LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Semaglutide and blood thinners are frequently prescribed together, particularly in patients with type 2 diabetes or obesity who also have cardiovascular conditions requiring anticoagulation. Semaglutide, a GLP-1 receptor agonist marketed as Ozempic, Wegovy, and Rybelsus, helps manage blood sugar and promotes weight loss. Blood thinners—including warfarin, apixaban, rivaroxaban, and antiplatelet agents like aspirin—prevent dangerous blood clots. Understanding how these medications interact and what safety precautions are necessary is essential for patients and healthcare providers managing complex medication regimens. This article examines the compatibility, potential interactions, and monitoring requirements for concurrent use of semaglutide and anticoagulant therapy.
Quick Answer: Semaglutide can generally be taken safely with blood thinners, as there are no direct contraindications or pharmacokinetic interactions documented in FDA prescribing information.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under brand names including Ozempic, Wegovy, and Rybelsus, semaglutide works by mimicking the action of the naturally occurring hormone GLP-1. This mechanism enhances glucose-dependent insulin secretion, suppresses inappropriate glucagon release, slows gastric emptying, and promotes satiety through central nervous system pathways.
Blood thinners, more accurately termed anticoagulants and antiplatelet agents, represent a diverse class of medications that reduce the blood's ability to form clots. Common anticoagulants include warfarin, apixaban (Eliquis), rivaroxaban (Xarelto), edoxaban (Savaysa), and dabigatran (Pradaxa), which work through various mechanisms to inhibit clotting factors. Antiplatelet medications such as aspirin and clopidogrel (Plavix) prevent platelets from aggregating. These medications are prescribed for conditions including atrial fibrillation, deep vein thrombosis, pulmonary embolism, and cardiovascular disease prevention. For mechanical heart valves, warfarin is the standard of care, as direct oral anticoagulants (DOACs) are not indicated for this purpose.
Many patients with type 2 diabetes or obesity also have cardiovascular comorbidities requiring anticoagulation therapy. According to the American Diabetes Association Standards of Care, cardiovascular disease remains the leading cause of morbidity and mortality in individuals with diabetes. Consequently, the concurrent use of semaglutide and blood thinners is increasingly common in clinical practice. Understanding the safety profile and potential interactions between these medication classes is essential for optimizing patient outcomes and minimizing adverse events.
Yes, semaglutide can generally be taken concurrently with blood thinners. There is no official contraindication or direct pharmacokinetic interaction documented in the FDA prescribing information for semaglutide that would prohibit its use with anticoagulant or antiplatelet medications. The drug is primarily metabolized through proteolytic degradation and does not undergo hepatic cytochrome P450 metabolism, which significantly reduces the potential for drug-drug interactions with medications metabolized through these pathways.
Clinical trials evaluating semaglutide safety and efficacy have included participants taking various cardiovascular medications, including anticoagulants and antiplatelet agents. The SUSTAIN and STEP trial programs, which established semaglutide's efficacy for diabetes management and weight loss respectively, did not identify specific safety concerns related to concomitant blood thinner use. The cardiovascular outcomes trial SUSTAIN-6, published in the New England Journal of Medicine, demonstrated cardiovascular safety in a population where many participants were receiving antiplatelet therapy.
However, the absence of a direct drug interaction does not eliminate all considerations for combined use. Healthcare providers must evaluate individual patient factors, including bleeding risk, renal function, and overall medication burden. For patients taking warfarin, more frequent INR monitoring is recommended during semaglutide initiation or dose changes, as a prudent clinical practice. Patients taking both medication classes require appropriate monitoring and should be educated about recognizing signs of bleeding complications. The decision to prescribe semaglutide to patients on anticoagulation therapy should be individualized, considering the therapeutic benefits against the patient's baseline bleeding risk and comorbidity profile. Close communication between prescribers, particularly when multiple specialists are involved in a patient's care, helps ensure safe medication management.
