight loss plateau or documented weight regain. This individualized approach often involves allowing adequate time for postoperative healing, nutritional stabilization, and assessment of surgical weight loss outcomes before introducing additional weight loss interventions.
Safety considerations in post-bariatric patients center on gastrointestinal tolerability and nutritional status. Semaglutide's mechanism of action includes delayed gastric emptying and reduced appetite, which may compound the restrictive effects of sleeve gastrectomy. Patients may experience enhanced gastrointestinal adverse effects, including nausea, vomiting, abdominal pain, and constipation—symptoms that overlap with potential postoperative complications. Clinicians must differentiate between medication side effects and surgical complications such as stricture, obstruction, or gastroesophageal reflux disease.
Nutritional monitoring becomes particularly important when combining semaglutide with prior bariatric surgery. Post-sleeve patients already face increased risks of protein malnutrition, vitamin deficiencies (particularly B12, iron, calcium, and vitamin D), and inadequate caloric intake. The appetite-suppressing effects of semaglutide may further compromise nutritional intake, necessitating close monitoring of nutritional markers, body composition, and supplementation adherence. Persistent vomiting requires prompt evaluation for thiamine deficiency and supplementation when indicated.
Key safety monitoring parameters include:
Baseline and periodic assessment of nutritional status (complete blood count, comprehensive metabolic panel, vitamin levels, albumin)
Renal function monitoring, particularly during dose escalation, due to risk of acute kidney injury from dehydration
Evaluation for gastrointestinal symptoms and differentiation from surgical complications
Monitoring for gallbladder disease, which may be increased with weight loss and semaglutide use
Assessment of medication adherence and injection technique
Eye examination in patients with diabetes due to potential risk of diabetic retinopathy progression with rapid glycemic improvement
Regular follow-up with both bariatric surgery and endocrinology or obesity medicine teams when possible
Patients should be counseled to report severe or persistent nausea, vomiting, abdominal pain, or inability to maintain adequate hydration or nutrition, as these may warrant dose adjustment, temporary discontinuation, or further evaluation for surgical complications. Women of childbearing potential should be advised that semaglutide should be discontinued at least 2 months before a planned pregnancy.
Semaglutide functions as a long-acting GLP-1 receptor agonist with 94% homology to native human GLP-1. Its mechanism of action involves binding to GLP-1 receptors in multiple tissues, including pancreatic beta cells, the gastrointestinal tract, and central nervous system appetite centers. The medication enhances glucose-dependent insulin secretion, suppresses inappropriate glucagon release, delays gastric emptying, and reduces appetite through hypothalamic pathways—particularly in the arcuate nucleus and paraventricular nucleus.
In patients who have undergone gastric sleeve surgery, the physiological landscape is already altered in ways that overlap with semaglutide's effects. Sleeve gastrectomy increases endogenous GLP-1 secretion through accelerated nutrient transit to L-cells in the distal ileum and colon, which produce GLP-1 in response to nutrient exposure. This enhanced incretin effect contributes significantly to the metabolic benefits observed after bariatric surgery, including improved glycemic control independent of weight loss.
When semaglutide is introduced after gastric sleeve surgery, it provides supraphysiologic GLP-1 receptor activation that exceeds the endogenous incretin response generated by the altered anatomy. This may theoretically produce additive effects on weight loss and metabolic parameters, though this interaction has not been extensively studied in controlled trials. The medication's central appetite-suppressing effects complement the mechanical restriction and hormonal changes from surgery, potentially addressing weight regain driven by increased caloric intake or adaptation to the surgical restriction.
The pharmacokinetics of semaglutide in post-bariatric patients have not been extensively studied, but the subcutaneous route of administration (Wegovy, Ozempic) bypasses the altered gastrointestinal anatomy, suggesting that absorption should remain consistent with non-surgical populations. Oral semaglutide (Rybelsus) may have less predictable absorption in patients with altered gastrointestinal anatomy and is generally not preferred in this population. The medication's long half-life (approximately one week) allows for once-weekly dosing with subcutaneous formulations, which may improve adherence in patients managing multiple postoperative medications and supplements. However, the pharmacodynamic effects—particularly on gastric emptying and appetite—may be different in patients with reduced gastric capacity, potentially requiring more cautious dose titration than in bariatric-naive patients.
The potential benefits of adding semaglutide after gastric sleeve surgery primarily address inadequate weight loss or weight regain, which affects approximately 15-30% of bariatric surgery patients. Emerging evidence, primarily from observational and retrospective studies, suggests that GLP-1 receptor agonists may produce additional weight loss in post-bariatric patients. Some studies report mean additional weight loss of 5-10% of total body weight, though the quality of evidence remains limited. For patients experiencing weight regain or plateau, this additional weight reduction may help achieve or maintain clinically meaningful weight loss thresholds associated with improved cardiometabolic outcomes.
Metabolic benefits beyond weight loss represent another potential advantage. Semaglutide has demonstrated cardiovascular benefits in clinical trials, including reduction in major adverse cardiovascular events. The SELECT trial showed that semaglutide 2.4 mg (Wegovy) reduces cardiovascular risk in adults with established cardiovascular disease and either overweight or obesity, leading to an FDA-approved indication for reducing cardiovascular risk in this population. For post-bariatric patients with persistent or recurrent type 2 diabetes, semaglutide may provide enhanced glycemic control and potential cardiovascular risk reduction. Additionally, improvements in blood pressure, lipid profiles, and markers of hepatic steatosis have been observed with semaglutide therapy.
