LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro, Zepbound) is a dual GIP and GLP-1 receptor agonist FDA-approved for type 2 diabetes and chronic weight management. While gastric sleeve surgery effectively treats severe obesity, some patients experience weight regain or plateau before reaching their goals. In these cases, clinicians may consider tirzepatide as adjunctive therapy. This represents an emerging, off-label application requiring careful evaluation of surgical history, metabolic status, and nutritional adequacy. Understanding the safety profile, timing considerations, and monitoring requirements helps patients and providers make informed decisions about combining pharmacotherapy with bariatric surgery outcomes.
Quick Answer: Tirzepatide may be considered off-label after gastric sleeve surgery for patients experiencing weight regain or persistent diabetes, though this use lacks extensive clinical trial data and requires careful monitoring.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m², or ≥27 kg/m² with at least one weight-related comorbidity. While gastric sleeve surgery (sleeve gastrectomy) remains one of the most effective interventions for severe obesity, some patients experience weight regain or fail to achieve their target weight loss goals. In these situations, clinicians may consider adjunctive pharmacotherapy to optimize metabolic outcomes.
The use of tirzepatide after gastric sleeve represents an emerging area of clinical practice, though it is not yet extensively studied in large-scale trials. Bariatric surgery alters gastrointestinal anatomy and physiology, which can affect medication tolerability and efficacy, though tirzepatide's subcutaneous administration bypasses concerns about altered GI absorption. The gastric sleeve procedure removes approximately 80% of the stomach, creating a tubular structure that reduces gastric capacity and modifies gut hormone secretion. This anatomical change shares some mechanistic overlap with GLP-1-based therapies, as both influence satiety signaling and glucose homeostasis.
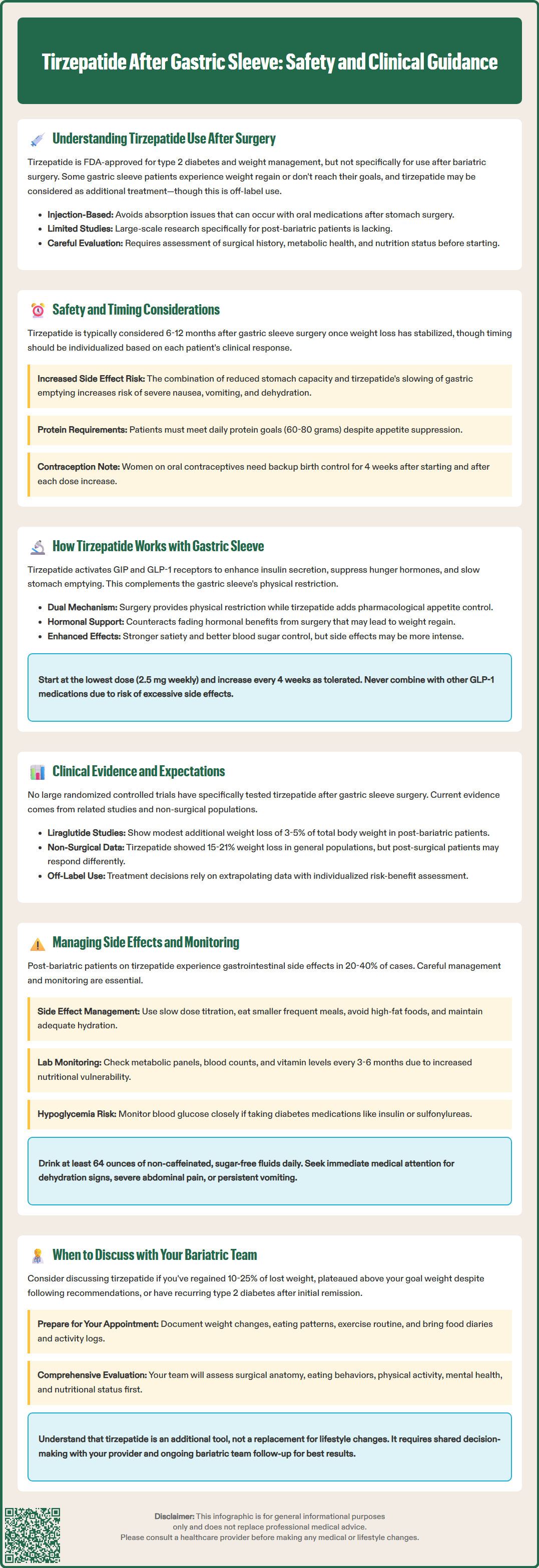
The timing of tirzepatide initiation after gastric sleeve surgery requires careful clinical consideration. While no standardized protocol exists, many clinicians assess patients once their post-surgical weight loss has stabilized, often 6-12 months after surgery, though timing should be individualized based on clinical response and metabolic needs.
Safety considerations are paramount in this population. Post-bariatric patients already experience reduced gastric capacity and altered gastric emptying, which tirzepatide further modifies through its GLP-1 receptor agonism. This dual effect on gastric motility may increase the risk of gastrointestinal adverse effects, including nausea, vomiting, and early satiety. Severe nausea and vomiting in post-sleeve patients can lead to dehydration, electrolyte disturbances, and inadequate nutritional intake, potentially compromising protein and micronutrient status.
