LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
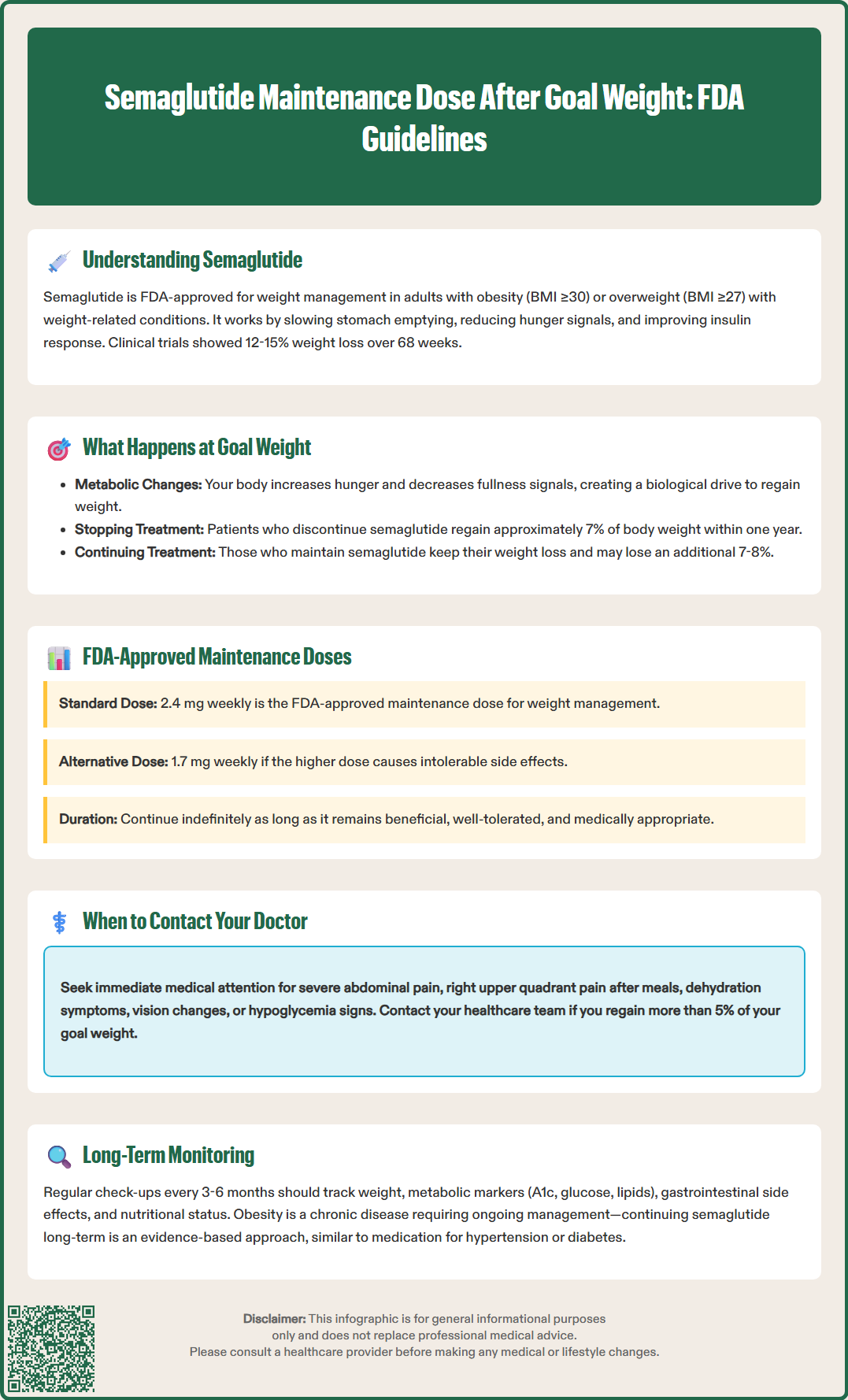
Semaglutide maintenance dose after goal weight is a critical consideration for patients who have successfully achieved their weight loss targets. Reaching your goal weight on semaglutide marks a transition from active weight loss to weight maintenance—a phase that requires continued medical management to prevent regain. Clinical evidence demonstrates that discontinuing semaglutide after weight loss leads to significant weight regain, while maintaining therapy helps sustain results. The FDA-approved maintenance dose is 2.4 mg weekly, with 1.7 mg weekly as an alternative if the higher dose isn't tolerated. Understanding your maintenance strategy is essential for long-term success.
Quick Answer: The FDA-approved semaglutide maintenance dose after reaching goal weight is 2.4 mg once weekly, with 1.7 mg weekly as an alternative if the higher dose is not tolerated.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. It's also approved for weight management in adolescents aged 12 years and older with obesity. While originally developed for type 2 diabetes management under the brand name Ozempic, a higher-dose formulation marketed as Wegovy received FDA approval specifically for weight management in 2021.
