LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide blood pressure reduction has emerged as a notable secondary benefit of this dual GIP/GLP-1 receptor agonist, FDA-approved for type 2 diabetes and chronic weight management. Clinical trials demonstrate systolic blood pressure reductions of 5 to 10 mmHg and diastolic decreases of 2 to 5 mmHg across diverse patient populations. While these cardiovascular effects appear partially mediated by weight loss, additional mechanisms may contribute. Understanding tirzepatide's impact on blood pressure helps clinicians optimize cardiometabolic management, though the medication is not FDA-approved for hypertension treatment and should complement guideline-directed antihypertensive therapy.
Quick Answer: Tirzepatide reduces systolic blood pressure by 5 to 10 mmHg and diastolic blood pressure by 2 to 5 mmHg in clinical trials, though it is not FDA-approved for hypertension treatment.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. Beyond its primary metabolic effects, tirzepatide has demonstrated reductions in systolic and diastolic blood pressure across multiple clinical trials. These blood pressure improvements appear to be partially mediated by weight loss, though additional mechanisms may contribute.
In clinical studies, patients treated with tirzepatide experienced average systolic blood pressure reductions ranging from 5 to 10 mmHg compared to baseline, with some trials showing greater reductions at higher doses. Diastolic blood pressure typically decreased by 2 to 5 mmHg. These changes were observed within weeks to months of treatment initiation and were maintained throughout study durations of 40 to 104 weeks. Individuals with elevated baseline blood pressure readings generally experienced more pronounced reductions.
The observed blood pressure reductions may have clinical relevance. Epidemiologic data suggest that a sustained 5 mmHg reduction in systolic blood pressure correlates with approximately 10% lower risk of major cardiovascular events and 7% reduction in all-cause mortality, though it's important to note that cardiovascular outcome trials for tirzepatide are ongoing and definitive cardiovascular benefit has not yet been established. It's also important to emphasize that tirzepatide is not FDA-approved for the treatment of hypertension, and should not replace standard antihypertensive therapy.
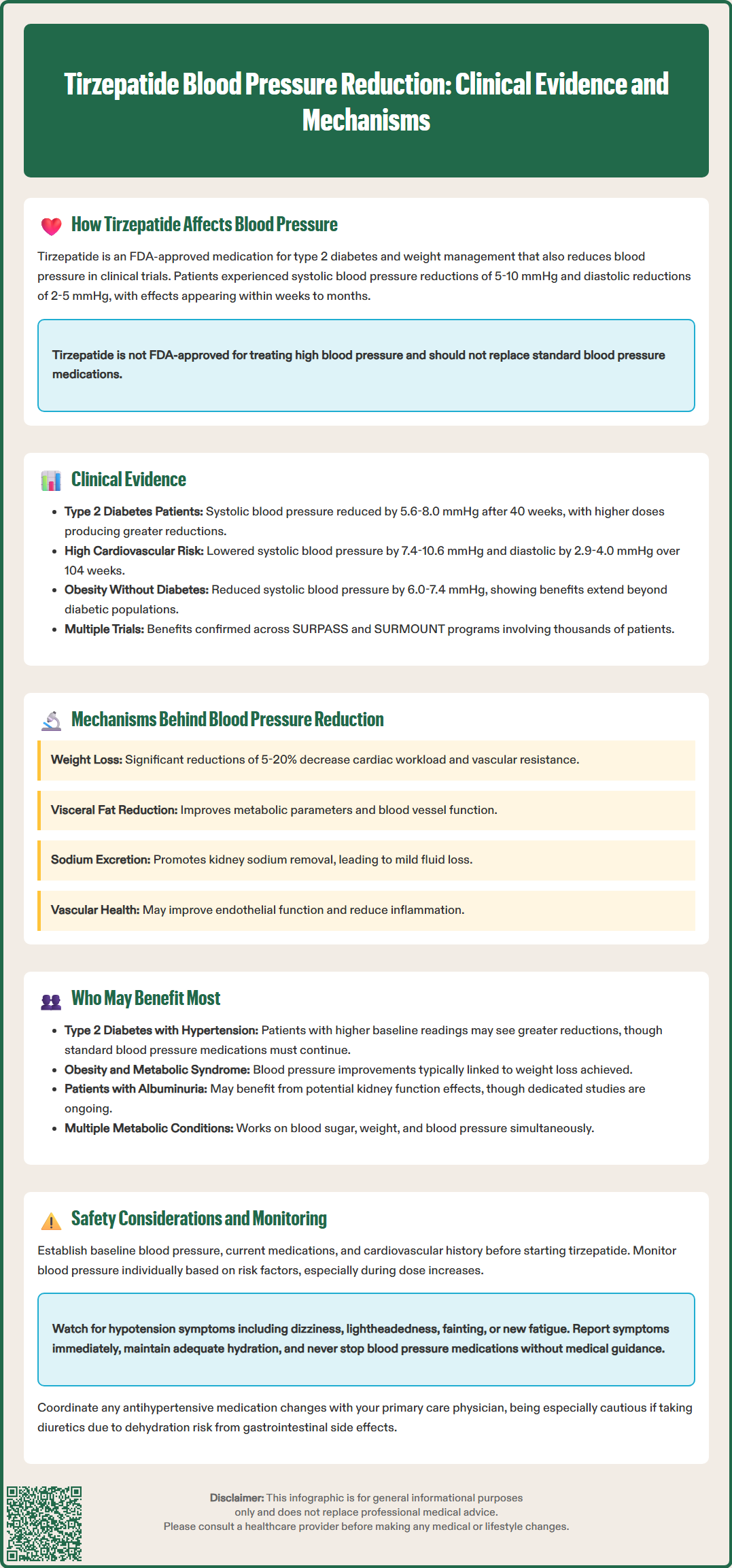
