LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

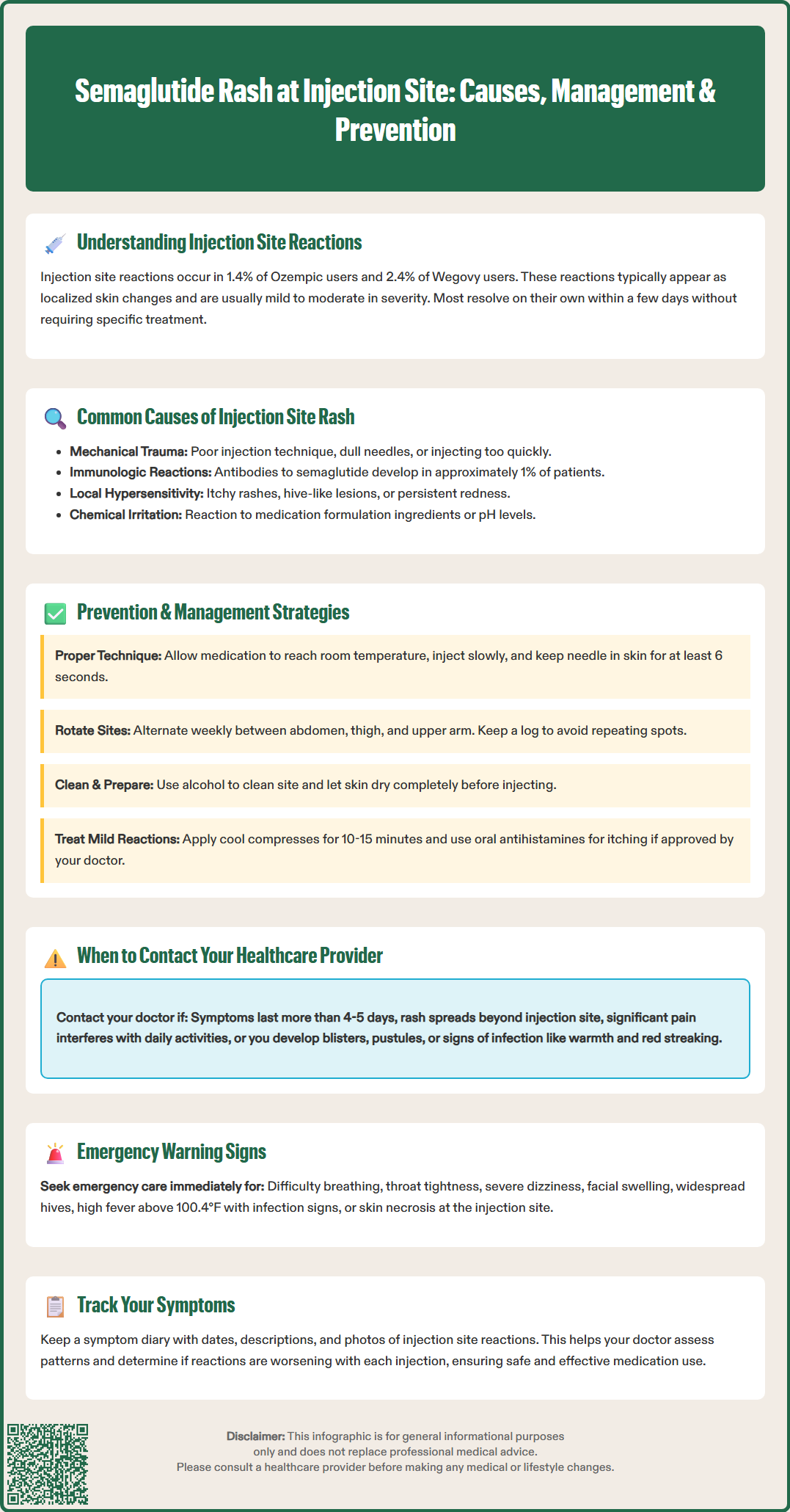
Semaglutide injection site rash affects approximately 1.4% to 2.4% of patients using this GLP-1 receptor agonist for type 2 diabetes or weight management. While most injection site reactions are mild and self-limiting, understanding their causes, symptoms, and management is essential for safe medication use. This article examines why rashes occur at semaglutide injection sites, how to distinguish benign reactions from those requiring medical attention, and evidence-based strategies for prevention and treatment. Proper injection technique, systematic site rotation, and recognizing warning signs can minimize discomfort and support successful therapy outcomes.
