LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Constipation is a common side effect of semaglutide (Ozempic, Wegovy, Rybelsus), affecting up to 24% of patients on weight management doses. This GLP-1 receptor agonist slows gastrointestinal transit and reduces appetite, leading to harder stools and decreased bowel frequency. Fortunately, most cases respond well to conservative interventions including increased hydration, dietary fiber, and physical activity. When lifestyle modifications prove insufficient, over-the-counter laxatives—particularly polyethylene glycol—offer safe, effective relief. Understanding how to treat constipation from semaglutide helps patients maintain treatment adherence while managing this predictable pharmacologic effect. This guide provides evidence-based strategies for prevention, management, and knowing when to seek medical evaluation.
Quick Answer: Semaglutide-induced constipation is typically managed with increased hydration, dietary fiber (25-38g daily), regular physical activity, and first-line use of polyethylene glycol 3350 when conservative measures are insufficient.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Ozempic, Rybelsus) and chronic weight management (Wegovy). While highly effective for glycemic control and weight reduction, gastrointestinal adverse effects are commonly reported, with constipation rates varying by indication and dosage—approximately 3-9% in diabetes treatment (Ozempic, Rybelsus) and up to 24% in weight management (Wegovy).
The mechanism underlying semaglutide-induced constipation relates directly to its pharmacologic action. GLP-1 receptors are distributed throughout the gastrointestinal tract, and semaglutide activation of these receptors significantly delays gastric emptying and slows intestinal transit time. This prolonged transit typically results in harder, drier stools that are more difficult to pass. Additionally, the appetite-suppressing effects of semaglutide often lead to reduced food and fluid intake, further contributing to constipation risk.
Constipation typically emerges during the initial titration phase or following dose escalation, though symptoms often improve with continued treatment. The severity ranges from mild infrequent bowel movements to significant discomfort requiring intervention. Understanding this mechanism is essential for both clinicians and patients, as it underscores that constipation is a predictable pharmacologic effect rather than an idiosyncratic reaction. This knowledge facilitates proactive management strategies and appropriate patient counseling before initiating therapy, potentially improving treatment adherence and overall tolerability.
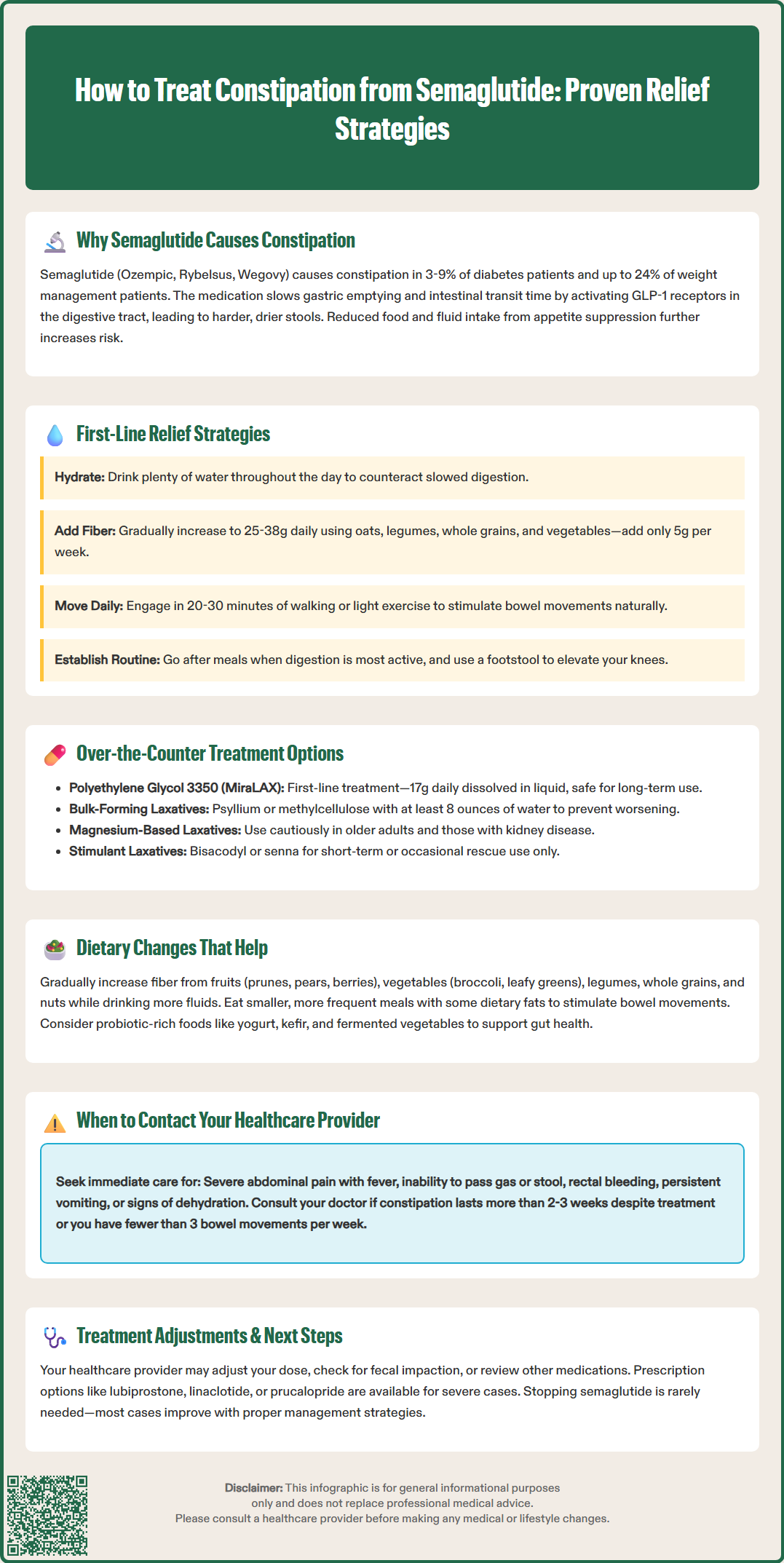
Initial management of semaglutide-related constipation should focus on conservative, non-pharmacologic interventions that address the underlying pathophysiology. These first-line strategies are safe, evidence-based, and often sufficient for mild to moderate symptoms.
Hydration optimization is paramount. Patients should maintain adequate fluid intake throughout the day, with increased consumption during physical activity or warm weather. Sufficient hydration helps counteract the effects of delayed transit time. Patients with heart failure, kidney disease, or other conditions requiring fluid restriction should follow their healthcare provider's specific guidance on fluid intake.
