LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
What helps nausea from GLP-1 medications is a common concern for patients starting semaglutide, liraglutide, dulaglutide, or tirzepatide for type 2 diabetes or weight management. Nausea affects 15-44% of patients, particularly during initial treatment or dose increases. Fortunately, proven strategies including gradual dose titration, dietary modifications, eating smaller meals, and staying well-hydrated can significantly reduce this side effect. Understanding why GLP-1 medications cause nausea—primarily through delayed gastric emptying—helps patients implement targeted management approaches. This guide provides evidence-based recommendations to minimize nausea while maintaining the therapeutic benefits of GLP-1 therapy.
Quick Answer: Gradual dose titration, eating smaller frequent meals, avoiding high-fat foods, staying hydrated, and using antiemetics like vitamin B6 or ondansetron help reduce nausea from GLP-1 medications.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (Ozempic, Wegovy, Rybelsus), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity), along with tirzepatide (Mounjaro, Zepbound)—a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist—are effective medications for type 2 diabetes and weight management. However, nausea is the most commonly reported adverse effect, with incidence varying by medication and dose: approximately 15-30% for most GLP-1 agonists and up to 30-44% at higher doses of semaglutide and tirzepatide according to FDA prescribing information.
The mechanism behind this nausea involves several physiological pathways. These medications slow gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed emptying creates a sensation of fullness that contributes to weight loss but can also trigger nausea, particularly when the stomach remains distended. Additionally, GLP-1 receptors in the brainstem's area postrema, a region involved in detecting toxins and triggering the vomiting reflex, may contribute to nausea when activated.
Nausea typically occurs during the first 4-8 weeks of treatment or following dose increases, with many patients experiencing gradual improvement as their body adjusts to the medication. The severity varies considerably between individuals and is generally dose-dependent—higher doses tend to produce more pronounced gastrointestinal effects. While nausea is common and expected, it does not necessarily indicate the medication is working better; some patients achieve excellent results with minimal side effects, while persistent or severe symptoms may indicate a need for dose adjustment.
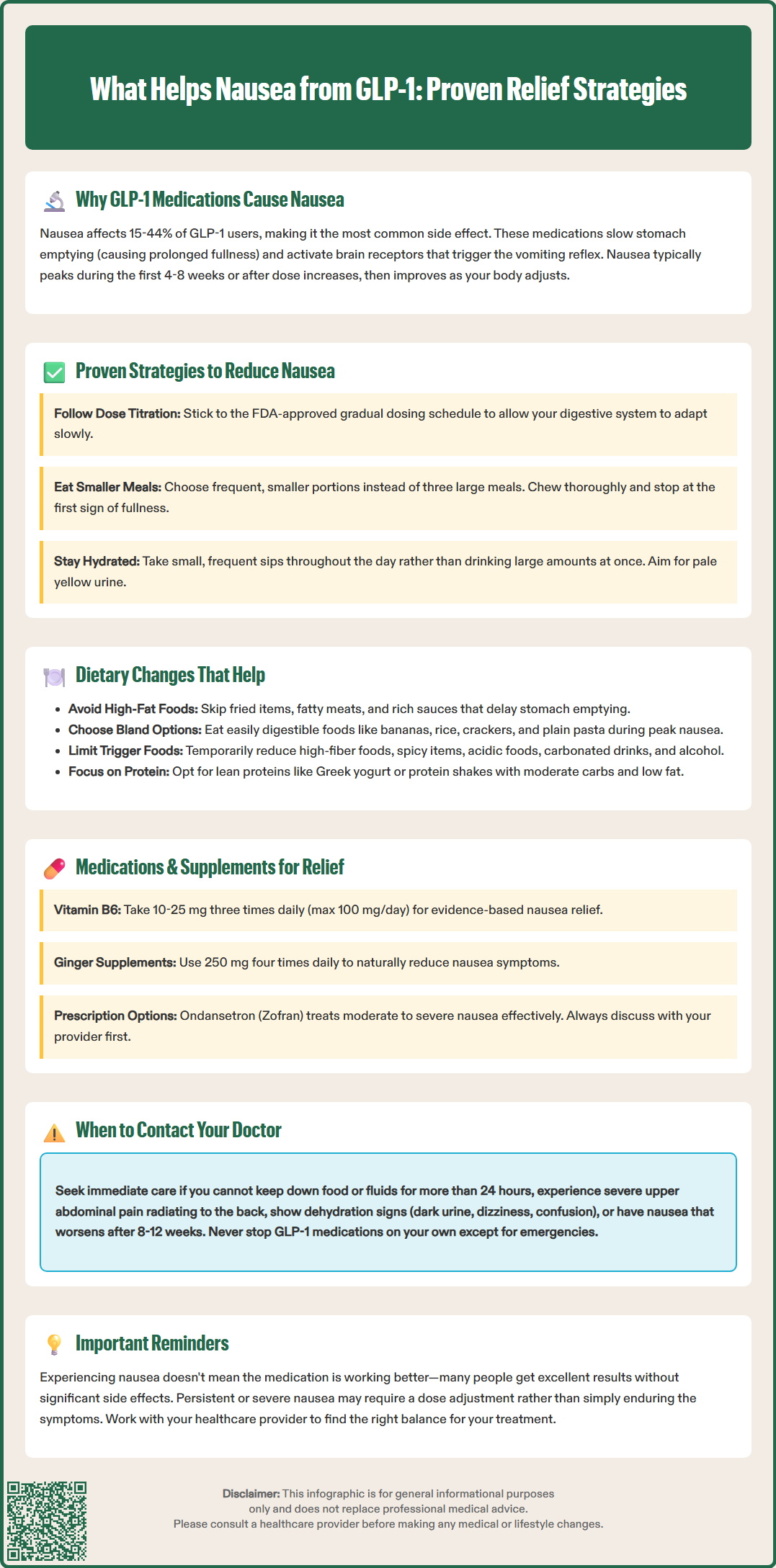
Clinical experience and patient reports have identified several evidence-based strategies that significantly reduce GLP-1-related nausea. Gradual dose titration remains the most effective preventive approach. The FDA-approved prescribing information for all GLP-1 medications includes specific titration schedules designed to minimize gastrointestinal side effects. Following these schedules allows the gastrointestinal system to adapt progressively. If you miss a dose, follow the specific instructions in your medication's prescribing information rather than attempting to catch up with multiple doses.