The SURPASS clinical trial program provides evidence for tirzepatide's blood pressure effects. In SURPASS-2, which compared tirzepatide to semaglutide 1 mg in 1,879 patients with type 2 diabetes, tirzepatide 5 mg, 10 mg, and 15 mg reduced systolic blood pressure from baseline by 5.6, 7.4, and 8.0 mmHg respectively at 40 weeks, compared to 5.3 mmHg with semaglutide. Notably, tirzepatide 5 mg produced greater weight loss than semaglutide 1 mg in this trial, which may contribute to blood pressure differences.
SURPASS-4, a cardiovascular safety study in 2,002 patients with type 2 diabetes and increased cardiovascular risk, demonstrated blood pressure changes over 104 weeks. Participants receiving tirzepatide experienced mean systolic blood pressure reductions from baseline of 7.4 to 10.6 mmHg across dosing tiers, with corresponding diastolic reductions of 2.9 to 4.0 mmHg. These effects were observed in patients receiving various background therapies, including antihypertensive medications.
The SURMOUNT trials, evaluating tirzepatide for weight management in individuals without diabetes, further documented blood pressure effects. SURMOUNT-1 enrolled 2,539 adults with obesity or overweight and demonstrated systolic blood pressure reductions from baseline of 6.0 to 7.4 mmHg at 72 weeks. Blood pressure improvements were observed across the study population, including those with elevated baseline readings. These findings suggest that tirzepatide's cardiovascular effects extend beyond the diabetic population to individuals with obesity or overweight.
Tirzepatide's blood pressure effects likely result from multiple mechanisms, with weight loss playing a central role. The medication's dual agonism of GIP and GLP-1 receptors triggers physiological changes that may collectively influence cardiovascular parameters, though many proposed mechanisms are based on GLP-1 receptor agonist class effects and require further confirmation specific to tirzepatide.
Weight reduction and adipose tissue changes represent primary contributors to blood pressure improvement. Tirzepatide induces substantial weight loss—typically 5-10% in type 2 diabetes and 15-20% in obesity without diabetes at therapeutic doses—which can directly reduce cardiac workload and peripheral vascular resistance. Tirzepatide promotes favorable changes in body composition, including visceral adipose tissue reduction, which may improve metabolic parameters that influence vascular function.
Natriuresis and volume effects may occur through GLP-1 receptor activation. Based on studies with other GLP-1 receptor agonists, these medications may enhance sodium excretion in renal tissues, potentially leading to mild diuresis. This effect could contribute to blood pressure reduction, though the specific impact of tirzepatide on renal sodium handling in humans requires further study.