Increased dietary fiber intake represents another cornerstone intervention. Gradual incorporation of soluble fiber (oats, psyllium, legumes) and insoluble fiber (whole grains, vegetables, wheat bran) to achieve recommended daily intake (approximately 25g for women, 38g for men) can significantly improve stool consistency and frequency. Fiber supplementation must be introduced slowly—increasing by 5 grams weekly—to minimize bloating and gas, which may be particularly problematic given semaglutide's effects on gastric emptying.
Regular physical activity stimulates colonic motility through multiple mechanisms, including increased parasympathetic tone and direct mechanical stimulation. Even modest activity—such as 20–30 minutes of walking daily—can provide meaningful benefit. Patients should be encouraged to establish consistent exercise routines.
Bowel habit training involves responding promptly to defecation urges and establishing regular toilet times, ideally after meals when the gastrocolic reflex is strongest. Using a footstool to elevate the knees above the hips can help straighten the anorectal angle, reducing straining during defecation. These conservative measures should be implemented for 1–2 weeks before escalating to pharmacologic interventions, unless symptoms are severe or significantly impact quality of life.
When conservative measures prove insufficient, pharmacologic interventions may be necessary. A stepwise approach prioritizing safety and tolerability is recommended.
Osmotic laxatives, particularly polyethylene glycol 3350 (MiraLAX), are generally recommended as first-line pharmacologic therapy. These agents draw water into the intestinal lumen, softening stool and stimulating motility. Standard dosing is 17 grams (one capful) dissolved in 4–8 ounces of beverage daily, adjustable based on response. Polyethylene glycol is safe for extended use and does not cause electrolyte disturbances when used as directed.
Bulk-forming laxatives such as psyllium (Metamucil) or methylcellulose (Citrucel) increase stool mass and water content, promoting natural peristalsis. These should be taken with at least 8 ounces of water per dose. Adequate hydration is critical to prevent paradoxical worsening or bowel obstruction. These can be used as initial therapy, particularly in patients who tolerate increased fiber well.
Magnesium-based osmotic laxatives (magnesium hydroxide, magnesium citrate) should be used with caution, especially in older adults or those with kidney disease, due to potential for magnesium accumulation and electrolyte disturbances.
Stool softeners such as docusate sodium (Colace) have minimal evidence supporting their efficacy as monotherapy and are generally not recommended alone for semaglutide-induced constipation.
Stimulant laxatives including bisacodyl (Dulcolax) or senna are appropriate for short-term or rescue therapy. While concerns about long-term daily use exist primarily due to limited data rather than proven harm, these agents should ideally be used under healthcare provider guidance if needed regularly.