Injection timing and technique may influence symptom management for some patients. While GLP-1 medications can be administered at any time of day (consistent with prescribing information), some patients report personal preference for evening administration. For weekly medications, the timing has less impact on side effects due to their steady-state pharmacokinetics. Rotating injection sites (abdomen, thigh, upper arm) as recommended prevents injection site reactions but has not been proven to affect nausea specifically.
Eating patterns require modification during GLP-1 therapy. Consuming smaller, more frequent meals rather than three large meals prevents excessive stomach distension. Eating slowly and chewing thoroughly gives the delayed gastric emptying time to signal satiety before overeating occurs. Stopping eating at the first sign of fullness is essential, as these medications amplify the consequences of overeating.
Hydration status significantly impacts nausea severity. Maintain adequate fluid intake throughout the day, taking small, frequent sips rather than large volumes at once. Aim for pale yellow urine as an indicator of proper hydration. Dehydration exacerbates nausea and can lead to more serious complications. Cold or room-temperature beverages are generally better tolerated than hot liquids during symptomatic periods.
Specific dietary modifications can substantially reduce GLP-1-associated nausea. Avoiding high-fat foods is particularly important, as dietary fat further delays gastric emptying beyond the medication's effect. Fried foods, fatty meats, full-fat dairy products, and rich sauces commonly trigger or worsen nausea. Patients should emphasize lean proteins, such as skinless poultry, fish, eggs, and plant-based options like tofu or legumes.
Limiting high-fiber and gas-producing foods during symptomatic periods can provide relief. While fiber is generally healthful, excessive intake of cruciferous vegetables (broccoli, cabbage, Brussels sprouts), beans, and whole grains may increase bloating and nausea when gastric emptying is already delayed. Gradually reintroduce these foods as tolerance improves.
Bland, easily digestible foods are better tolerated during peak nausea. Bananas, rice, applesauce, and toast (the BRAT diet)—along with crackers, plain pasta, and boiled potatoes—can provide nutrition without overwhelming the digestive system. This approach is suitable for short-term symptom management but should not replace a balanced diet long-term. Ginger, either as fresh ginger tea, ginger ale (with real ginger), or ginger supplements (typically 250 mg four times daily), has demonstrated antiemetic properties in clinical studies for various types of nausea, though evidence specific to GLP-1 medications is limited.
Foods and beverages to avoid include:
Spicy or heavily seasoned dishes
Acidic foods (citrus, tomatoes) that may irritate the stomach
Carbonated beverages, which increase gastric distension
Alcohol, which can worsen nausea and interfere with blood glucose control
Very hot or very cold foods, which some patients report as triggers
Protein-forward meals with moderate carbohydrates and low fat content help maintain stable blood glucose levels while minimizing nausea. Small portions of Greek yogurt, cottage cheese, or protein shakes can provide nutrition when solid foods are poorly tolerated. Consider keeping a food diary to identify your personal trigger foods and avoid them during treatment.
