LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide and beta blockers are frequently prescribed together for patients managing both type 2 diabetes and cardiovascular conditions. Tirzepatide, a dual GIP/GLP-1 receptor agonist marketed as Mounjaro and Zepbound, improves glycemic control and promotes weight loss. Beta blockers treat hypertension, heart failure, and arrhythmias by reducing heart rate and blood pressure. Since cardiovascular disease is the leading cause of death in people with diabetes, many patients require both medications. While no absolute contraindication exists for their combined use, understanding potential pharmacodynamic interactions—particularly regarding hypoglycemia recognition and heart rate effects—is essential for safe, effective therapy under medical supervision.
Quick Answer: Tirzepatide can generally be taken safely with beta blockers, as there is no absolute contraindication to their combined use.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management), tirzepatide works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite. Clinical trials have demonstrated significant reductions in hemoglobin A1c levels and substantial weight loss, making it an important therapeutic option for patients with metabolic conditions.
Importantly, tirzepatide carries a boxed warning for thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Beta blockers, also known as beta-adrenergic blocking agents, represent a diverse class of cardiovascular medications that block the effects of epinephrine (adrenaline) on beta-adrenergic receptors. These medications are commonly prescribed for hypertension, heart failure, coronary artery disease, arrhythmias, and occasionally for specific situations like performance anxiety (often off-label). Common examples include metoprolol, atenolol, carvedilol, and propranolol. Beta blockers work by reducing heart rate, decreasing myocardial contractility, and lowering blood pressure, thereby reducing cardiac workload and oxygen demand.
Many patients with type 2 diabetes also have cardiovascular comorbidities requiring beta blocker therapy. According to the American Diabetes Association, cardiovascular disease remains the leading cause of morbidity and mortality in individuals with diabetes. Consequently, the concurrent use of tirzepatide and beta blockers is increasingly common in clinical practice. Understanding the pharmacological profiles of both medication classes is essential for safe and effective management of patients requiring combination therapy for their metabolic and cardiovascular conditions.
Yes, tirzepatide can generally be taken with beta blockers, and there is no absolute contraindication to their combined use. The FDA-approved prescribing information for tirzepatide (Mounjaro and Zepbound) does not list beta blockers as medications that cannot be used concurrently. Many patients with type 2 diabetes have coexisting cardiovascular conditions that necessitate beta blocker therapy, and clinical experience supports the safety of using these medications together under appropriate medical supervision.
It's important to note that while beta blockers and tirzepatide can be used together, other contraindications for tirzepatide still apply, including personal or family history of MTC or MEN2, and pregnancy risk.
The pharmacokinetic profiles of tirzepatide and beta blockers suggest minimal direct drug-drug interactions. Tirzepatide is administered subcutaneously once weekly and is primarily eliminated through proteolytic degradation, with minimal renal excretion of intact drug. Beta blockers, depending on the specific agent, are metabolized hepatically (lipophilic agents like metoprolol and carvedilol) or excreted renally unchanged (hydrophilic agents like atenolol). These distinct metabolic pathways reduce the likelihood of competitive inhibition or altered clearance when used together.
However, combined use requires clinical awareness of potential pharmacodynamic considerations rather than direct pharmacokinetic interactions. Both medication classes can influence cardiovascular parameters and glucose metabolism in ways that may require monitoring and dose adjustments. The decision to use tirzepatide and beta blockers together should be individualized based on the patient's complete medical profile, including their cardiovascular status, glycemic control, renal function, and overall treatment goals. Healthcare providers routinely manage patients on both medications, but appropriate monitoring and patient education remain essential components of safe combination therapy.
