LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide, marketed as Mounjaro for type 2 diabetes and Zepbound for weight management, is a dual GIP and GLP-1 receptor agonist that has transformed metabolic disease treatment. As more patients begin this once-weekly injectable medication, questions arise about potential side effects, including whether tirzepatide causes nightmares. While gastrointestinal effects like nausea and diarrhea are well-documented, nightmares are not listed among recognized adverse reactions in FDA prescribing information or clinical trial data. Understanding the medication's actual side effect profile helps patients and clinicians distinguish between established risks and coincidental symptoms.
Quick Answer: Nightmares are not a recognized or documented side effect of tirzepatide according to FDA prescribing information and clinical trial data.
Tirzepatide is a prescription medication approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management in adults. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight loss), tirzepatide represents a novel class of medications known as dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonists.
For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m² (obesity) or ≥27 kg/m² (overweight) with at least one weight-related comorbidity. Tirzepatide is not indicated for patients with type 1 diabetes.
The medication works through a unique dual mechanism of action. By activating both GIP and GLP-1 receptors, tirzepatide enhances insulin secretion when blood glucose levels are elevated, suppresses inappropriate glucagon release, slows gastric emptying, and reduces appetite through effects on brain centers that regulate food intake. This combined action results in improved glycemic control in patients with type 2 diabetes and significant weight reduction in both diabetic and non-diabetic individuals with obesity.
Tirzepatide is administered as a once-weekly subcutaneous injection, with doses typically starting at 2.5 mg and gradually increasing every 4 weeks to a maintenance dose ranging from 5 mg to 15 mg (with intermediate steps of 7.5 mg and 12.5 mg), depending on individual response and tolerability. The gradual dose escalation helps minimize gastrointestinal side effects, which are among the most common adverse reactions associated with this medication class.
Importantly, tirzepatide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Women using oral hormonal contraceptives should use a non-oral method or add a backup method of contraception for 4 weeks after initiating tirzepatide and for 4 weeks after each dose increase, as tirzepatide may reduce the effectiveness of oral contraceptives during these periods.
Clinical trials have demonstrated that tirzepatide produces substantial improvements in hemoglobin A1c levels and body weight compared to placebo and other diabetes medications. The SURPASS clinical trial program established its efficacy and safety profile in diverse patient populations with type 2 diabetes, while the SURMOUNT trials evaluated its effectiveness for weight management in individuals without diabetes.
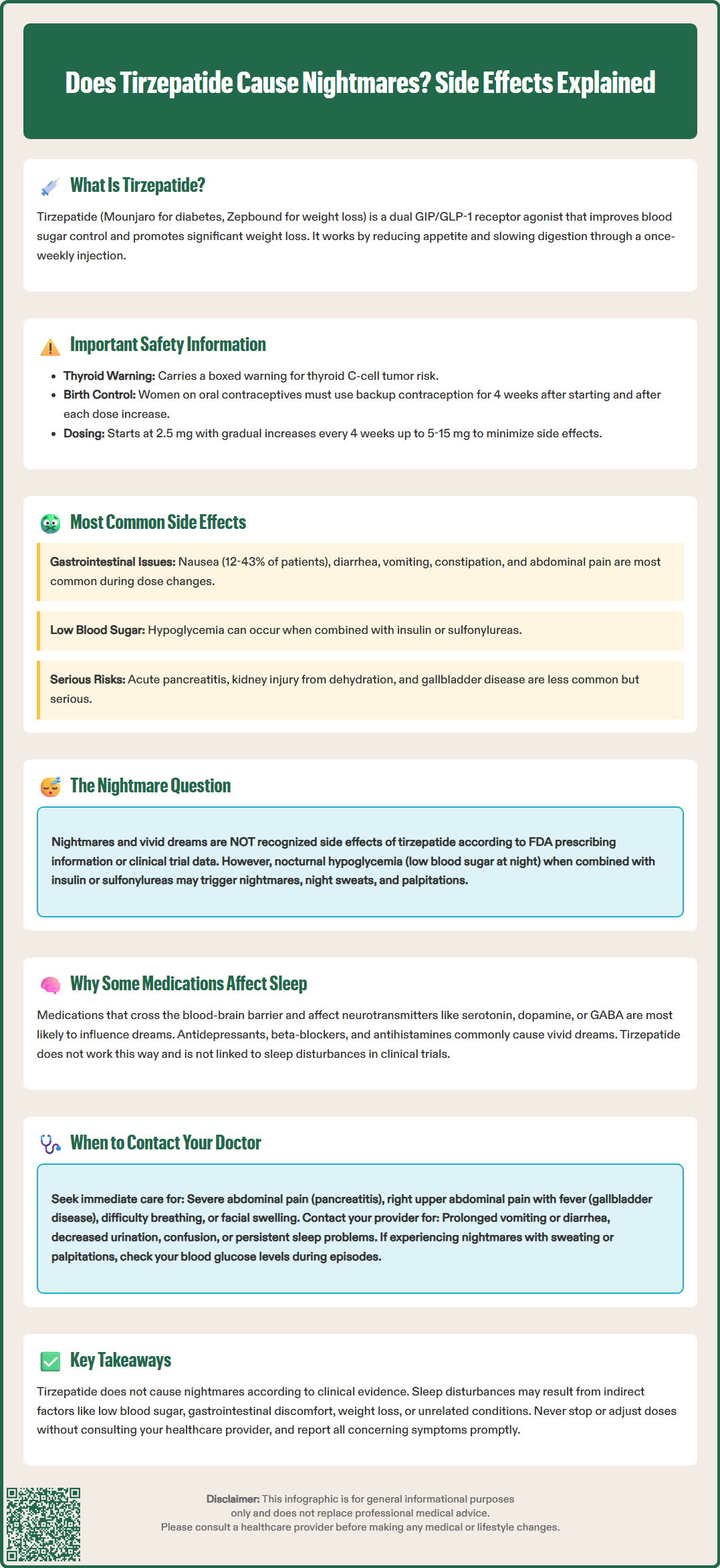