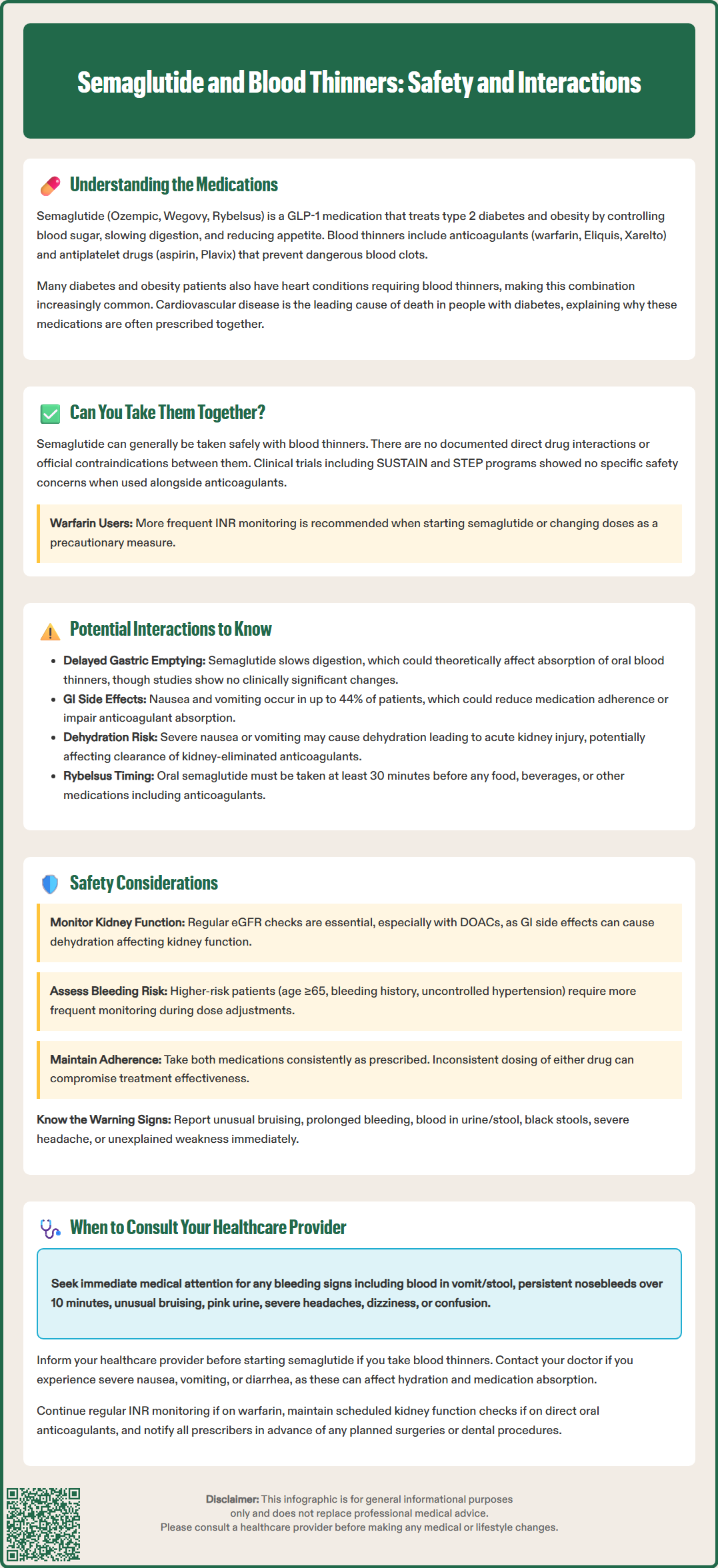
While semaglutide does not directly interact with the pharmacokinetics or pharmacodynamics of anticoagulant medications, several indirect considerations merit clinical attention. Semaglutide's effect on gastric emptying represents the most clinically relevant consideration. By delaying gastric emptying, semaglutide may theoretically affect the absorption rate of oral medications, including oral anticoagulants such as warfarin, apixaban, rivaroxaban, edoxaban, and dabigatran. However, clinical studies have not demonstrated clinically significant alterations in the bioavailability or therapeutic effect of these agents when co-administered with semaglutide.
For patients taking warfarin, which requires careful monitoring through international normalized ratio (INR) testing, the initiation of semaglutide warrants consideration of more frequent INR monitoring during the titration phase. Although direct interactions are not expected based on FDA labeling, any medication change in patients on warfarin justifies increased vigilance. Changes in dietary intake, weight loss, or gastrointestinal symptoms associated with semaglutide initiation could indirectly influence warfarin's anticoagulant effect through alterations in vitamin K intake or absorption.
For patients taking oral semaglutide (Rybelsus), specific administration timing is required. According to the FDA prescribing information, Rybelsus must be taken at least 30 minutes before the first food, beverage, or other oral medications of the day. This means patients taking oral anticoagulants should take Rybelsus first, wait at least 30 minutes, and then take their anticoagulant medication, ensuring any food requirements for the anticoagulant are also met (e.g., rivaroxaban 15/20 mg should be taken with food).
Semaglutide's gastrointestinal adverse effects, particularly nausea and vomiting, occur commonly during treatment initiation and dose escalation. According to the FDA prescribing information, gastrointestinal adverse reactions occur in up to 44% of patients taking Wegovy and at varying rates with Ozempic and Rybelsus depending on dose. These symptoms could potentially affect anticoagulant therapy through reduced medication adherence, impaired absorption, or in severe cases, dehydration leading to acute kidney injury that could alter clearance of renally eliminated anticoagulants.