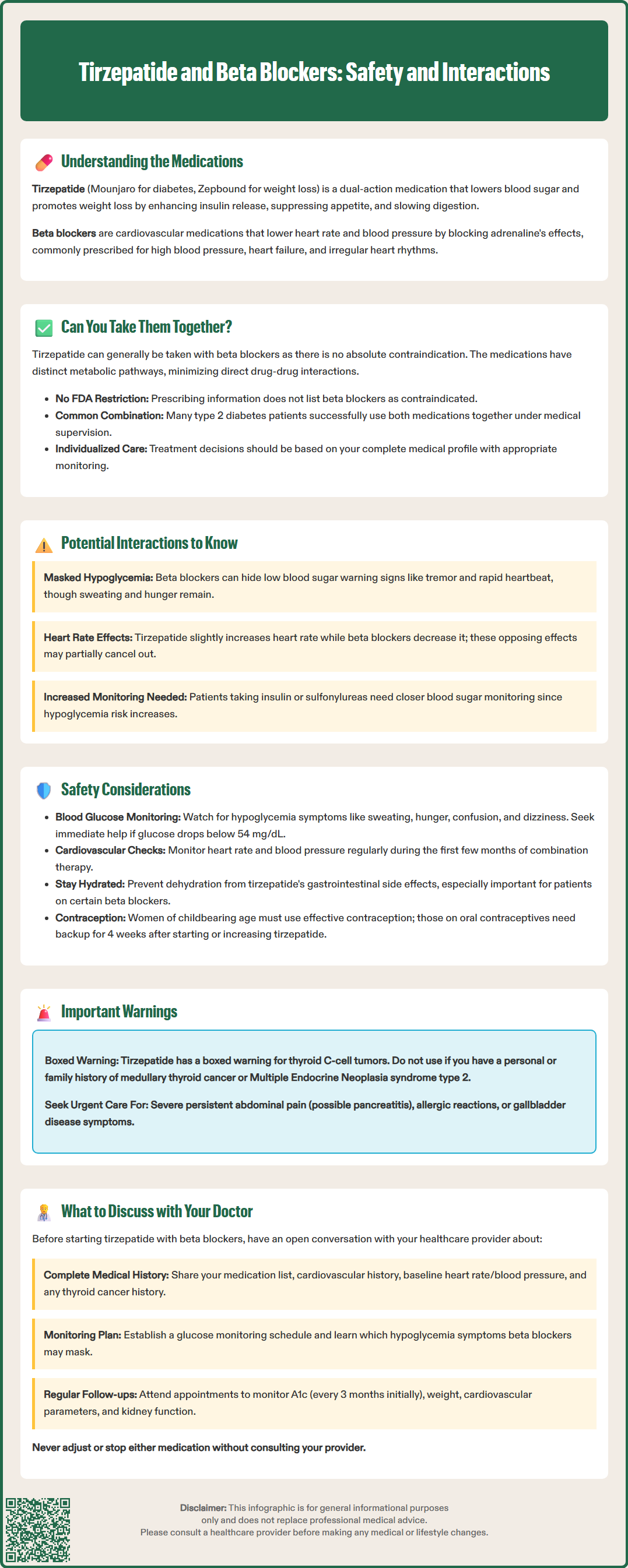
While tirzepatide and beta blockers do not have direct pharmacokinetic interactions, several pharmacodynamic considerations warrant clinical attention. The most clinically relevant concern involves the recognition and management of hypoglycemia. Beta blockers, particularly non-selective agents like propranolol, can mask certain warning symptoms of hypoglycemia such as tremor, palpitations, and tachycardia by blocking adrenergic responses. This masking effect may delay recognition of low blood glucose, though sweating and hunger typically remain intact as warning signs. Although tirzepatide carries a lower intrinsic risk of hypoglycemia compared to insulin or sulfonylureas when used as monotherapy, patients taking tirzepatide with concomitant insulin or insulin secretagogues may experience hypoglycemic episodes that could be more difficult to detect if beta blockers are also prescribed.
Cardiovascular effects represent another area of potential interaction. Tirzepatide commonly causes a modest increase in resting heart rate (average increase of 2-4 beats per minute in clinical trials), though the precise mechanism is not fully established. Beta blockers, conversely, reduce heart rate as part of their therapeutic mechanism. When used together, these opposing effects on heart rate may partially offset each other, though beta blockers typically predominate in their chronotropic effects. This interaction is generally not clinically problematic but may require monitoring, particularly during tirzepatide initiation or dose escalation.
Additionally, gastrointestinal effects of tirzepatide—including nausea, vomiting, and delayed gastric emptying—could theoretically affect the absorption of oral medications. While no clinically significant interactions with beta blockers have been reported, tirzepatide does have an important labeled interaction with oral contraceptives. The FDA prescribing information notes that tirzepatide can reduce the exposure to oral contraceptives, requiring the use of backup contraception for 4 weeks after initiation and after each dose escalation of tirzepatide.