The most frequently reported side effects of tirzepatide are gastrointestinal in nature, consistent with the mechanism of action shared by GLP-1 receptor agonists. According to FDA prescribing information and clinical trial data, the most common adverse reactions include nausea, diarrhea, vomiting, constipation, abdominal pain, and decreased appetite. These gastrointestinal effects typically occur most prominently during dose initiation and escalation, and often diminish over time as the body adjusts to the medication.
In clinical trials for type 2 diabetes (SURPASS), nausea was reported by approximately 12-29% of patients receiving tirzepatide, depending on the dose, compared to 6-8% receiving placebo. Rates were generally higher in obesity trials (SURMOUNT), with nausea affecting up to 43% of patients at the highest doses. Diarrhea affected 13-16% of patients with diabetes and up to 30% in obesity trials, while vomiting occurred in 5-9% of those treated with tirzepatide for diabetes and up to 24% in obesity studies. These symptoms are generally mild to moderate in severity but can lead to treatment discontinuation in some patients, particularly at higher doses.
Other notable side effects include injection site reactions (redness, itching, or swelling at the injection site), fatigue, and hypoglycemia, particularly when tirzepatide is used in combination with insulin or sulfonylureas. Patients may also experience changes in heart rate, with an average increase in resting heart rate of approximately 2-4 beats per minute.
Tirzepatide carries warnings for several serious potential adverse effects, including acute pancreatitis, acute kidney injury (particularly from dehydration due to gastrointestinal effects), and acute gallbladder disease (including gallstones and cholecystitis). Caution is advised in patients with severe gastrointestinal disease, including gastroparesis.
Importantly, nightmares or vivid dreams are not listed among the common or recognized side effects of tirzepatide in the FDA-approved prescribing information. There is currently no established evidence from clinical trials linking tirzepatide to nightmare occurrence. Any sleep disturbances reported by patients taking tirzepatide may be coincidental or related to other factors such as dietary changes, weight loss, improved metabolic health, or concurrent medications.
Understanding why certain medications can influence sleep patterns and dream experiences requires knowledge of how drugs interact with the central nervous system and the complex neurobiology of sleep. Medications that directly cross the blood-brain barrier and interact with neurotransmitter systems—particularly those involving serotonin, norepinephrine, dopamine, acetylcholine, and gamma-aminobutyric acid (GABA)—are most likely to affect sleep architecture and dream content.
Medications known to cause vivid dreams or nightmares typically include certain antidepressants (particularly selective serotonin reuptake inhibitors and tricyclic antidepressants), beta-blockers used for cardiovascular conditions, some antihistamines, medications for Parkinson's disease, and certain antimalarial drugs. These medications can alter the normal progression through sleep stages, particularly affecting rapid eye movement (REM) sleep, the stage most associated with vivid dreaming. Some drugs suppress REM sleep initially, and when discontinued or when the body adapts, a "REM rebound" phenomenon can occur, leading to more intense or frequent dreams.