Quick Answer: Semaglutide injection site rash occurs in 1.4% to 2.4% of patients and typically presents as mild, self-limiting erythema or swelling that resolves within 2 to 4 days without treatment.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand name Ozempic) and chronic weight management (as Wegovy). Administered as a once-weekly subcutaneous injection, semaglutide works by enhancing glucose-dependent insulin secretion, suppressing glucagon release, and slowing gastric emptying. While the medication has demonstrated significant efficacy in glycemic control and weight reduction, patients may experience local injection site reactions, though these are less common than gastrointestinal adverse effects.
According to FDA prescribing information, injection site reactions occur in approximately 1.4% of patients using Ozempic and 2.4% of patients using Wegovy. These reactions typically manifest as localized skin changes at or near the injection site and are generally mild to moderate in severity.
Most injection site reactions with semaglutide are self-limiting and resolve without specific intervention within a few days. However, understanding the nature of these reactions, their potential causes, and appropriate management strategies is essential for both healthcare providers and patients. Proper injection technique, site rotation, and recognition of warning signs that warrant medical evaluation can help minimize discomfort and ensure safe, effective use of semaglutide therapy. Patient education regarding expected versus concerning symptoms plays a crucial role in medication adherence and overall treatment success.
Injection site rashes associated with semaglutide can result from several distinct mechanisms. Understanding these underlying causes helps differentiate between benign, self-resolving reactions and those requiring clinical intervention.
Mechanical trauma and local irritation represent the most common cause of injection site reactions. The physical act of needle insertion creates minor tissue trauma, which triggers a localized inflammatory response. This mechanical irritation may be exacerbated by improper injection technique, including injecting too rapidly, using a dull needle, or failing to allow the medication to reach room temperature before administration. The subcutaneous tissue responds with increased blood flow, mild edema, and sometimes visible erythema or a raised area at the injection site.
Immunologic reactions to semaglutide or formulation excipients constitute another potential mechanism. While true allergic reactions to semaglutide are rare, the medication can stimulate antibody formation in some patients. According to FDA prescribing information, anti-semaglutide antibodies develop in approximately 1% of patients using injectable semaglutide. Most of these antibodies do not appear to affect clinical efficacy or safety. Local hypersensitivity reactions may manifest as pruritic rashes, urticaria-like lesions, or persistent erythema extending beyond the immediate injection site.
Chemical irritation from the medication formulation itself may contribute to localized skin reactions. Semaglutide injection solutions contain various excipients that can occasionally cause contact dermatitis or irritant reactions in susceptible individuals. The pH and osmolality of the solution may also contribute to transient discomfort or visible skin changes following injection.
Injection site reactions with semaglutide present with varying characteristics and severity. Recognizing the spectrum of symptoms helps patients distinguish between expected, minor reactions and those warranting medical evaluation.
Common, typically benign symptoms include:
Mild erythema (redness) at the injection site, usually less than 2 inches in diameter
Slight swelling or a small raised area that feels firm to touch
Transient tenderness or mild discomfort lasting 1 to 3 days
Minimal itching without spreading or worsening
Small bruising (ecchymosis) at the puncture site
These reactions generally appear within minutes to hours after injection and typically resolve spontaneously within 2 to 4 days without treatment. They do not typically interfere with daily activities or indicate a serious problem.
Symptoms requiring healthcare provider contact include:
Rash or erythema spreading beyond the injection site or appearing at distant body locations
Persistent or worsening symptoms lasting more than 4 to 5 days
Significant pain that interferes with movement or daily function
Development of pustules, blisters, or skin breakdown
Warmth, increasing redness, or red streaking extending from the injection site (potential cellulitis)
Fever, chills, or systemic symptoms accompanying local reactions
Recurrent severe reactions at multiple injection sites
Signs of possible allergic reaction, including hives, facial swelling, or difficulty breathing
Call 911 or seek emergency care immediately for signs of severe allergic reaction such as difficulty breathing, throat tightness, severe dizziness, or widespread hives.
Patients should maintain a symptom diary documenting the timing, appearance, and duration of injection site reactions. Photographs can be helpful for clinical assessment, particularly when symptoms have resolved by the time of the healthcare visit. Any pattern of progressively worsening reactions with subsequent injections warrants prompt medical evaluation.