Patients who have experienced surgical complications such as strictures, gastroesophageal reflux disease (GERD), or peptic/staple-line ulcers require particularly cautious evaluation. Tirzepatide's effect on gastric emptying could theoretically exacerbate reflux symptoms or complicate stricture management. Additionally, the medication's appetite-suppressing effects may make it challenging for patients to meet their protein requirements (typically 60-80 grams daily post-bariatric surgery) and maintain adequate hydration.
Important FDA-labeled safety warnings include risk of pancreatitis, gallbladder disease, and acute kidney injury with dehydration. Patients with diabetes should be aware of potential diabetic retinopathy complications with rapid glycemic improvement. Women using oral contraceptives should use alternative or back-up contraception for 4 weeks after tirzepatide initiation and after each dose increase due to potential reduced effectiveness from delayed gastric emptying.
Before initiating tirzepatide, clinicians should document baseline nutritional status, including complete blood count, comprehensive metabolic panel, calcium, vitamin B12, folate, iron studies, and vitamin D levels. Patients should demonstrate stable weight, adequate protein intake, and compliance with vitamin supplementation. Those with active nutritional deficiencies should have these corrected before starting therapy.
Tirzepatide's dual agonist mechanism offers complementary effects to the physiological changes induced by gastric sleeve surgery. The medication activates both GIP and GLP-1 receptors, enhancing glucose-dependent insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. These effects align with but extend beyond the hormonal changes that occur after sleeve gastrectomy.
Gastric sleeve surgery itself produces significant alterations in gut hormone profiles. The procedure reduces ghrelin production (the primary hunger hormone), increases postprandial GLP-1 secretion, and improves insulin sensitivity through weight loss and direct metabolic effects. However, these hormonal changes may diminish over time, contributing to weight regain in some patients. Tirzepatide may help sustain or amplify these beneficial hormonal signals, particularly in patients experiencing metabolic adaptation or hormonal normalization years after surgery.
The synergistic potential lies in addressing different aspects of weight regulation. While the sleeve provides mechanical restriction and baseline hormonal modification, tirzepatide adds pharmacological enhancement of satiety signaling and glucose metabolism. This combination may be particularly valuable for patients who have reached a weight loss plateau despite good surgical anatomy, or those with persistent insulin resistance and type 2 diabetes despite significant weight loss.
Clinically, patients using tirzepatide after gastric sleeve may experience enhanced satiety, reduced food cravings, and improved glycemic control. However, the overlapping mechanisms also mean that side effects related to delayed gastric emptying and reduced appetite may be more pronounced. Careful dose titration is essential, starting with the lowest available dose (2.5 mg weekly) for initiation only, with increases every 4 weeks as tolerated to reach therapeutic doses per FDA labeling. Tirzepatide should not be co-administered with other GLP-1 receptor agonists due to overlapping mechanisms and potential for additive adverse effects.
The evidence base for GLP-1 receptor agonists and dual agonists after bariatric surgery is evolving but remains limited compared to their use in non-surgical populations. Most published data involve earlier-generation GLP-1 agonists such as liraglutide, with emerging case series and small studies examining semaglutide and tirzepatide in post-bariatric patients. No large randomized controlled trials have specifically evaluated tirzepatide after gastric sleeve surgery, though clinical experience is accumulating.
Studies of liraglutide in post-bariatric patients have demonstrated modest additional weight loss (typically 3-5% of total body weight) when initiated for weight regain after surgery. These findings established proof of concept that pharmacotherapy can provide meaningful benefit in the post-surgical population. Semaglutide, a more potent GLP-1 agonist, has shown greater weight loss efficacy in general populations and appears promising in preliminary post-bariatric reports, though published data remain sparse.
In separate clinical trials of non-surgical populations, tirzepatide (SURMOUNT program) and semaglutide (STEP trials) have both demonstrated significant weight loss efficacy. The SURMOUNT-1 trial showed mean weight loss of 15-21% in non-surgical patients, depending on dose. However, direct comparisons between these trials should be interpreted cautiously due to differences in study design and populations. Whether similar efficacy translates to post-surgical populations remains uncertain, as these patients have different baseline physiology and may respond differently to incretin-based therapies.
Current clinical practice relies on extrapolation from general population data and individualized risk-benefit assessment. The American Society for Metabolic and Bariatric Surgery (ASMBS) acknowledges that pharmacotherapy may be appropriate for post-surgical weight regain but emphasizes the importance of comprehensive evaluation, behavioral intervention, and nutritional optimization before medication initiation. Clinicians should counsel patients that evidence specific to tirzepatide after gastric sleeve is limited, and treatment represents off-label use in this context.
Post-bariatric patients initiating tirzepatide require enhanced monitoring protocols due to their unique physiological status and increased vulnerability to certain adverse effects. The most common side effects of tirzepatide—nausea, vomiting, diarrhea, constipation, and abdominal discomfort—occur in 20-40% of patients in clinical trials. These gastrointestinal effects may be more pronounced or problematic in post-sleeve patients who already experience altered gastric function.