Monitoring blood glucose is essential when initiating or adjusting doses of either tirzepatide or beta blockers in combination therapy. Patients should be educated about hypoglycemia symptoms that remain detectable despite beta blocker use, particularly sweating, hunger, confusion, and dizziness. Those taking insulin or sulfonylureas alongside tirzepatide and beta blockers require especially vigilant glucose monitoring, and dose reductions of insulin or insulin secretagogues are often necessary when starting tirzepatide to minimize hypoglycemia risk. The American Diabetes Association recommends individualized glycemic targets and emphasizes the importance of patient education regarding hypoglycemia recognition and management. Patients should seek immediate medical attention for severe hypoglycemia (glucose <54 mg/dL or requiring assistance).
Cardiovascular monitoring should include periodic assessment of heart rate and blood pressure, particularly during the first few months of combination therapy. While the heart rate increase associated with tirzepatide is generally modest and well-tolerated, patients with pre-existing arrhythmias or those taking beta blockers for rate control may require closer monitoring. Blood pressure should be assessed regularly, as both weight loss from tirzepatide and the antihypertensive effects of beta blockers may necessitate adjustments in blood pressure medications to avoid hypotension.
Renal function monitoring is important because both medication classes have considerations related to kidney function. While tirzepatide does not require dose adjustment for renal impairment, gastrointestinal side effects (nausea, vomiting, diarrhea) could potentially lead to dehydration and acute kidney injury, particularly in patients taking renally excreted beta blockers like atenolol. Patients should be counseled on maintaining adequate hydration and reporting persistent gastrointestinal symptoms promptly.
Patients should be aware of red-flag symptoms requiring urgent medical attention, including severe, persistent abdominal pain (with or without vomiting) which may suggest pancreatitis, signs of allergic reaction, or symptoms of gallbladder disease. Additionally, women of childbearing potential should be advised that tirzepatide may cause fetal harm and should use effective contraception during treatment. If using oral contraceptives, backup contraception is needed for 4 weeks after tirzepatide initiation and after each dose escalation.
Before starting tirzepatide while taking beta blockers, patients should provide their healthcare provider with a complete medication list, including all prescription medications, over-the-counter drugs, and supplements. Specific information about the type and dose of beta blocker is important, as different agents (selective vs. non-selective, lipophilic vs. hydrophilic) may have varying implications for combination therapy. Patients should discuss their cardiovascular history, including the indication for beta blocker therapy, any history of arrhythmias, heart failure status, and baseline heart rate and blood pressure measurements.
Patients should inform their provider about any personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2), as tirzepatide is contraindicated in these cases. Women should discuss pregnancy plans or current pregnancy, as tirzepatide is not recommended during pregnancy due to potential fetal harm. Women using oral contraceptives should be aware they'll need backup contraception for 4 weeks after starting tirzepatide and after each dose increase.
Key topics to address include hypoglycemia awareness and management strategies, particularly if taking insulin or sulfonylureas. Patients should understand which hypoglycemia symptoms may be masked by beta blockers and develop a plan for regular glucose monitoring. Discussion of target glucose ranges, frequency of self-monitoring, and circumstances requiring urgent medical attention is essential. Patients should know to seek immediate medical care for severe hypoglycemia (glucose <54 mg/dL or requiring assistance), persistent severe abdominal pain, or signs of allergic reaction.
Ongoing communication with healthcare providers should include reporting of side effects such as persistent nausea, vomiting, diarrhea, abdominal pain, or signs of dehydration. Patients should also report any episodes of hypoglycemia, changes in heart rate or blood pressure, unusual fatigue, dizziness, or shortness of breath. Regular follow-up appointments are necessary to monitor glycemic control (hemoglobin A1c typically every 3 months initially), weight changes, cardiovascular parameters, and renal function. Patients should never adjust or discontinue either medication without consulting their healthcare provider, as both tirzepatide and beta blockers require careful management to optimize therapeutic benefits while minimizing risks. Collaborative decision-making between patients and providers ensures safe and effective use of combination therapy tailored to individual clinical needs.
Beta blockers, especially non-selective agents, can mask certain hypoglycemia warning signs such as tremor, palpitations, and rapid heartbeat. However, other symptoms like sweating, hunger, confusion, and dizziness typically remain detectable, allowing patients to recognize low blood sugar.
Beta blocker dose adjustments are not routinely required when starting tirzepatide, though your healthcare provider may monitor your heart rate and blood pressure more closely. Any medication changes should be made only under medical supervision based on your individual response to combination therapy.
Regular monitoring should include blood glucose levels, heart rate, blood pressure, and kidney function. Patients should also watch for hypoglycemia symptoms, gastrointestinal side effects, signs of dehydration, and any cardiovascular symptoms like unusual fatigue or dizziness.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.