Potential benefits include:
Additional weight loss in cases of inadequate surgical response or weight regain
Enhanced glycemic control for persistent or recurrent type 2 diabetes
Cardiovascular risk reduction in appropriate patients
Improvement in obesity-related comorbidities (hypertension, dyslipidemia, sleep apnea)
Non-invasive intervention avoiding revision surgery
However, the combined approach carries specific risks that warrant careful consideration. Gastrointestinal adverse effects may be more pronounced or poorly tolerated in post-surgical patients with altered anatomy. The risk of nutritional deficiencies may be amplified by further appetite suppression and reduced food intake. There is theoretical concern about exacerbating gastroesophageal reflux disease, which can be problematic after sleeve gastrectomy due to increased intragastric pressure and loss of the gastric fundus.
Potential risks include:
Enhanced gastrointestinal side effects (nausea, vomiting, diarrhea, constipation)
Increased risk of nutritional deficiencies and protein malnutrition
Potential worsening of gastroesophageal reflux symptoms
Dehydration risk and acute kidney injury, particularly during dose escalation
Increased risk of gallbladder disease and complications
Risk of intestinal obstruction or ileus
Diabetic retinopathy progression in patients with diabetes, particularly with rapid glycemic improvement
Hypoglycemia risk, particularly in patients on insulin or sulfonylureas
Cost considerations and insurance coverage challenges
Rare but serious risks including pancreatitis and thyroid C-cell tumors (boxed warning)
Clinicians must engage in shared decision-making with patients, carefully weighing these potential benefits against risks in the context of individual patient circumstances, surgical outcomes, comorbidities, and treatment goals.
Currently, there are no specific FDA-approved indications or comprehensive clinical guidelines exclusively addressing semaglutide use after bariatric surgery. However, clinical practice can be informed by general obesity medicine principles, bariatric surgery guidelines, and emerging expert consensus. The American Society for Metabolic and Bariatric Surgery (ASMBS) and other professional organizations recognize that adjunctive medical therapy may be appropriate for post-bariatric patients with inadequate weight loss or weight regain, though specific medication recommendations continue to evolve.
Candidate selection for semaglutide after gastric sleeve surgery should be individualized and based on clear clinical indications. Appropriate candidates typically include patients who have achieved postoperative stability, demonstrate inadequate weight loss (less than 50% excess weight loss) or significant weight regain (typically defined as regaining 25% or more of lost weight), and have persistent obesity-related comorbidities despite surgical intervention. Patients should have optimized behavioral factors, including dietary adherence, physical activity, and psychological support, as medication is not a substitute for lifestyle modification.
Clinical approach considerations:
Patient selection: Stable post-surgical patients with inadequate weight loss, weight regain, or persistent metabolic disease
Timing: Individualized based on weight trajectory and metabolic status, often when weight loss plateaus or regain is documented
Baseline evaluation: Comprehensive metabolic panel, nutritional markers (vitamin B12, iron studies, vitamin D, calcium, albumin), HbA1c if diabetic, lipid panel, assessment of gastrointestinal symptoms, renal function
Dosing strategy: For Wegovy, initiate at 0.25 mg weekly with gradual titration (0.25→0.5→1.0→1.7→2.4 mg); consider slower titration if gastrointestinal symptoms are problematic
Monitoring frequency: More frequent follow-up than in bariatric-naive patients, particularly during dose escalation (every 4-6 weeks initially)
Nutritional support: Continued emphasis on protein intake (60-80 grams daily), vitamin/mineral supplementation, and adequate hydration
Multidisciplinary coordination: Collaboration between bariatric surgery, endocrinology/obesity medicine, nutrition, and behavioral health providers
Contraindications to semaglutide use include personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, prior serious hypersensitivity to semaglutide or its components, and pregnancy. Semaglutide is not indicated for type 1 diabetes management. Women planning pregnancy should discontinue semaglutide at least 2 months before conception. Relative contraindications or situations requiring heightened caution include severe gastroparesis, active gallbladder disease, history of pancreatitis, severe gastrointestinal disease, diabetic retinopathy, and inadequate nutritional status.
Patients should receive comprehensive counseling about realistic expectations, potential side effects, the importance of continued lifestyle modification, and the need for ongoing nutritional monitoring. They should understand that semaglutide is typically a long-term therapy, and discontinuation may result in weight regain. Insurance coverage can be challenging, and patients should be informed about potential costs and prior authorization requirements. Referral back to the bariatric surgery team is appropriate if concerning gastrointestinal symptoms develop, if nutritional parameters deteriorate despite intervention, or if there is consideration of revision surgery as an alternative approach.
The timing of semaglutide initiation after gastric sleeve surgery is individualized and typically considered when patients experience weight loss plateau or documented weight regain after adequate postoperative healing and nutritional stabilization. Many clinicians allow time to assess surgical weight loss outcomes before introducing additional pharmacotherapy.
Semaglutide can be used after bariatric surgery with careful monitoring, though it carries specific risks including enhanced gastrointestinal side effects, increased nutritional deficiency risk, and potential complications from delayed gastric emptying. Close monitoring of nutritional status, renal function, and gastrointestinal symptoms is essential in post-bariatric patients.
Potential benefits include additional weight loss in cases of inadequate surgical response or weight regain, enhanced glycemic control for persistent type 2 diabetes, cardiovascular risk reduction in appropriate patients, and improvement in obesity-related comorbidities without requiring revision surgery. Emerging evidence suggests possible additional weight loss, though high-quality controlled trials are limited.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.