LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide side effects insomnia concerns arise as more patients use this dual GIP/GLP-1 receptor agonist for type 2 diabetes (Mounjaro) and weight management (Zepbound). While insomnia is not listed among common adverse reactions in FDA prescribing information or major clinical trials, some patients report sleep disturbances during treatment. Understanding whether tirzepatide directly causes sleep problems, potential indirect mechanisms, and management strategies helps patients and clinicians address these concerns effectively. This article examines the evidence on tirzepatide and sleep, explores possible contributing factors, and provides practical guidance for managing sleep quality during treatment.
Quick Answer: Insomnia is not listed as a common side effect of tirzepatide in FDA prescribing information or major clinical trials, though some patients report sleep disturbances that may be indirectly related to gastrointestinal symptoms or metabolic changes.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist available in the US under two brand names: Mounjaro (for type 2 diabetes in adults) and Zepbound (for chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity). This once-weekly injectable medication works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways.
According to FDA prescribing information, the most commonly reported side effects of tirzepatide are gastrointestinal in nature. For Mounjaro, these include nausea (12–29% of patients depending on dose), diarrhea (12–16%), vomiting (5–9%), constipation (6–7%), and abdominal pain or discomfort. Zepbound's profile includes similar GI effects plus additional reports of gastroesophageal reflux disease (GERD), eructation (belching), and dyspepsia. These effects typically emerge during dose initiation or escalation and often diminish over time as the body adjusts to the medication.
Other documented adverse effects include decreased appetite (which contributes to the therapeutic effect), fatigue, injection site reactions, dizziness, and modest increases in heart rate (typically 2-4 beats per minute). More serious but less common risks include pancreatitis, gallbladder disease, and acute kidney injury (usually secondary to dehydration from gastrointestinal symptoms). Hypoglycemia risk is low with tirzepatide monotherapy but increases when combined with insulin or sulfonylureas.
The FDA label carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies. Tirzepatide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Patients should report symptoms such as neck mass, difficulty swallowing, or persistent hoarseness.
Additionally, tirzepatide may delay gastric emptying, potentially reducing the absorption of oral medications including oral contraceptives. Women using oral contraceptives should consider additional contraceptive methods during tirzepatide initiation and dose escalation. Zepbound also carries a warning about monitoring for depression and suicidal thoughts.
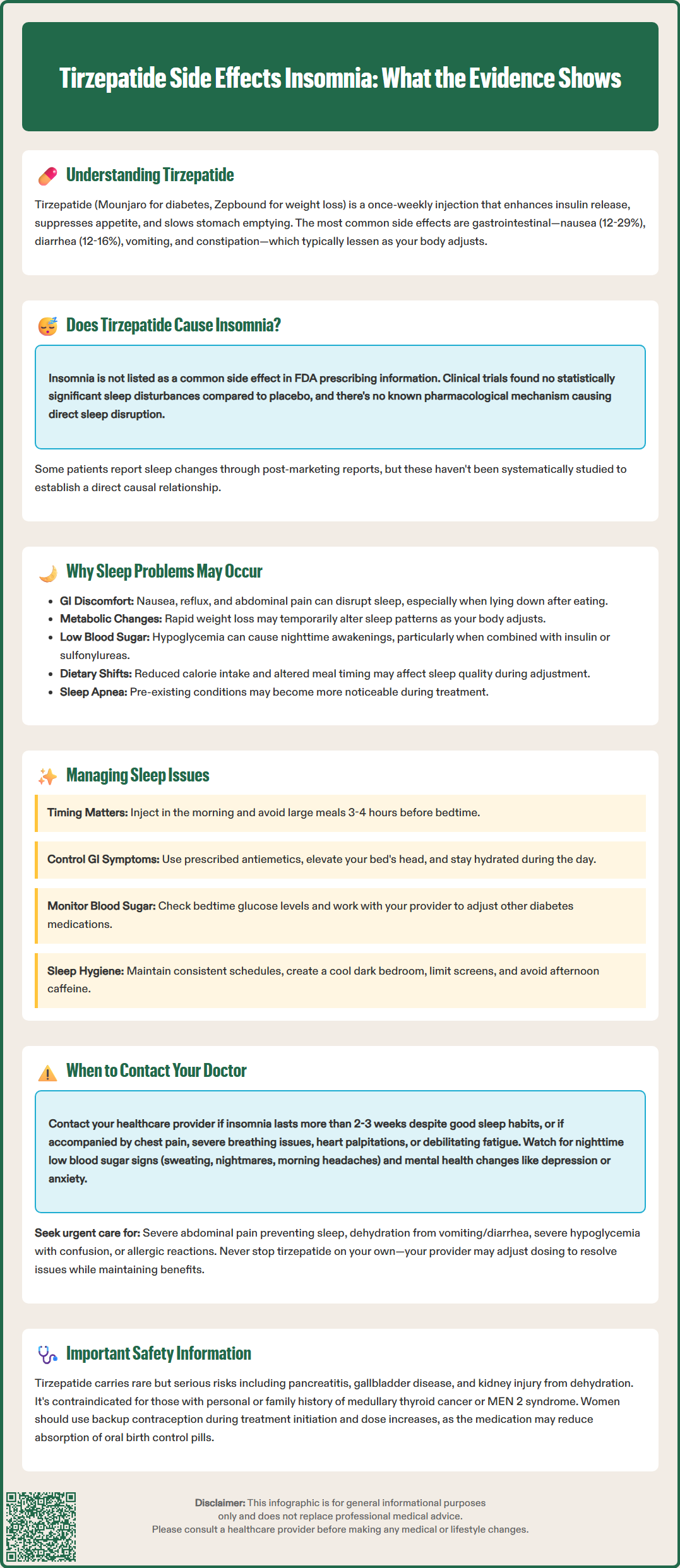
Insomnia and sleep disturbances are not listed among the common adverse reactions for tirzepatide in the FDA-approved prescribing information for either Mounjaro or Zepbound. In the SURPASS clinical trial program evaluating tirzepatide for type 2 diabetes and the SURMOUNT trials for weight management, insomnia was not identified as a statistically significant adverse event compared to placebo groups, based on published trial results.
This does not definitively establish that tirzepatide cannot affect sleep in some individuals, as clinical trials may not capture all potential effects, particularly those that occur at low frequencies or emerge during longer-term use. There is currently no established pharmacological mechanism by which tirzepatide would directly cause sleep disruption, though research in this specific area is limited.