While mild to moderate nausea is expected with GLP-1 therapy, certain symptoms warrant prompt medical evaluation. Persistent vomiting—defined as inability to keep down food or fluids for more than 24 hours—requires immediate contact with your healthcare provider. Prolonged vomiting can lead to dehydration, electrolyte imbalances, and acute kidney injury, complications documented in post-marketing surveillance of GLP-1 medications.
Signs of dehydration include dark urine, decreased urination, dizziness upon standing, dry mouth, extreme thirst, and confusion. These symptoms indicate the need for urgent assessment and possible intravenous fluid replacement. Patients with diabetes face additional risk, as dehydration can precipitate diabetic ketoacidosis in susceptible individuals.
Severe or worsening abdominal pain, particularly if localized to the upper abdomen and radiating to the back, may indicate pancreatitis—a rare but serious adverse effect included in the Warnings and Precautions section of GLP-1 medication labels. If pancreatitis is suspected, immediately discontinue the medication and seek emergency evaluation. Pancreatitis typically presents with intense, persistent pain accompanied by nausea and vomiting.
Other concerning symptoms that necessitate medical consultation include:
Severe abdominal distension or inability to pass gas/stool (possible ileus or bowel obstruction)
Nausea that worsens rather than improves after 8–12 weeks
Inability to maintain adequate nutrition or hydration
Unintentional weight loss exceeding clinical targets
New or worsening heartburn or reflux symptoms
Visual changes (especially with rapid blood sugar improvement)
Severe headache or altered mental status
Signs of gallbladder disease (right upper quadrant pain, especially after eating)
Hypoglycemia symptoms if taking insulin or sulfonylureas
Patients should generally not discontinue GLP-1 medications without medical guidance, except in emergencies such as suspected pancreatitis or severe allergic reaction. Your healthcare provider can adjust the dose, slow the titration schedule, or consider alternative management strategies. Temporary dose reduction often allows symptom resolution while maintaining therapeutic benefit.
Several pharmacological options can help manage GLP-1-induced nausea when lifestyle modifications prove insufficient. Over-the-counter antiemetics provide first-line symptomatic relief for many patients. Vitamin B6 (pyridoxine), typically 10–25 mg three times daily, has demonstrated antiemetic efficacy in clinical studies, particularly for pregnancy-related nausea. Do not exceed 100 mg total daily dose, as higher amounts may cause nerve damage with prolonged use. Ginger supplements (250 mg four times daily) offer a natural alternative with moderate evidence supporting their antiemetic properties, though patients on blood thinners should consult their provider before use.
Prescription antiemetics may be appropriate for moderate to severe nausea. Ondansetron (Zofran), a 5-HT3 receptor antagonist, effectively reduces nausea and is commonly prescribed off-label for GLP-1 side effects. Typical dosing is 4–8 mg every 8 hours as needed. Be aware that ondansetron can cause constipation and, rarely, QT interval prolongation (especially with electrolyte abnormalities). Metoclopramide (Reglan) works by promoting gastric emptying, theoretically counteracting the GLP-1 mechanism, but carries a boxed warning for tardive dyskinesia and should not be used for longer than 12 weeks except in rare circumstances. Prochlorperazine (Compazine) and promethazine (Phenergan) are alternative options but may cause significant sedation and anticholinergic effects; avoid driving or operating machinery while taking these medications.
Proton pump inhibitors (PPIs) such as omeprazole or pantoprazole may help patients experiencing concurrent reflux symptoms, as delayed gastric emptying can worsen gastroesophageal reflux disease. H2 blockers like famotidine are alternatives for milder reflux symptoms. However, neither directly addresses nausea and should not be used routinely without specific indication.
Important considerations include potential drug interactions and the risk of masking serious complications. Antiemetics should not be used to enable continued overeating or to suppress symptoms that might indicate pancreatitis or other serious adverse effects. Patients should discuss any additional medications or supplements with their healthcare provider before starting them, as some interactions may affect diabetes control or medication absorption.
There is no definitive evidence supporting probiotics, digestive enzymes, or most other supplements specifically for GLP-1 nausea, though individual patients may report subjective benefit. Any supplement use should be disclosed to healthcare providers to ensure comprehensive medication review and safety monitoring.
Nausea from GLP-1 medications typically occurs during the first 4-8 weeks of treatment or following dose increases, with gradual improvement as the body adjusts. Most patients experience significant reduction in symptoms within 8-12 weeks, though individual experiences vary.
Yes, over-the-counter options like vitamin B6 (10-25 mg three times daily) and ginger supplements can help manage GLP-1 nausea. However, discuss any medications or supplements with your healthcare provider to ensure safety and avoid interactions with your diabetes medications.
Contact your doctor immediately if you cannot keep down food or fluids for more than 24 hours, show signs of dehydration (dark urine, dizziness, confusion), experience severe abdominal pain, or have nausea that worsens rather than improves after 8-12 weeks of treatment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.