LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide and vitamin B3 (niacin) are medications that may both be relevant for patients managing metabolic conditions such as type 2 diabetes and cardiovascular risk factors. Tirzepatide, a dual GIP/GLP-1 receptor agonist approved by the FDA for diabetes management and chronic weight management, works by enhancing insulin secretion, suppressing glucagon, and reducing appetite. Niacin, at pharmacologic doses, has historically been used to modify lipid profiles, though current guidelines no longer routinely recommend it for cardiovascular risk reduction. While no direct drug interaction exists between these medications, their concurrent use requires careful consideration due to opposing effects on glucose metabolism and specific monitoring requirements.
Quick Answer: Tirzepatide and vitamin B3 (niacin) can be taken together as no direct drug interaction exists, but concurrent use requires enhanced glucose monitoring due to their opposing effects on blood sugar metabolism.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound) in adults with BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity. Administered as a once-weekly subcutaneous injection, tirzepatide works through dual incretin receptor activation to enhance insulin secretion in a glucose-dependent manner, suppress glucagon release, slow gastric emptying, and reduce appetite. Clinical trials have demonstrated substantial reductions in hemoglobin A1c (up to 2.5%) and body weight (approximately 15-22.5% depending on dose in the SURMOUNT-1 trial), making it a significant advancement in metabolic disease treatment.
Vitamin B3 exists in two primary forms: niacin (nicotinic acid) and niacinamide (nicotinamide). Only niacin, not niacinamide, affects lipid metabolism. At pharmacologic doses (typically 500–2000 mg daily), niacin has been used to modify lipid profiles, particularly raising high-density lipoprotein (HDL) cholesterol and lowering triglycerides and low-density lipoprotein (LDL) cholesterol. However, current American Diabetes Association (ADA) and American College of Cardiology/American Heart Association (ACC/AHA) guidelines no longer routinely recommend niacin for cardiovascular risk reduction due to lack of demonstrated outcome benefits and potential adverse effects. Niacin is available over-the-counter in lower doses as a dietary supplement and by prescription in higher-dose formulations for specific dyslipidemia management scenarios.
Both medications may be relevant for patients with metabolic syndrome, type 2 diabetes, or cardiovascular risk factors. Tirzepatide addresses glycemic control and weight reduction, while niacin may be considered in select cases for lipid abnormalities when first-line therapies are insufficient or contraindicated. Understanding each medication's mechanism, therapeutic role, and safety profile is essential before considering their concurrent use, as both can influence glucose metabolism and cardiovascular parameters through different pathways.
There is no direct drug-drug interaction between tirzepatide and vitamin B3 (niacin) documented in the FDA prescribing information for tirzepatide. However, the concurrent use of these medications requires careful clinical consideration due to their opposing effects on glucose metabolism.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2). These contraindications apply regardless of concurrent medications.
Patients with type 2 diabetes who are prescribed tirzepatide for glycemic control may also have dyslipidemia requiring lipid-modifying therapy. While statins remain first-line therapy for most patients according to ADA and ACC/AHA guidelines, some individuals may be taking niacin for specific indications such as severe hypertriglyceridemia or statin intolerance. The decision to use both medications simultaneously should be individualized based on the patient's overall metabolic profile, cardiovascular risk, and treatment goals.
Clinical context matters significantly. For patients taking low-dose niacin as a dietary supplement (typically 20–100 mg daily), the risk of metabolic interference is minimal. However, patients receiving pharmacologic doses of niacin (500 mg or higher) for lipid modification require closer monitoring due to niacin's known effects on insulin sensitivity and glucose homeostasis. It's important to note that "flush-free" niacin (inositol hexanicotinate) and niacinamide do not provide the lipid-modifying benefits of nicotinic acid.
Healthcare providers can prescribe both medications together when clinically indicated, but this combination necessitates enhanced glucose monitoring, particularly during niacin initiation or dose escalation. The ADA guidelines emphasize individualized treatment approaches that balance glycemic control with cardiovascular risk reduction, which may include careful use of multiple medications affecting different metabolic pathways.