While tirzepatide is not associated with nightmares in FDA labeling or clinical trials, it's worth noting that nocturnal hypoglycemia can cause nightmares, night sweats, and sleep disturbances. This is particularly relevant when tirzepatide is used in combination with insulin or sulfonylureas. Patients experiencing nightmares accompanied by sweating, palpitations, or morning headaches should check their blood glucose levels during these episodes.
Indirect effects on sleep can occur with any medication that causes significant metabolic or physiological changes. Weight loss, improved glycemic control, changes in eating patterns, gastrointestinal discomfort, or anxiety about treatment could theoretically influence sleep quality. Additionally, underlying sleep disorders such as obstructive sleep apnea or gastroesophageal reflux disease (GERD) may affect sleep quality in patients taking tirzepatide.
Patients beginning tirzepatide may experience other life changes or stressors that coincidentally affect their sleep, making it important to consider the broader context of any reported sleep disturbances rather than automatically attributing them to the medication itself.
While tirzepatide is generally well-tolerated, certain side effects warrant prompt medical attention. Patients should contact their healthcare provider immediately if they experience severe or persistent abdominal pain, which could indicate pancreatitis—a rare but serious potential complication. Signs of pancreatitis include severe pain in the upper abdomen that may radiate to the back, often accompanied by nausea and vomiting. This condition requires urgent medical evaluation and typically necessitates discontinuation of the medication.
Patients should also seek immediate medical attention for signs of gallbladder disease, including pain in the right upper abdomen, fever, or yellowing of the skin or eyes (jaundice). Prolonged vomiting or diarrhea can lead to dehydration and acute kidney injury, requiring prompt evaluation and possibly intravenous fluids.
Other situations requiring prompt medical contact include signs of allergic reactions (difficulty breathing, swelling of the face or throat, severe rash)—call 911 for severe allergic reactions—symptoms of thyroid tumors (a lump or swelling in the neck, hoarseness, difficulty swallowing), or signs of kidney problems (decreased urination, swelling in legs or feet, unusual fatigue). Patients should also report symptoms of severe hypoglycemia, including confusion, severe dizziness, loss of consciousness, or seizures, particularly if taking tirzepatide with insulin or sulfonylureas.
Regarding sleep disturbances or nightmares specifically, while these are not recognized side effects of tirzepatide, patients experiencing significant sleep problems should discuss them with their healthcare provider. Persistent nightmares, severe insomnia, or other sleep disturbances can significantly impact quality of life and may indicate underlying issues requiring evaluation. Your provider can assess whether the sleep problems might be related to the medication, other health conditions, concurrent medications, or psychological factors, and can recommend appropriate management strategies.
Women using oral contraceptives should be aware that tirzepatide may reduce their effectiveness during dose initiation and escalation. Use a non-oral or backup method of contraception for 4 weeks after starting tirzepatide and for 4 weeks after each dose increase.
Patients who become pregnant while using Zepbound for weight management should discontinue the medication, as weight loss offers no potential benefit during pregnancy and may cause fetal harm.
Routine follow-up is essential for all patients taking tirzepatide. Healthcare providers typically monitor treatment response, adjust dosing as needed, assess for side effects, and conduct periodic laboratory testing to evaluate kidney function and glycemic control. Patients should never discontinue tirzepatide or adjust their dose without consulting their healthcare provider, as abrupt changes in diabetes management can lead to adverse outcomes.
Serious side effects should be reported to the FDA MedWatch program in addition to discussing them with your healthcare provider. Open communication about all symptoms and concerns enables comprehensive care and optimal treatment outcomes.
No, nightmares are not listed as a recognized side effect of tirzepatide in FDA prescribing information or clinical trial data. The most common side effects are gastrointestinal, including nausea, diarrhea, vomiting, and constipation.
While tirzepatide itself does not cause nightmares, nocturnal hypoglycemia (low blood sugar at night) can cause nightmares and sleep disturbances, particularly when tirzepatide is combined with insulin or sulfonylureas. Patients should monitor blood glucose levels if experiencing nightmares with sweating or palpitations.
Discuss persistent nightmares or sleep disturbances with your healthcare provider to identify potential causes, which may include nocturnal hypoglycemia, other medications, underlying sleep disorders, or unrelated factors. Your provider can assess whether adjustments to your treatment plan are needed.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.