LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Side effects of GLP-1 probiotics are primarily gastrointestinal and typically mild, resembling those of conventional probiotic supplements. These emerging dietary supplements contain bacterial strains—commonly Lactobacillus and Bifidobacterium species—marketed to support metabolic health by potentially influencing natural GLP-1 production. Unlike FDA-approved GLP-1 receptor agonists such as semaglutide or tirzepatide, these products are regulated as dietary supplements, not medications. Most users experience bloating, gas, or temporary digestive changes during the initial adjustment period. While generally safe for healthy individuals, certain populations—including immunocompromised patients and premature infants—face elevated risks. Understanding the side effect profile and appropriate usage guidelines helps consumers make informed decisions about these supplements.
Quick Answer: GLP-1 probiotics typically cause mild gastrointestinal side effects such as bloating, gas, and temporary digestive changes, though serious risks exist for immunocompromised individuals.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
GLP-1 probiotics represent an emerging category of dietary supplements marketed to support metabolic health by potentially influencing glucagon-like peptide-1 (GLP-1) production in the gut. Unlike prescription GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro for type 2 diabetes, Zepbound for obesity)—which is actually a dual GIP/GLP-1 receptor agonist—these probiotic formulations contain specific bacterial strains, most commonly Lactobacillus and Bifidobacterium species, that manufacturers claim may stimulate endogenous GLP-1 secretion from intestinal L-cells.
The proposed mechanism centers on the gut microbiome's role in metabolic regulation. Certain probiotic strains may produce short-chain fatty acids (SCFAs) through fermentation of dietary fiber, which can theoretically activate receptors on enteroendocrine cells to trigger GLP-1 release. However, it is essential to understand that these supplements are not pharmaceutical agents and are not FDA-approved for treating diabetes or obesity. Under the Dietary Supplement Health and Education Act (DSHEA), these products are regulated as foods, not medications, and manufacturers cannot legally claim they treat, cure, or prevent disease.
GLP-1 is an incretin hormone that enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and promotes satiety. While prescription GLP-1 agonists deliver pharmacologic doses that produce measurable clinical effects, the magnitude of GLP-1 elevation from probiotic supplements—if any—is substantially lower and clinically uncertain. The American Diabetes Association does not recommend probiotics or other dietary supplements for glycemic control due to insufficient evidence.
Consumers should recognize that "GLP-1 probiotic" is primarily a marketing term rather than a distinct therapeutic class, and these products function fundamentally as probiotics with theoretical metabolic benefits that require further validation through rigorous clinical research.
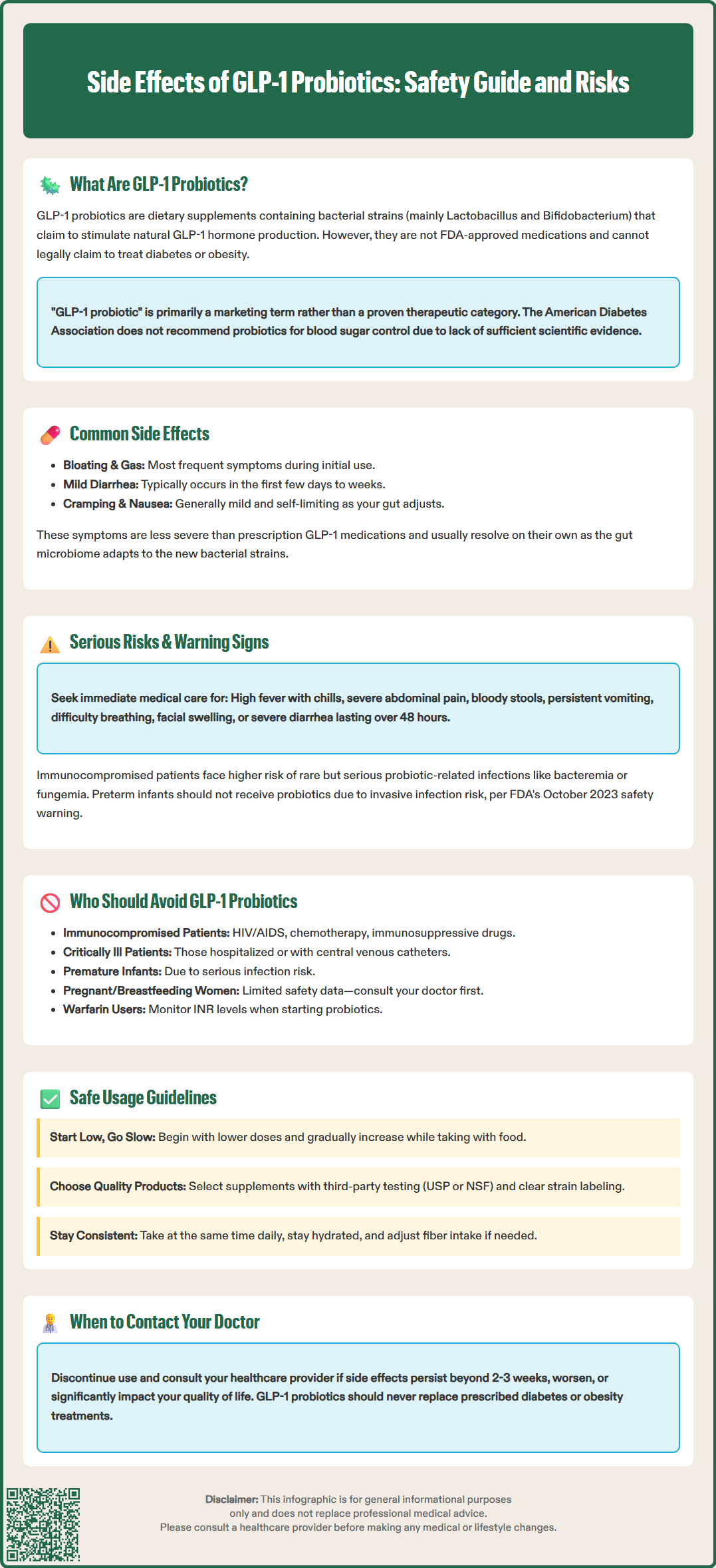
The side effect profile of GLP-1 probiotics generally mirrors that of conventional probiotic supplements, as the bacterial strains used are similar to those in standard formulations. The most frequently reported adverse effects involve gastrointestinal symptoms, which typically emerge during the initial days to weeks of supplementation as the gut microbiome adjusts to the introduced bacterial strains.
Common gastrointestinal effects include:
Bloating and gas: Increased fermentation activity from probiotic bacteria can produce excess intestinal gas, causing abdominal distension and discomfort
Mild diarrhea or loose stools: Changes in gut flora composition may temporarily alter bowel habits
Abdominal cramping: Some individuals experience mild to moderate cramping as their digestive system adapts
Nausea: Less common but reported, particularly when supplements are taken on an empty stomach
These symptoms are generally mild, self-limiting, and often resolve within days to weeks as the microbiome equilibrates. The duration and severity vary considerably between individuals. Unlike prescription GLP-1 receptor agonists, which commonly cause significant nausea, vomiting, and gastrointestinal distress due to delayed gastric emptying, probiotic-related symptoms are typically less severe and mechanistically different.
Some users report headaches or fatigue during the adjustment period, though there is limited evidence establishing a causal relationship between these symptoms and probiotic use. Allergic reactions to probiotic ingredients (such as dairy-derived components in certain formulations) may occur in sensitive individuals.
It is important to note that the side effect profile can vary considerably depending on the specific bacterial strains, colony-forming unit (CFU) count, and additional ingredients in the formulation. Yeast-based probiotics (such as Saccharomyces boulardii) may have different side effect profiles compared to bacterial probiotics. Individuals with underlying gastrointestinal conditions may experience more pronounced symptoms and should consult healthcare providers before initiating supplementation.
While probiotics are generally considered safe for healthy individuals, serious adverse events can occur in specific populations, and certain symptoms warrant immediate medical evaluation. The most significant concern involves systemic infection (bacteremia or fungemia) in immunocompromised patients, though this remains rare with quality-controlled products.
Seek immediate medical attention if you experience:
High fever (temperature >101°F/38.3°C) with chills, which may indicate systemic infection
Severe abdominal pain that is persistent, worsening, or accompanied by rigidity
Bloody or black tarry stools, suggesting gastrointestinal bleeding
Persistent vomiting that prevents adequate hydration
Signs of allergic reaction: difficulty breathing, facial swelling, hives, or throat tightness
Severe diarrhea lasting more than 48 hours or signs of dehydration (decreased urination, dizziness, extreme thirst)
Patients with compromised immune systems—including those with HIV/AIDS, active cancer treatment, organ transplant recipients, or those taking immunosuppressive medications—face elevated risk of probiotic-related infections. Case reports have documented Lactobacillus bacteremia and Saccharomyces fungemia in vulnerable populations, with the latter particularly associated with central venous catheter use, though incidence remains extremely low.
The FDA issued a safety communication in October 2023 warning against the use of probiotic products in preterm infants due to the risk of invasive infection. Preterm infants should not receive probiotics unless specifically directed by neonatologists in controlled clinical protocols.
Individuals with central venous catheters, recent gastrointestinal surgery, or intestinal damage may experience bacterial translocation across compromised mucosal barriers. Additionally, patients with short bowel syndrome may experience small intestinal bacterial overgrowth (SIBO), potentially worsening symptoms.