Prescription options for refractory cases include lubiprostone (Amitiza), linaclotide (Linzess), plecanatide (Trulance), and prucalopride (Motegrity). These medications work through distinct mechanisms to increase intestinal fluid secretion and accelerate transit. Referral to gastroenterology is appropriate when over-the-counter measures fail or if concerning features develop.
Comprehensive dietary and lifestyle modifications can significantly mitigate semaglutide-induced constipation while supporting the medication's therapeutic goals.
Fiber-rich food selection should emphasize variety and gradual introduction. Excellent sources include:
Fruits: Prunes, pears, apples with skin, berries, figs
Vegetables: Broccoli, Brussels sprouts, carrots, leafy greens
Legumes: Lentils, black beans, chickpeas
Whole grains: Oatmeal, quinoa, brown rice, whole wheat bread
Nuts and seeds: Almonds, chia seeds, flaxseeds
Patients should be counseled that while increasing fiber intake, they must simultaneously increase fluid consumption to prevent worsening constipation.
Meal timing and composition warrant attention. Smaller, more frequent meals may be better tolerated given semaglutide's effects on gastric emptying. Including some dietary fats may help stimulate the gastrocolic reflex. Probiotic-rich foods such as yogurt, kefir, and fermented vegetables may support gut health, though evidence specific to GLP-1-induced constipation remains limited.
Physical activity integration should be practical and sustainable. Beyond structured exercise, increasing daily movement through parking farther away, taking stairs, or brief walking breaks can accumulate meaningful activity. Gentle yoga or core exercises may provide additional benefit for some patients.
Stress management is often overlooked but relevant, as stress can exacerbate gastrointestinal symptoms through the gut-brain axis. Techniques such as deep breathing, meditation, or progressive muscle relaxation may provide adjunctive benefit.
Medication administration timing considerations vary by product. Oral semaglutide (Rybelsus) must be taken in the morning on an empty stomach with a small sip of water, following specific FDA instructions. For injectable semaglutide (Ozempic, Wegovy), administration can be timed according to patient preference, though consistency is recommended. Patients should not adjust their dosing schedule without consulting their healthcare provider.
While constipation from semaglutide is generally manageable with conservative interventions, certain clinical scenarios warrant prompt medical evaluation to exclude serious complications or alternative diagnoses.
Immediate medical attention is required for:
Severe abdominal pain, particularly if localized, progressively worsening, or accompanied by fever
Abdominal distension with inability to pass gas or stool, suggesting possible bowel obstruction
Rectal bleeding or black, tarry stools indicating potential gastrointestinal bleeding
Persistent nausea and vomiting preventing adequate oral intake
Signs of dehydration including decreased urination, dizziness, or confusion
Routine consultation is appropriate when:
Constipation persists beyond 2–3 weeks despite conservative measures and over-the-counter laxatives
Bowel movement frequency decreases to fewer than 3 per week
Significant straining or sensation of incomplete evacuation occurs regularly
New or worsening symptoms develop after previously stable bowel patterns
Quality of life is substantially impacted, affecting daily activities or treatment adherence
Unexplained weight loss, anemia, or new-onset constipation in older adults
Family history of colorectal cancer with new constipation symptoms
Healthcare providers should evaluate for potential complications such as fecal impaction, particularly in elderly patients or those with pre-existing motility disorders. Assessment should include medication review to identify other constipating agents, digital rectal examination when indicated, and consideration of abdominal imaging if obstruction is suspected.
Dose adjustment considerations: In some cases, delaying dose escalation or temporarily reverting to a previously tolerated dose may be necessary to improve tolerability while maintaining therapeutic benefit. Patients should not adjust their dose without healthcare provider guidance. Discontinuation is rarely required solely for constipation but may be appropriate if symptoms prove refractory to all interventions or if serious complications develop. Shared decision-making between patient and provider should weigh the medication's benefits against the burden of gastrointestinal adverse effects, exploring whether alternative GLP-1 receptor agonists or different therapeutic approaches might be better tolerated.
Constipation typically emerges during initial titration or after dose increases and often improves with continued treatment as the body adjusts. Most cases respond to conservative management within 1-2 weeks, though some patients may require ongoing interventions throughout therapy.
Polyethylene glycol 3350 (MiraLAX) is generally recommended as first-line pharmacologic therapy because it is safe for extended use, does not cause electrolyte disturbances when used as directed, and effectively softens stool by drawing water into the intestinal lumen.
Yes, proactive measures include establishing adequate hydration habits (8+ glasses daily), gradually increasing dietary fiber to recommended levels before starting treatment, maintaining regular physical activity, and establishing consistent bowel routines. These strategies can reduce constipation risk and severity.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.