Nausea management strategies include slow dose titration (remaining at each dose level for at least four weeks), eating smaller and more frequent meals, avoiding high-fat foods, and ensuring adequate hydration. Unlike oral medications, the timing of subcutaneous tirzepatide injections relative to meals does not affect absorption or efficacy. Anti-emetic medications such as ondansetron may provide symptomatic relief but should not mask concerning symptoms that warrant medical evaluation. Persistent severe nausea, vomiting, or abdominal pain requires prompt assessment to rule out surgical complications such as stricture or severe GERD, or medication-related issues like pancreatitis.
Nutritional monitoring becomes even more critical when combining surgical and pharmacological interventions. Patients should undergo laboratory assessment every 3-6 months, including complete metabolic panel, complete blood count, calcium, iron studies, vitamin B12, folate, 25-hydroxyvitamin D, and parathyroid hormone. Protein intake monitoring through dietary recall or food diaries helps ensure patients meet their elevated protein requirements despite reduced appetite. Some patients may require protein supplementation or temporary dose reduction if intake becomes inadequate.
Hypoglycemia risk, while generally low with tirzepatide monotherapy, increases in patients taking concurrent diabetes medications, particularly insulin or sulfonylureas. Post-bariatric patients with diabetes may experience improved glycemic control requiring medication adjustment. Blood glucose monitoring and proactive medication titration prevent hypoglycemic episodes. Patients should be educated on hypoglycemia recognition and management.
Patients should be monitored for signs of pancreatitis (severe abdominal pain, sometimes radiating to the back, with or without vomiting), gallbladder disease, and acute kidney injury, especially with dehydration. Those with diabetic retinopathy should have appropriate ophthalmologic monitoring. Dehydration represents a significant concern, as both gastric sleeve anatomy and tirzepatide-induced nausea can reduce fluid intake. Patients should aim for at least 64 ounces of non-caffeinated, sugar-free fluids daily, sipping slowly throughout the day. Signs of dehydration warrant immediate medical attention and may require intravenous fluid administration.
Patients should initiate conversations about tirzepatide with their bariatric surgery team when experiencing specific clinical scenarios that may warrant additional intervention. Weight regain after bariatric surgery lacks standardized definitions, but is often described as regaining 10-25% or more of lost weight after reaching nadir weight. Earlier intervention may be appropriate for patients who plateau significantly above their goal weight despite optimal adherence to dietary and exercise recommendations.
Persistent or recurrent type 2 diabetes after initial post-surgical remission provides another compelling reason to discuss tirzepatide. Many patients achieve diabetes remission following gastric sleeve surgery, though recurrence rates vary by procedure, patient factors, and follow-up duration. According to American Diabetes Association Standards of Care, medication intensification should be considered when glycemic targets (typically A1c <7% for most patients) are not achieved with metformin and lifestyle measures. Tirzepatide's dual mechanism offers both glycemic control and weight management benefits, potentially addressing both concerns simultaneously.
The discussion should occur within the context of comprehensive bariatric follow-up, not as a replacement for it. Before considering medication, the bariatric team will typically assess several factors: surgical anatomy integrity (via upper gastrointestinal imaging if indicated), dietary adherence and eating behaviors, physical activity patterns, psychological factors including eating disorders or depression, and nutritional status. Addressing modifiable factors such as grazing behavior, liquid calorie consumption, or sedentary lifestyle may obviate the need for medication in some cases.
Patients should prepare for the discussion by documenting their weight trajectory, current eating patterns, exercise routine, and any symptoms or concerns. Bringing food diaries, activity logs, and home blood glucose records (if diabetic) provides valuable information for clinical decision-making. The discussion should include contraindications, potential insurance coverage and cost considerations, and for women of reproductive age, contraception plans given tirzepatide's interaction with oral contraceptives.
Ultimately, the decision to use tirzepatide after gastric sleeve requires shared decision-making between patient and provider, weighing potential benefits against risks, costs, and the limited evidence base specific to this population. Patients should understand that medication represents an adjunct to, not a replacement for, the lifestyle modifications and behavioral changes essential for long-term bariatric success. Regular follow-up with the bariatric team ensures coordinated care and optimal outcomes.
Most clinicians consider tirzepatide 6-12 months after gastric sleeve surgery once post-surgical weight loss has stabilized, though timing should be individualized based on your metabolic response, nutritional status, and clinical needs. Your bariatric team will assess surgical outcomes and ensure nutritional adequacy before initiating therapy.
No, tirzepatide does not have specific FDA indication for post-bariatric surgery use, making this an off-label application. However, it may be prescribed if you meet standard criteria for obesity or diabetes management (BMI ≥30 kg/m² or ≥27 kg/m² with comorbidities, or type 2 diabetes).
The primary concerns include enhanced gastrointestinal side effects (nausea, vomiting) due to overlapping effects on gastric emptying, potential difficulty meeting protein requirements, dehydration risk, and nutritional deficiencies. Close monitoring of nutritional status and hydration is essential, with laboratory assessment every 3-6 months.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.