If you develop new or worsening symptoms after starting GLP-1 probiotics, discontinue use and consult your healthcare provider. This is especially important for individuals with diabetes, as any supplement claiming metabolic effects requires medical oversight to ensure it does not interfere with established treatment regimens or mask concerning symptoms requiring evaluation. Serious adverse events should be reported to the FDA's MedWatch program.
Certain populations should avoid GLP-1 probiotic supplements or use them only under close medical supervision due to elevated risk of adverse outcomes. The decision to avoid these products should be individualized based on comprehensive medical history and current health status.
Individuals who should avoid or exercise extreme caution include:
Immunocompromised patients: Those with primary immunodeficiency disorders, HIV/AIDS with low CD4 counts, active chemotherapy recipients, or individuals taking immunosuppressive medications (corticosteroids, biologics, transplant drugs) face increased infection risk
Critically ill or hospitalized patients: Severely ill individuals, particularly those in intensive care settings or with compromised gut barrier function, should not receive probiotics outside controlled clinical protocols
Patients with central venous catheters: Indwelling lines provide potential routes for bacterial translocation into the bloodstream
Premature infants: The FDA issued a safety warning in October 2023 against using probiotics in preterm infants due to risk of invasive infection
Patients with severe acute pancreatitis: Clinical guidelines from the American College of Gastroenterology recommend against probiotic use in this condition due to potential harm
Additional populations requiring medical consultation:
Pregnant and breastfeeding women should consult healthcare providers before using GLP-1 probiotics, as safety data in these populations remains limited. Individuals with active gastrointestinal conditions—including inflammatory bowel disease (Crohn's disease, ulcerative colitis)—should seek medical advice and follow American Gastroenterological Association guidance regarding strain-specific, condition-specific probiotic use.
Patients with known allergies to probiotic ingredients, including dairy proteins or specific bacterial strains, should carefully review product labels. Those taking warfarin should exercise caution and monitor INR levels when starting or stopping probiotics, as some bacterial strains might theoretically affect vitamin K production, though evidence is limited and this concern does not apply to direct oral anticoagulants (DOACs). Anyone with diabetes should discuss probiotic use with their healthcare provider, as the American Diabetes Association does not recommend supplements for glycemic control due to insufficient evidence.
Minimizing side effects from GLP-1 probiotics requires thoughtful implementation strategies and realistic expectations about these supplements' capabilities and limitations. Most adverse effects can be mitigated through gradual introduction and attention to timing and dosage.
Strategies to reduce side effects:
Start with lower doses: Begin with a reduced amount and gradually increase as tolerated, allowing your gut microbiome to adapt
Take with food: Consuming probiotics with meals may reduce gastrointestinal discomfort and improve bacterial survival through the acidic stomach environment
Stay hydrated: Maintain adequate fluid intake unless you have a medical condition requiring fluid restriction (consult your healthcare provider for personalized guidance)
Maintain consistent timing: Taking supplements at the same time daily promotes microbiome stability
Monitor fiber intake: Excessive dietary fiber combined with probiotics may amplify gas and bloating; adjust fiber consumption if symptoms are bothersome
Safe usage guidelines:
Choose products from reputable manufacturers that provide third-party testing verification (such as USP or NSF certification), clearly list bacterial strains and CFU counts, and follow FDA current Good Manufacturing Practices (cGMP). Store probiotics according to package instructions—many require refrigeration to maintain bacterial viability. Check expiration dates, as potency diminishes over time.
Understand that GLP-1 probiotics are dietary supplements regulated under the Dietary Supplement Health and Education Act (DSHEA). They are not FDA-approved for treating diabetes or obesity and are not substitutes for prescription medications or evidence-based lifestyle interventions for metabolic health. There is no established therapeutic dose, and claims about metabolic benefits lack robust clinical validation.
If you have diabetes, continue all prescribed medications and monitoring protocols; do not adjust treatment based on probiotic use without physician guidance. If side effects persist beyond 2-3 weeks, worsen over time, or significantly impact quality of life, discontinue the supplement and consult your healthcare provider. Document any adverse effects, including timing, severity, and associated factors, to facilitate clinical assessment. Report serious adverse events to the FDA's MedWatch program.
Approach GLP-1 probiotic claims with appropriate skepticism, prioritizing evidence-based interventions for metabolic health management.
No, GLP-1 probiotics are dietary supplements containing bacterial strains that may theoretically influence natural GLP-1 production, while prescription GLP-1 medications like semaglutide are FDA-approved drugs that deliver pharmacologic doses with proven clinical effects for diabetes and obesity.
Most gastrointestinal side effects such as bloating and gas are mild and self-limiting, typically resolving within days to weeks as the gut microbiome adjusts to the introduced bacterial strains.
Immunocompromised patients, premature infants, critically ill individuals, those with central venous catheters, and patients with severe acute pancreatitis should avoid GLP-1 probiotics due to elevated risk of serious infections and adverse outcomes.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.