The medication works through multiple mechanisms to promote weight reduction. Semaglutide slows gastric emptying, which prolongs the sensation of fullness after meals. It also acts on appetite centers in the hypothalamus to reduce hunger signals and food cravings. Additionally, semaglutide increases glucose-dependent insulin secretion, suppresses glucagon, and may contribute to metabolic improvements beyond weight loss alone.
Clinical trials have demonstrated substantial weight loss with semaglutide therapy. The STEP (Semaglutide Treatment Effect in People with obesity) trial program showed that participants using semaglutide 2.4 mg weekly achieved an average weight loss of 12-15% of their initial body weight over 68 weeks, compared to 2-3% with placebo. These results represent some of the most significant weight reductions achieved with pharmacotherapy to date.
Semaglutide is administered as a once-weekly subcutaneous injection, typically starting at a low dose of 0.25 mg and gradually escalating over 16-20 weeks to the target maintenance dose of 2.4 mg weekly for weight management. If the 2.4 mg dose is not tolerated, 1.7 mg weekly is an FDA-approved maintenance alternative. This gradual titration helps minimize gastrointestinal side effects such as nausea, vomiting, and diarrhea, which are the most commonly reported adverse effects during the initial treatment phase. If doses are missed for more than 2 weeks, re-titration is recommended per FDA labeling.
Reaching your goal weight while taking semaglutide represents a significant achievement, but it also marks a critical transition point in your treatment journey. Many patients and healthcare providers face uncertainty about the appropriate next steps once weight loss targets have been met. Understanding what happens physiologically and clinically at this juncture is essential for long-term success.
When you achieve your target weight, your body has undergone substantial metabolic adaptations. Weight loss triggers compensatory mechanisms that increase hunger hormones like ghrelin and decrease satiety signals, creating a biological drive to regain lost weight. Research indicates that these metabolic adaptations can persist for years after weight loss, making weight maintenance particularly challenging without continued intervention.
Clinical evidence from the STEP trials provides important insights into what occurs when semaglutide is discontinued after weight loss. In the STEP 4 trial, participants who achieved significant weight loss on semaglutide 2.4 mg were randomized to either continue the medication or switch to placebo. Those who discontinued semaglutide regained approximately 7% of their body weight within one year, while those who continued the medication maintained their weight loss and even experienced modest additional reductions (approximately 7-8% further loss).
These findings suggest that semaglutide addresses an ongoing physiological need rather than providing a temporary fix. The medication appears to counteract the metabolic adaptations that promote weight regain, potentially affecting what some researchers hypothesize as the body's defended weight. For most patients, reaching goal weight does not signal the end of treatment but rather a transition from the weight loss phase to the weight maintenance phase, which typically requires continued pharmacological support for optimal outcomes as long as benefits outweigh risks.
Determining the appropriate maintenance dose of semaglutide after achieving your goal weight requires individualized assessment and should be guided by your healthcare provider. According to FDA labeling, the standard maintenance dose for weight management is semaglutide 2.4 mg administered once weekly, with 1.7 mg weekly as an approved alternative if the higher dose is not tolerated.
US clinical guidelines from organizations such as the American Diabetes Association (ADA), American Gastroenterological Association (AGA), and Endocrine Society recommend continuing effective anti-obesity medication therapy as long as it remains beneficial, well-tolerated, and medically appropriate. The FDA label also provides guidance on when to consider discontinuation: if a patient has not lost at least 5% of their initial body weight after 12 weeks on the 2.4 mg dose, stopping treatment may be appropriate as further benefits are unlikely.
Factors that influence maintenance dose decisions include:
Degree of weight loss achieved: Patients who have lost substantial weight (>15% of initial body weight) may require full-dose therapy to counteract stronger biological drives toward weight regain.
Tolerability and side effects: Persistent gastrointestinal symptoms or other adverse effects may warrant using the FDA-approved alternative maintenance dose of 1.7 mg weekly.
Metabolic improvements: Patients who have achieved resolution of comorbidities such as prediabetes or hypertension may have different risk-benefit considerations.
Weight stability: Some patients maintain stable weight on lower doses, though systematic evidence for doses below 1.7 mg remains limited.
Some clinicians have explored maintaining patients on 1.0 mg weekly after goal weight achievement, particularly for those experiencing persistent side effects. However, this approach is considered off-label for weight management and should be approached with caution. Any dose adjustment should be made gradually and accompanied by enhanced lifestyle interventions and frequent follow-up.
Importantly, semaglutide should be discontinued at least 2 months before a planned pregnancy and is not recommended during pregnancy or breastfeeding. It should also be used with caution in patients with severe gastroparesis.
Long-term continuation of semaglutide after achieving goal weight is supported by both clinical trial data and our understanding of obesity as a chronic disease requiring ongoing management. The current evidence suggests that sustained pharmacotherapy is necessary for most patients to maintain weight loss and prevent the metabolic adaptations that drive weight regain.