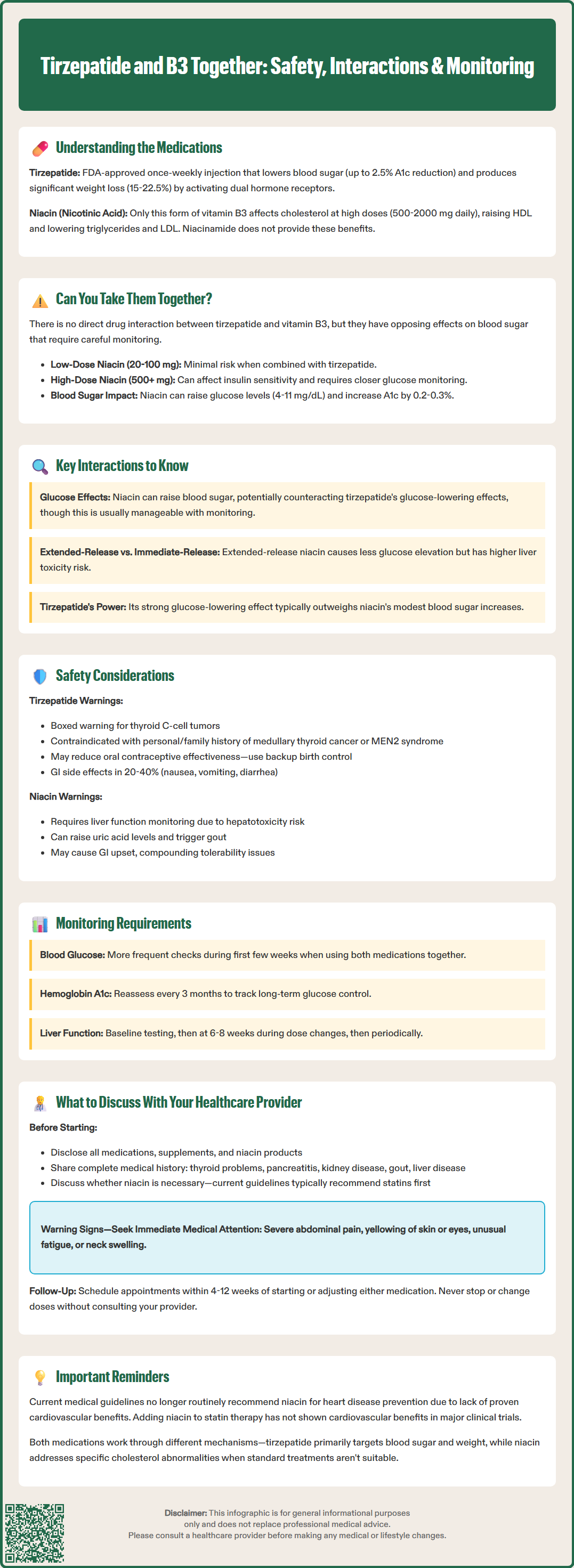
The primary concern when combining tirzepatide and niacin relates to their opposing effects on glucose metabolism rather than a direct pharmacokinetic interaction. Niacin, particularly at pharmacologic doses, can impair insulin sensitivity and increase hepatic glucose production, potentially raising blood glucose levels. This effect is dose-dependent and typically more pronounced with immediate-release formulations compared to extended-release preparations.
Studies have shown that niacin therapy can increase fasting glucose by approximately 4-11 mg/dL on average, with some patients experiencing more substantial elevations. In patients with diabetes, niacin may increase hemoglobin A1c by approximately 0.2–0.3% with standard doses. The mechanism involves increased insulin resistance at the cellular level and enhanced hepatic gluconeogenesis. For patients taking tirzepatide specifically to improve glycemic control, niacin's hyperglycemic effect could theoretically counteract some of tirzepatide's glucose-lowering benefits.
However, this interaction is generally manageable. Tirzepatide's potent glucose-lowering effects often outweigh niacin's modest hyperglycemic impact. Many patients can maintain adequate glycemic control on both medications with appropriate monitoring and dose adjustments. Extended-release niacin formulations may cause less glucose elevation than immediate-release products but carry a higher risk of hepatotoxicity.
It's important to note that while both medications can affect lipid parameters, large clinical trials (AIM-HIGH and HPS2-THRIVE) have not demonstrated cardiovascular outcome benefits from adding niacin to statin therapy. Therefore, the combination should not be used with the expectation of enhanced cardiovascular protection.
An additional consideration is tirzepatide's effect on gastric emptying, which may delay the absorption of oral medications. While this does not directly affect niacin, it can reduce the exposure of oral contraceptives, requiring additional contraceptive precautions during tirzepatide initiation and dose escalation. No other significant pharmacokinetic interactions affecting drug absorption, distribution, metabolism, or elimination have been identified between these agents.