Effective management and prevention of semaglutide injection site reactions involve both proper injection technique and appropriate symptomatic care when reactions occur.
Preventive strategies focus on optimizing injection practices:
Proper injection technique is fundamental. Follow the specific Instructions for Use for your medication:
For Ozempic: Allow the pen to reach room temperature before injection. Inject slowly and hold the needle in the skin for at least 6 seconds after the dose counter shows 0 to ensure complete delivery.
For Wegovy: Follow the autoinjector instructions, pressing and holding until the yellow bar fully appears/indicator stops moving (typically about 10 seconds).
Site rotation is essential for preventing cumulative tissue trauma and irritation. Semaglutide can be injected into the abdomen, thigh, or upper arm. Rotate injection sites with each weekly dose, avoiding injecting into the same exact spot. Maintaining a written or digital log of injection sites helps ensure systematic rotation.
Skin preparation should include cleaning the injection site with an alcohol swab and allowing the skin to dry completely before injection. Injecting through wet alcohol can introduce irritants into the subcutaneous tissue. Patients should avoid areas with active skin conditions, scars, moles, or recent sunburn.
Symptomatic management for mild injection site reactions includes:
Applying a cool compress or ice pack wrapped in a thin cloth for 10 to 15 minutes to reduce swelling and discomfort
Avoiding rubbing or massaging the injection site, which may increase irritation
Using over-the-counter oral antihistamines (such as cetirizine or loratadine) for itching, if approved by a healthcare provider
Applying fragrance-free, hypoallergenic moisturizer to dry or irritated skin around (not directly on) the injection site
Patients should consult their healthcare provider before applying topical medications to injection sites, as these may mask signs of infection. For persistent allergic-type reactions, your healthcare provider may recommend a short course of low-potency topical corticosteroids.
While most semaglutide injection site reactions are benign and self-limiting, certain presentations require prompt medical evaluation to rule out complications or hypersensitivity reactions.
Immediate medical attention (emergency department or urgent care) is warranted for:
Signs of anaphylaxis or severe allergic reaction, including difficulty breathing, throat tightness, rapid pulse, dizziness, or widespread urticaria (call 911)
Severe swelling extending beyond the injection site or involving the face, lips, or tongue
Signs of significant infection, including fever above 100.4°F (38°C), purulent drainage, or rapidly spreading erythema with warmth
Severe pain disproportionate to visible findings
Skin necrosis, blistering, or ulceration at the injection site
Scheduled healthcare provider evaluation is appropriate for:
Persistent injection site reactions lasting more than 5 to 7 days despite conservative management
Recurrent moderate to severe reactions with each injection, suggesting possible hypersensitivity
Development of indurated nodules or lipohypertrophy at injection sites
Uncertainty about whether symptoms represent normal reactions or require intervention
Clinical assessment of concerning injection site reactions typically includes examination of the affected area, review of injection technique, and evaluation for signs of infection or hypersensitivity. Healthcare providers may consider:
Bacterial culture if infection is suspected
Temporary discontinuation of semaglutide to assess symptom resolution
Referral to allergy/immunology for suspected hypersensitivity reactions
For type 2 diabetes patients only, alternative GLP-1 receptor agonist formulations (such as oral semaglutide/Rybelsus) if injection site reactions are recurrent and problematic
Patients with confirmed hypersensitivity to semaglutide should not continue the medication. The FDA label lists hypersensitivity to semaglutide or any formulation excipients as a contraindication. Additionally, semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Healthcare providers should document all significant injection site reactions in the medical record and report serious adverse events to the FDA MedWatch program. Patient education emphasizing the distinction between expected minor reactions and warning signs requiring medical attention supports safe, effective semaglutide therapy.
Most semaglutide injection site rashes are mild and resolve spontaneously within 2 to 4 days without treatment. If symptoms persist beyond 5 to 7 days or worsen, contact your healthcare provider for evaluation.
Mild, localized rashes that resolve within a few days typically do not require discontinuation. However, recurrent severe reactions, spreading rash, or signs of allergic reaction warrant immediate medical evaluation and may require stopping the medication.
Systematic site rotation with each weekly injection, proper injection technique including allowing medication to reach room temperature, and thorough skin preparation with alcohol swabs are the most effective prevention strategies for minimizing injection site reactions.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.