Vascular function may also be affected. GLP-1 receptor activation has been associated with improved endothelial function in some studies. Tirzepatide, like other incretin-based therapies, may modestly increase heart rate (typically 2-4 beats per minute), which should be considered in overall cardiovascular assessment. Weight loss itself can reduce inflammatory markers and improve vascular function, which may contribute to blood pressure improvements observed with tirzepatide therapy.
Certain patient populations may experience blood pressure changes with tirzepatide therapy as part of its overall metabolic effects. Understanding these patterns helps contextualize blood pressure observations within comprehensive cardiometabolic management.
Patients with type 2 diabetes and hypertension represent a key population. Approximately two-thirds of individuals with type 2 diabetes have concurrent hypertension according to the American Diabetes Association, creating compounded cardiovascular risk. For these patients, tirzepatide addresses multiple metabolic parameters simultaneously—improving glycemic control, promoting weight loss, and potentially affecting blood pressure. Clinical trial data suggest that patients with elevated baseline blood pressure may experience more pronounced reductions, though individual responses vary. It's important to emphasize that tirzepatide is not indicated for hypertension treatment and should complement, not replace, guideline-directed antihypertensive therapy.
Individuals with obesity and metabolic syndrome without diabetes may also experience blood pressure changes. The SURMOUNT trials demonstrated that blood pressure effects occur in this population, with magnitude often correlating to degree of weight loss. For these individuals, tirzepatide may address multiple components of metabolic syndrome while supporting weight management goals.
Patients with albuminuria may warrant special consideration. While dedicated renal outcome trials for tirzepatide are not yet completed, post-hoc analyses from the SURPASS program suggest potential effects on urinary albumin excretion. Other GLP-1 receptor agonists have demonstrated renoprotective effects in dedicated outcome trials, though these findings cannot be automatically extrapolated to tirzepatide. Blood pressure effects may contribute to overall cardiorenal risk management in these patients, though standard nephroprotective therapies should be maintained according to current guidelines.
While tirzepatide's blood pressure effects are generally considered favorable, appropriate monitoring ensures safe implementation, particularly in individuals receiving concurrent antihypertensive therapy. Clinicians should establish individualized approaches to blood pressure assessment based on patient risk factors.
Baseline assessment should precede tirzepatide initiation. Document baseline blood pressure, current antihypertensive medications, and cardiovascular history. Patients taking multiple blood pressure medications, those with known cardiovascular disease, or elderly individuals may require more careful monitoring. The FDA prescribing information for tirzepatide does not mandate specific blood pressure monitoring protocols, but clinical judgment suggests appropriate assessment during dose titration.
Monitoring frequency should be individualized based on patient risk factors and concurrent medications. Home blood pressure monitoring may be valuable for patients on antihypertensive therapy, with clinical reassessment during dose escalation according to standard practice guidelines. Signs warranting clinical attention include:
Symptoms of hypotension (dizziness, lightheadedness, syncope)
Orthostatic blood pressure changes (per ACC/AHA guidelines)
New-onset fatigue or weakness suggesting hemodynamic changes
Antihypertensive medication adjustments should follow a patient-centered approach in coordination with the patient's primary care physician or specialist. Tirzepatide may cause gastrointestinal adverse effects that could lead to dehydration, potentially compounding hypotension risk, particularly in patients taking diuretics or renin-angiotensin system blockers.
Patient education is essential. Advise patients to report symptoms of hypotension promptly and maintain adequate hydration, particularly during hot weather or illness. Counsel regarding gradual position changes if orthostatic symptoms develop. Patients should understand that blood pressure changes may occur but that they should never independently discontinue prescribed antihypertensive medications. Remind patients of other important safety information from the FDA label, including the boxed warning regarding thyroid C-cell tumors and contraindications in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2.
No, tirzepatide is not FDA-approved for hypertension treatment and should not replace standard antihypertensive therapy. It may complement guideline-directed blood pressure management as part of comprehensive cardiometabolic care.
Blood pressure reductions with tirzepatide are typically observed within weeks to months of treatment initiation and are maintained throughout long-term therapy. Individual responses vary based on baseline blood pressure and degree of weight loss achieved.
Patients on concurrent antihypertensive medications should have individualized blood pressure monitoring, particularly during dose titration. Report symptoms of hypotension such as dizziness or lightheadedness to your healthcare provider promptly.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.