The STEP 4 trial provides compelling evidence for continued use. Participants who maintained semaglutide therapy after initial weight loss sustained their improvements over an additional 48 weeks, while those switched to placebo experienced significant weight regain. This pattern mirrors findings from studies of other weight loss interventions, including bariatric surgery, where ongoing support and intervention are critical for maintaining results.
Long-term safety data for semaglutide comes from diabetes trials lasting approximately 2 years and the SELECT cardiovascular outcomes trial with median follow-up of about 3.3 years. The weight management formulation demonstrates a generally favorable safety profile. The most common adverse effects—nausea, diarrhea, vomiting, and constipation—typically diminish over time as patients acclimate to the medication.
Important safety considerations for long-term use include:
Regular monitoring for gastrointestinal symptoms and appropriate management strategies
Awareness of signs of pancreatitis (severe abdominal pain radiating to the back); if suspected or confirmed, discontinue semaglutide and do not restart
Monitoring for gallbladder disease, particularly in patients with rapid weight loss
Risk of diabetic retinopathy complications in patients with type 2 diabetes
Potential for acute kidney injury, especially with dehydration from gastrointestinal side effects
Rare but serious hypersensitivity reactions including anaphylaxis
Contraindication in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2
Not recommended during pregnancy or breastfeeding; discontinue at least 2 months before planned pregnancy
Patients should understand that obesity is a chronic condition with biological underpinnings that persist after weight loss. Continuing semaglutide is not a sign of failure but rather an evidence-based approach to managing a chronic disease, similar to ongoing treatment for hypertension or diabetes.
Effective long-term management with semaglutide requires ongoing collaboration with your healthcare provider through regular monitoring and dose optimization. After reaching your goal weight, the frequency and focus of clinical follow-up should shift from weight loss tracking to comprehensive maintenance monitoring.
Recommended monitoring parameters include:
Weight measurements: Monthly or quarterly weight checks to detect early signs of regain (typically defined as >3-5% increase from goal weight)
Metabolic markers: Periodic assessment of hemoglobin A1c, fasting glucose, and lipid panels to track metabolic health improvements
Gastrointestinal tolerance: Ongoing evaluation of side effects and their impact on quality of life and nutritional status
Nutritional status: Assessment for adequate protein intake and nutritional adequacy based on dietary patterns
Kidney function: Monitoring when clinically indicated, especially with significant gastrointestinal symptoms or dehydration
Retinopathy screening: Regular ophthalmology follow-up for patients with type 2 diabetes
Mental health: Screening for mood changes, as weight loss may affect mental health in some individuals
Your healthcare provider should conduct comprehensive reviews at least every 3-6 months during the maintenance phase. These visits provide opportunities to assess whether your current dose remains appropriate, evaluate for any emerging safety concerns, and reinforce lifestyle modifications that complement pharmacotherapy.
Dose adjustments during maintenance should be approached cautiously and systematically. If dose reduction is considered due to side effects, the FDA-approved alternative maintenance dose of 1.7 mg weekly may be appropriate. If doses are missed for more than 2 weeks, re-titration according to the FDA-approved schedule is recommended to minimize side effects.
If you're taking insulin or sulfonylureas along with semaglutide, your provider may need to reduce these medications' doses to prevent hypoglycemia, especially during dose escalation.
Situations requiring prompt medical attention include:
Severe or persistent abdominal pain (possible pancreatitis)
Signs of gallbladder disease (right upper quadrant pain, especially after meals)
Symptoms of dehydration or kidney problems (decreased urination, swelling)
Severe or persistent gastrointestinal symptoms affecting nutrition or hydration
Changes in vision or symptoms of hypoglycemia (if taking other diabetes medications)
Significant weight regain (>5% of goal weight) should prompt timely contact with your healthcare team, though it's not a medical emergency.
Patients should maintain open communication with their healthcare team about challenges, side effects, and goals. Successful long-term weight maintenance with semaglutide requires not only appropriate dosing but also continued attention to nutrition, physical activity, sleep, and stress management as part of a comprehensive approach to metabolic health.
Clinical evidence shows that discontinuing semaglutide after weight loss leads to significant weight regain (approximately 7% within one year). Most patients require continued therapy to maintain weight loss and counteract metabolic adaptations that promote regain.
The FDA-approved maintenance doses for weight management are 2.4 mg weekly (standard) or 1.7 mg weekly (alternative if higher dose not tolerated). Lower doses are considered off-label and lack systematic evidence for weight maintenance.
Comprehensive healthcare provider reviews should occur at least every 3-6 months during maintenance, with monitoring of weight, metabolic markers, gastrointestinal tolerance, nutritional status, and safety parameters including kidney function and retinopathy screening for patients with diabetes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.