Post-marketing surveillance through the FDA Adverse Event Reporting System (FAERS) and clinical experience suggest that some patients do report sleep changes after starting tirzepatide. However, these reports have not been systematically studied or quantified in controlled research to establish causality. Many factors can influence sleep quality during treatment with any medication, including pre-existing conditions, concurrent medications, and lifestyle factors.
The metabolic and physiological changes induced by tirzepatide may indirectly affect sleep patterns in some individuals. For example, gastrointestinal symptoms might disrupt sleep if they occur at night, or changes in eating patterns and weight loss could temporarily influence sleep architecture as the body adjusts.
Patients experiencing new or worsening sleep problems after initiating tirzepatide should discuss these symptoms with their healthcare provider. A thorough evaluation can help determine whether sleep disturbances might be related to the medication or if other factors such as obstructive sleep apnea, stress, caffeine intake, or other medications might be contributing.
Although tirzepatide has no established direct mechanism for causing insomnia, several indirect pathways may explain why some patients experience sleep disturbances during treatment. Understanding these potential factors can help address sleep issues more effectively.
Gastrointestinal symptoms represent a likely indirect cause of sleep disruption. Nausea, abdominal discomfort, or gastroesophageal reflux—all documented with tirzepatide—can interfere with sleep onset and maintenance. The medication's effect on slowing gastric emptying means food remains in the stomach longer, potentially causing discomfort when lying down, particularly if meals are consumed close to bedtime.
Metabolic and hormonal changes during weight loss may potentially affect sleep. Some research suggests that rapid weight reduction can temporarily influence sleep patterns as the body adjusts to new metabolic demands. While not specifically studied with tirzepatide, changes in appetite-regulating hormones that also influence sleep-wake regulation could hypothetically contribute to altered sleep quality during active weight loss phases.
Hypoglycemia, though uncommon with tirzepatide monotherapy, can cause nighttime awakenings, sweating, and restlessness if blood glucose drops too low during sleep. According to American Diabetes Association guidelines, this risk increases when tirzepatide is combined with insulin or sulfonylureas. Even mild nocturnal hypoglycemia may fragment sleep without causing full awakening or obvious symptoms. Continuous glucose monitoring or overnight glucose checks can help identify this potential cause.
Dietary changes and timing often accompany tirzepatide treatment. Reduced caloric intake, altered meal timing, or changes in macronutrient composition can affect sleep. Some patients may experience hunger-related sleep disruption as they adjust to decreased appetite and smaller portions.
Sleep apnea considerations: While weight loss typically improves obstructive sleep apnea (OSA), symptoms may persist despite weight reduction. Some patients might become more aware of pre-existing sleep apnea symptoms during treatment that were previously attributed to other causes.
Patients experiencing sleep disturbances while taking tirzepatide can implement several strategies to improve sleep quality without discontinuing beneficial therapy. A systematic approach addressing both medication-related factors and general sleep hygiene often yields the best results.