Patients receiving both semaglutide and anticoagulant therapy require comprehensive safety monitoring and patient education. Baseline assessment should include evaluation of renal function, particularly for direct oral anticoagulants (DOACs) which require dose adjustments in renal impairment. While semaglutide does not require dose adjustment based on renal function according to FDA labeling, patients with severe gastrointestinal adverse effects may experience dehydration that could impact renal function. Regular monitoring of estimated glomerular filtration rate (eGFR) is appropriate for patients on DOACs, with warfarin often preferred in severe renal impairment or end-stage renal disease depending on the indication.
Bleeding risk assessment should be performed before initiating either medication class. Tools such as the HAS-BLED score can help quantify bleeding risk in patients requiring anticoagulation. Factors that increase bleeding risk include advanced age (≥65 years), history of bleeding, uncontrolled hypertension, labile INR (for warfarin users), concomitant antiplatelet therapy, excessive alcohol use, and certain comorbidities. Patients with multiple risk factors require enhanced monitoring and may benefit from more frequent follow-up during semaglutide titration.
Patients should receive clear education about recognizing signs and symptoms of bleeding complications, including unusual bruising, prolonged bleeding from minor cuts, blood in urine or stool, black tarry stools, severe headache, or unexplained weakness. They should be instructed to report these symptoms immediately. Additionally, patients should be counseled about the importance of medication adherence for both semaglutide and their anticoagulant, as inconsistent dosing of either medication could affect therapeutic outcomes.
For patients taking oral semaglutide (Rybelsus), healthcare providers should provide explicit instructions about the timing of administration relative to oral anticoagulants. Rybelsus must be taken at least 30 minutes before other oral medications, with a small amount of water (no more than 4 ounces) and on an empty stomach. This timing requirement is essential to ensure proper absorption of both medications.
Patients taking semaglutide and blood thinners concurrently should maintain regular communication with their healthcare team and understand specific circumstances requiring immediate medical attention. Any signs of bleeding represent a medical concern warranting prompt evaluation. These include visible blood in vomit or stool, persistent nosebleeds lasting more than 10 minutes, unusual or excessive bruising, bleeding gums, pink or red urine, coughing up blood, severe or persistent headaches, dizziness, weakness, or confusion. For severe, uncontrolled bleeding, head injury while anticoagulated, signs of stroke, or syncope with bleeding, patients should call 911 or seek emergency care immediately.
Patients should contact their healthcare provider before starting semaglutide if they are taking anticoagulants, even if the prescribing physician is aware of their medication list. This conversation should include discussion of bleeding risk, monitoring requirements, and signs of complications. Similarly, if a patient on semaglutide is prescribed a new anticoagulant or antiplatelet medication, both prescribers should be informed to ensure coordinated care.
Severe gastrointestinal symptoms during semaglutide treatment, including persistent nausea, vomiting, or diarrhea, warrant medical consultation, particularly in anticoagulated patients. These symptoms could affect hydration status, nutritional intake, and medication absorption. Patients unable to maintain adequate oral intake or experiencing dehydration may require temporary medication adjustment or additional supportive care.
Routine follow-up appointments should be maintained as scheduled. For patients on warfarin, INR monitoring should continue per the prescribing physician's recommendations, with potential for increased frequency during semaglutide initiation or dose changes. Patients taking direct oral anticoagulants should attend scheduled appointments for renal function monitoring and medication review. Any planned surgical or dental procedures require advance notification to all prescribers, as both anticoagulant and semaglutide management may need adjustment perioperatively. Current guidelines recommend specific approaches to perioperative management of both GLP-1 receptor agonists and anticoagulants. Establishing clear communication channels and understanding when to seek medical advice helps ensure safe concurrent use of these important medication classes.
Yes, semaglutide can be taken with warfarin, though more frequent INR monitoring is recommended during semaglutide initiation or dose changes. There are no direct drug interactions, but changes in diet, weight, or gastrointestinal symptoms may indirectly affect warfarin's anticoagulant effect.
Semaglutide does not directly alter the pharmacokinetics or pharmacodynamics of anticoagulants. However, its effect on delaying gastric emptying could theoretically affect absorption rates of oral anticoagulants, though clinical studies have not demonstrated significant alterations in therapeutic effect.
Watch for unusual bruising, blood in urine or stool, black tarry stools, prolonged bleeding from cuts, persistent nosebleeds, bleeding gums, severe headaches, or unexplained weakness. Report these symptoms to your healthcare provider immediately, and seek emergency care for severe uncontrolled bleeding or signs of stroke.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.