When tirzepatide and niacin are used concurrently, several important safety considerations warrant attention:
Tirzepatide-specific safety concerns:
Boxed warning: Risk of thyroid C-cell tumors; patients should be counseled to report symptoms such as neck mass, dysphagia, or persistent hoarseness
Contraindication: Personal or family history of MTC or MEN2
Gallbladder disease: Tirzepatide may increase risk of gallstones and cholecystitis
Acute kidney injury: Dehydration from gastrointestinal adverse effects may impair renal function
Pancreatitis: Patients should be counseled to report severe, persistent abdominal pain
Niacin-specific safety concerns:
Hepatotoxicity: Baseline liver function tests and monitoring during dose titration and periodically thereafter are recommended; avoid in active liver disease
Hyperuricemia/gout: Niacin can raise uric acid levels; use cautiously in patients with gout
Myopathy risk: When combined with statins, increased risk of muscle symptoms requires monitoring
Glucose effects: Dose-dependent increases in blood glucose and A1c
Monitoring recommendations:
Glucose monitoring is paramount, particularly during the first few weeks after initiating or adjusting either medication. Patients should check blood glucose levels more frequently than usual, and healthcare providers should consider reassessing hemoglobin A1c within 3 months.
Liver function tests should be obtained at baseline, after 6-8 weeks during niacin dose titration, and periodically thereafter.
Renal function should be monitored, especially if patients experience significant gastrointestinal symptoms that could lead to dehydration.
Side effect management:
Common adverse effects of tirzepatide include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and decreased appetite, which occur in 20–40% of patients, particularly during dose escalation.
Niacin commonly causes flushing (occurring in up to 80% of patients with immediate-release formulations), pruritus, and gastrointestinal upset.
While these side effect profiles do not directly overlap, patients experiencing significant gastrointestinal symptoms from tirzepatide may find niacin's additional gastrointestinal effects poorly tolerated.
Pregnancy considerations: Tirzepatide is not recommended during pregnancy, and women of childbearing potential should be advised that tirzepatide may reduce the effectiveness of oral contraceptives, particularly during initiation and dose escalation. Additional contraceptive methods may be needed during these periods.
Before combining tirzepatide and vitamin B3, patients should have a comprehensive discussion with their healthcare provider covering several key topics. Full medication disclosure is essential—patients should inform their provider about all prescription medications, over-the-counter supplements, and the specific dose and formulation of any niacin products they are taking or considering.
Important discussion points include:
Medical history: Disclose any history of thyroid problems (especially MTC), MEN2, pancreatitis, gallbladder disease, kidney disease, gout, liver disease, or alcohol use
Treatment goals: Clarify whether niacin therapy is necessary given current lipid management guidelines, which generally favor statins, ezetimibe, PCSK9 inhibitors, or other agents before niacin for cardiovascular risk reduction
Glucose monitoring plan: Establish a clear schedule for blood glucose checks and hemoglobin A1c testing (typically every 3 months) to assess the combination's net effect on glycemic control
Liver monitoring plan: Discuss the schedule for liver function tests if taking pharmacologic doses of niacin (baseline, 6-8 weeks during titration, and periodically thereafter)
Pregnancy planning: If applicable, discuss contraception needs, as tirzepatide may reduce oral contraceptive effectiveness during initiation and dose escalation
Symptom management: Review strategies for managing potential side effects from both medications, including the timing of niacin doses to minimize flushing and approaches to mitigate tirzepatide's gastrointestinal effects
Patients should specifically ask about the expected timeline for therapeutic effects, warning signs that require immediate medical attention (severe abdominal pain, yellowing of skin/eyes, unusual fatigue, neck swelling), and whether any dose adjustments to existing diabetes medications may be necessary. Those taking niacin supplements without medical supervision should inform their provider, as even over-the-counter formulations can affect glucose metabolism at higher doses.
Regular follow-up appointments are crucial when using this combination. Providers typically recommend reassessment within 4–12 weeks of initiating or adjusting therapy to evaluate efficacy, tolerability, and metabolic parameters including glucose control and lipid profiles. Patients should never discontinue or adjust doses of either medication without consulting their healthcare provider, as abrupt changes could adversely affect metabolic control.
No direct drug-drug interaction exists between tirzepatide and vitamin B3 (niacin) according to FDA prescribing information. However, niacin can raise blood glucose levels, which may partially counteract tirzepatide's glucose-lowering effects, requiring enhanced monitoring.
Patients should increase blood glucose monitoring frequency, particularly during the first few weeks after initiating or adjusting either medication. Healthcare providers typically recommend hemoglobin A1c reassessment within 3 months and liver function tests at baseline and periodically if taking pharmacologic niacin doses.
Discuss any niacin supplementation with your healthcare provider before starting, as pharmacologic doses can affect glucose metabolism. Current guidelines generally favor statins and other lipid-lowering agents over niacin for cardiovascular risk reduction, making the clinical necessity of niacin an important consideration.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.