Consider injection timing and meal scheduling. Since tirzepatide is administered once weekly, some patients anecdotally report that morning administration (rather than evening) may help minimize any potential sleep interference, though this has not been formally studied. More importantly, avoid large meals within 3–4 hours of bedtime to minimize gastric discomfort and reflux symptoms. Smaller, low-fat meals throughout the day may reduce nighttime gastrointestinal symptoms.
Address gastrointestinal side effects proactively. Work with your healthcare provider to manage nausea and other GI symptoms that may interfere with sleep. This may include:
Taking prescribed antiemetics if recommended by your provider for significant nausea
Elevating the head of the bed if reflux symptoms occur
Avoiding trigger foods that worsen GI symptoms
Ensuring adequate hydration throughout the day (but limiting fluids close to bedtime)
Discussing temporary dose reduction or slower titration if GI symptoms are severe
Monitor and prevent hypoglycemia. If you take tirzepatide with insulin or sulfonylureas, work with your provider to adjust doses appropriately. Check bedtime blood glucose levels if nocturnal hypoglycemia is suspected. A small, balanced snack before bed may help stabilize overnight glucose levels, but only if specifically recommended by your healthcare team based on documented low glucose patterns.
Implement evidence-based sleep hygiene practices:
Maintain consistent sleep and wake times, even on weekends
Create a cool, dark, quiet sleep environment
Limit screen time for 1–2 hours before bed
Avoid caffeine after early afternoon and limit alcohol consumption
Engage in regular physical activity, but not within 3 hours of bedtime
Practice relaxation techniques such as deep breathing or progressive muscle relaxation
If sleep problems persist despite these interventions, discuss with your healthcare provider whether referral to a sleep specialist may be appropriate. For chronic insomnia, cognitive behavioral therapy for insomnia (CBT-I) is recommended as first-line treatment by the American Academy of Sleep Medicine, rather than long-term use of sleep medications.
While mild, transient sleep changes may not require immediate medical attention, certain patterns and associated symptoms warrant prompt communication with your healthcare provider. Distinguishing between self-manageable sleep disruption and situations requiring professional evaluation is essential for safe tirzepatide use.
Contact your provider if you experience:
Severe or persistent insomnia lasting more than 2–3 weeks despite implementing sleep hygiene measures
Sleep disruption accompanied by other concerning symptoms such as chest pain, severe shortness of breath, palpitations, or excessive daytime fatigue affecting daily function
Signs suggesting nocturnal hypoglycemia including nighttime sweating, nightmares, or morning headaches (overnight glucose monitoring may be recommended to confirm)
Significant mood changes including new or worsening depression, anxiety, irritability, or thoughts of self-harm (particularly important for patients taking Zepbound, which carries a warning about suicidality)
Symptoms suggesting sleep apnea such as loud snoring, witnessed breathing pauses, gasping during sleep, or excessive daytime sleepiness—these warrant evaluation even if you are losing weight
Thyroid-related symptoms including neck mass, difficulty swallowing, or persistent hoarseness (related to the boxed warning for tirzepatide)
Seek urgent medical attention for:
Severe abdominal pain that prevents sleep, which could indicate pancreatitis or gallbladder disease
Signs of dehydration from persistent vomiting or diarrhea, including decreased urination, dizziness, or confusion
Symptoms of severe hypoglycemia, including confusion, inability to wake fully, or loss of consciousness
Signs of allergic reaction such as facial/tongue swelling, difficulty breathing, severe rash, or hives
Your healthcare provider can assess whether sleep disturbances are related to tirzepatide, require dose adjustment, or reflect an unrelated condition requiring separate treatment. In some cases, temporary dose reduction or slower titration may resolve sleep issues while maintaining therapeutic benefits. Never discontinue tirzepatide without medical guidance, as abrupt cessation may affect diabetes control or weight management progress.
Insomnia is not listed among common adverse reactions in FDA prescribing information for Mounjaro or Zepbound, and clinical trials did not identify it as a statistically significant side effect. However, some patients report sleep disturbances that may be indirectly related to gastrointestinal symptoms or metabolic changes during treatment.
Implement sleep hygiene practices, avoid large meals within 3-4 hours of bedtime, and address gastrointestinal symptoms with your healthcare provider. If sleep problems persist for more than 2-3 weeks or are accompanied by concerning symptoms, contact your provider for evaluation and potential treatment adjustments.
Hypoglycemia risk with tirzepatide monotherapy is low, but increases when combined with insulin or sulfonylureas. Nocturnal hypoglycemia can cause nighttime awakenings, sweating, and restlessness, so patients on combination therapy should monitor bedtime glucose levels if sleep disruption occurs.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.